Abstract
Current insomnia treatments such as γ-aminobutyric acid (GABA) receptor modulators are associated with sedative and muscle-relaxant effects, which increase when drug intake is combined with alcohol. This study compared the novel sleep-enabling compound almorexant (ACT-078573-hydrochloride), a dual orexin receptor antagonist, with the positive GABAA-α1 receptor modulator zolpidem. Both compounds were administered alone or in combination with ethanol, and their effects on forced motor performance were determined in Wistar rats upon waking after treatment. To detect substance-induced sedation and myorelaxation, time spent on an accelerating rotating rod (rotarod) and forepaw grip strength were measured. Zolpidem (10, 30, and 100 mg/kg, p.o.) and ethanol (0.32, 1, and 1.5 g/kg, i.p.) dose-dependently decreased rotarod performance and grip strength, whereas almorexant (30, 100, and 300 mg/kg, p.o.) did not. Doses of ethanol (0.32 and 1 g/kg), which were ineffective when administered alone, showed interactions with zolpidem (10 and 30 mg/kg) leading to reduced rotarod performance and grip strength; in contrast, combination of ethanol (0.32 and 1 g/kg) with almorexant (100 and 300 mg/kg) did not reduce performance or grip strength below ethanol alone. We conclude that unlike zolpidem, almorexant does not interfere with forced motor performance or grip strength in the rat, nor does it further increase the sedative effects of ethanol. Our results suggest that the effect of almorexant can be immediately reversed to full alertness like under physiological sleep, and that almorexant is less likely to show strong sedation, excessive myorelaxation, or interaction with alcohol than commonly prescribed hypnotics such as zolpidem.
Similar content being viewed by others
INTRODUCTION
Approximately one-third to one-half of the adult population experiences symptoms of insomnia at least once in their lifetime, and ∼10–15% meet the criteria for diagnosis of insomnia disorder (Schutte-Rodin et al, 2008; Sullivan and Guilleminault, 2009). Currently, the most commonly prescribed insomnia treatments belong to the class of benzodiazepines and related compounds that enhance the action of the major inhibitory neurotransmitter γ-aminobutyric acid (GABA) in the brain. Although benzodiazepine receptor agonists (including the GABAA-α1 receptor-specific allosteric modulators zolpidem, zaleplon, and zopiclone) are successfully used to treat insomnia symptoms, these medications often are associated with unwanted side effects in terms of abuse potential, tolerance, daytime fatigue, rebound insomnia after withdrawal, and memory and psychomotor impairments (Mohler, 2006; Wafford and Ebert, 2008; Zammit, 2009). Psychomotor impairments include ataxia, loss of balance, drowsiness, attention deficits, and slowed response times. This can impose serious risks of accidents on patients, including fall-related injuries (Allain et al, 2005; Hemmelgarn et al, 1997; Panneman et al, 2003). Elderly patients are among those most affected, especially in cases in which an increased prevalence of insomnia coincides with decreased clearance of a drug, age-related cognitive deficits or reduced physical and mental fitness (Glass et al, 2005; Greenblatt et al, 1989; Kallin et al, 2004). In addition, the sedative action of hypnotic GABA receptor modulators is enhanced by the concomitant use of alcohol, because ethanol acts at least partially by enhancing central GABAergic activity (Hanchar et al, 2005; Liljequist and Engel, 1982; Voss et al, 2003). This is of particular concern because alcohol is used as self-medication by many insomnia patients to help them fall asleep (Stein and Friedmann, 2005). For these reasons, there is a great need for novel approaches to treat insomnia that are less likely to induce psychomotor impairments and unwanted pharmacodynamic interactions (Sullivan and Guilleminault, 2009).
Orexin neuropeptides play a pivotal role in the regulation of vigilance and wakefulness (Saper et al, 2005). Orexin neurons are active during wake stages (Estabrooke et al, 2001), and they innervate and excite major nuclei constituting the arousal system of the brain, such as the locus coeruleus, the raphe nuclei, the tuberomammillary nucleus, and the laterodorsal/pedunculopontine tegmental nuclei by binding to orexin receptors type 1 and type 2 (OXR-1/2) (Mieda and Sakurai, 2009). In addition, the orexin system also orchestrates the emotional and physiological responses that are associated with wakefulness, such as reward, stress processing, appetite, and energy expenditure (Carter et al, 2009). Recently, the dual orexin receptor antagonist almorexant (ACT-078573-hydrochloride) was developed, which reduces time spent in wake states and enables and maintains sleep in rats, dogs, and human subjects (Brisbare-Roch et al, 2007; Hoever et al, 2010).
Sedation and myorelaxation can be investigated in rodents using standard neurological tests such as the accelerating rotating rod (rotarod) and the forepaw grip strength tests (Tang et al, 1995; Voss et al, 2003). We used both tests to determine whether almorexant treatment leads to sedative and muscle-relaxant effects, when given alone or in combination with low doses of ethanol. The positive GABAA-α1 receptor modulator zolpidem was used as a comparator. Wistar rats were tested during their inactive phase of day upon waking after treatment.
MATERIALS AND METHODS
Animals
Male normal Wistar rats (RCC, Füllinsdorf, Switzerland) were maintained under standard laboratory conditions (temperature 20±2°C, relative humidity 55–70%, and food and water ad libitum) under a regular 12-h light/dark cycle (lights on at 0600 hours). Experimental procedures were approved by the local Veterinary Office and adhered to Swiss federal regulations on animal experimentation. All experiments were performed during the light phase of the day between 0800 and 1700 hours.
Drugs and Formulations
Almorexant (Actelion Pharmaceuticals, Allschwil, Switzerland) and zolpidem (purified from commercially available sources by Actelion Pharmaceuticals) were formulated in 100% (v/v) polyethylene glycol 400 at 5 ml/kg body weight. Ethanol (purum ⩾99.8%; Sigma-Aldrich, Buchs, Switzerland) was formulated in 0.9% NaCl at 5 ml/kg body weight. Almorexant concentrations and doses were calculated as the free base.
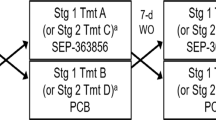
Drug Treatment before Rotarod and Grip Strength Tests
Rats received oral pretreatment with vehicle, almorexant (30, 100, or 300 mg/kg), or zolpidem (10, 30, or 100 mg/kg) 30 min before the first rotarod and grip strength test followed by intraperitoneal treatment with either vehicle or ethanol (0.32, 1, or 1.5 g/kg; i.p.) 15 min before testing, according to published protocols (Voss et al, 2003). Latency to the first episode of continuous 60 s non-rapid eye movement (non-REM) sleep in Wistar rats occurs within 30 min of administration of almorexant (Brisbare-Roch et al, 2007) and zolpidem (24 min for the 10 mg/kg dose, 11 min for the 30 mg/kg dose; in-house pilot experiments). Rotarod and grip strength testing continued at regular intervals within the following 2.5 h (see the following Materials and Methods section for details). Almorexant was also tested using a 2-h pretreatment time to investigate interactions with ethanol at higher brain concentrations of almorexant (see Supplementary Table 1 for a detailed overview of the treatment groups).
Rotarod Test
The rotarod test system (IITC Life Sciences, Woodland Hills, CA, USA) consisted of a rod 9.5 cm in diameter and 20 cm wide located 18 cm above a platform, with the system divided into five separate compartments. Rats were placed onto the rod that accelerated from 5 to 40 revolutions per minute in 2 min. The time the rats spent on the rotarod was measured, with the cutoff time set at 120 s. Trip plates in the platform controlled a digital timer that recorded the time from the start of the test until an animal fell off the rod.
Rats were first trained on the day before the test session in three consecutive trials in the morning plus three consecutive trials in the afternoon until maximal performance was reached. On the testing day, animals received one additional ‘reminder’ training trial before drugs were administered and testing began. Animals were tested repeatedly (five times) on the rotarod at each of 0-, 30-, 60-, 90-, and 150-min test time points to be able to observe pharmacodynamic effects at different time points of the concentration–time profiles of the applied drugs. Rats that did not learn the rotarod task (8 out of 218), defined as rats with a baseline performance of <20 s on the rod, were excluded from the rotarod part of the study. However, these rats were not excluded from the grip strength test (see below). The individual baseline rotarod performance was calculated by averaging the time spent on the rotarod during the last training trial on the day before testing and the time spent on the rotarod during the single ‘reminder’ training trial on the test day. Baseline performances of different experimental groups of rats were comparable and did not differ statistically (see baseline values in Figures 1 and 2). Consequently, absolute values were reported and statistically analyzed.
Effects of acute administration of (a) vehicle (Veh)–ethanol (Eth; 0.32, 1, and 1.5 g/kg, i.p.), (b) zolpidem (Zol; 10, 30, and 100 mg/kg, p.o.)–vehicle, (c) almorexant (Alm; 30, 100, and 300 mg/kg, p.o.)–vehicle, and effects of acute combination of ethanol 0.32 g/kg and ethanol 1 g/kg with pretreatment of either zolpidem 10 mg/kg (d), zolpidem 30 mg/kg (e), almorexant 100 mg/kg (f), or almorexant 300 mg/kg (g) on time spent on the rotarod in Wistar rats. The vehicle–vehicle group data depicted in (a) are repeated in (b and c) to allow better comparison of the respective treatment effects. In (d, e, f, g), these data have been replaced by a dotted line at the mean of vehicle–vehicle group performance across the entire test period (56 s spent on the rotarod) for the purpose of clarity. The data of the respective drug–vehicle treatment groups in (b, c) are repeated in (d, e, f, g) to enable better comparison with the ethanol combination data. Baseline performance levels were measured under drug-free conditions before treatment commenced. All rats received pretreatment (Veh, Zol, Alm) −30 min and treatment (Veh, Eth) −15 min before the first rotarod test at 0 min test time. Testing was repeated five times within the next 2.5 h at the times indicated in the x axis legends. Data are shown as mean±standard error of the mean (SEM); animal numbers are shown within parentheses; *p<0.05 versus vehicle–vehicle in (a, b) and versus the respective drug–vehicle treatment group in (d, f), Tukey's post hoc test following analysis of variance.
Effects of acute vehicle (Veh)–ethanol (Eth; 1 g/kg, i.p.) and almorexant (Alm; 300 mg/kg, p.o.)–vehicle administration, and the combination of almorexant 300 mg/kg with ethanol 1 g/kg on time spent on the rotarod in Wistar rats following a 2 h pretreatment time. Baseline performance was measured under drug-free conditions before treatment commenced. All rats received pretreatment (Veh, Alm) −2 h and treatment (Veh, Eth) −15 min before the first rotarod test at 0 min test time. Testing was repeated five times within the next 2.5 h at the times indicated in the x axis legends. Data are shown as mean±standard error of the mean (SEM); animal numbers are shown within parentheses.
Grip Strength Test
The grip strength test used a triangular bar 2 mm in diameter and 5 cm wide connected to a digital strain gauge (BIOSEB, Vitrolles, France) to measure graded changes in the forelimb grip strength of rats. Animals held by the tail grasped the bar and were then gently pulled away from it in a smooth, steady motion, until they released the bar. The strain gauge measured the force (g) required to break the animal's grip. Three readings were taken for each animal and the average force required was recorded as the individual grip strength score of that rat. Baseline grip strength was measured directly after the single rotarod ‘reminder’ training session on the test day. Animals were then tested (five times) after drug administration, immediately after animals had performed the rotarod task, at the 0-, 30-, 60-, 90-, and 150-min test time points. Individual baseline grip strength performance was calculated by averaging the three first readings for each animal before drug treatment started. Baseline performances of different experimental groups of rats differed significantly in their absolute values (data not shown). Therefore, grip strengths after drug administration were calculated and analyzed as the percentage changes from the respective baselines.
Plasma and Brain Concentrations of Almorexant in Combination with Ethanol
Male Wistar rats were pretreated with almorexant 300 mg/kg, p.o. either 15 or 105 min before receiving either vehicle i.p. or ethanol 1 g/kg, i.p. Rats were killed by an overdose of CO2 after an additional 15 min (30 or 120 min after almorexant administration, respectively). Blood was sampled from the inferior vena cava into plastic tubes coated with ethylenediamine tetraacetic acid as anticoagulant and centrifuged to yield plasma. Halves of the brains were sampled after transcardiac perfusion of 10 ml 0.9% NaCl and homogenized into one volume of cold phosphate buffer (pH 7.4). Following extraction with methanol, concentrations of almorexant in brain homogenate and plasma were determined using liquid chromatography coupled to tandem mass spectrometry. Ethanol concentrations in plasma and ethanol concentrations in the other halves of the brains were determined by a commercially available enzyme-linked immunosorbent assay (EnzyChrom Ethanol Assay Kit; BioAssay Systems, Hayward, CA).
Statistical Analysis
Data are presented as mean±standard error of the mean (SEM). Statistical analyses of dose–response drug effects and drug–ethanol interaction effects on rotarod performance and grip strength were performed using two-way analyses of variances (factors: treatment, time) for repeated measures (time), followed by Tukey's post hoc test where appropriate. Plasma and brain concentrations of almorexant and ethanol were evaluated using Student's t-test. Significance level was set at p<0.05.
RESULTS
Rotarod Performance
Effects of acute ethanol, zolpidem, and almorexant administration on rotarod performance
The control group of rats that received both vehicle pretreatment and vehicle treatment exhibited similar rotarod performance at all test time points (0–150 min; Figure 1a). Animals that received vehicle pretreatment and ethanol treatment showed an ethanol dose-dependent decrease in time spent on the rotarod (treatment: F3,45=8.9, p<0.001; Figure 1a), with an effective ethanol dose of 1.5 g/kg. The effect of ethanol was strongest at test time 0 min, 15 min after ethanol injection, and faded over the 2.5-h test period (treatment × time: F12,180=3.5, p<0.001). Similar to ethanol-treated animals, rats that received zolpidem pretreatment and vehicle treatment showed also reduced rotarod performance in a dose-dependent manner (treatment: F3,42=9.5, p<0.001; Figure 1b), with effective zolpidem doses of 30 and 100 mg/kg. However, impairment of rotarod performance by zolpidem 100 mg/kg was longer lasting than by ethanol 1.5 g/kg and relatively stable over the entire 2.5-h test period (treatment × time: F12,168=1.6, NS). In contrast to both ethanol and zolpidem, which strongly impaired rotarod performance, almorexant-pretreated and vehicle-treated rats did not display reduced rotarod performance below vehicle–vehicle levels at any time point during the 2.5-h testing period (treatment: F3,44=2.6, NS; Figure 1c). A nonsignificant trend toward an increase was observed (p=0.06).
Effects of acute administration of zolpidem or almorexant combined with low doses of ethanol on rotarod performance
Zolpidem–ethanol and almorexant–ethanol interaction effects were investigated using the 0.32 and 1 g/kg ethanol doses, which, when administered alone, had no significant effect on rotarod performance (see Figure 1a). For the zolpidem pretreatment, the two lower zolpidem doses (10 and 30 mg/kg) were used to allow for the detection of a further decrease in rotarod performance when administered in combination with ethanol. For the almorexant pretreatment, the two highest doses (100 and 300 mg/kg) were chosen based on the hypothesis that these doses were most likely to reveal a potential interaction with ethanol.
Combining zolpidem 10 mg/kg with the 0.32 g/kg ethanol dose revealed no effects on rotarod performance that were different from zolpidem–vehicle alone (Figure 1d). However, combining zolpidem 10 mg/kg with the 1 g/kg dose of ethanol resulted in a marked decrease in rotarod performance to below vehicle–vehicle and zolpidem–vehicle levels (treatment × time: F8,140=5.5, p<0.001). This zolpidem–ethanol interaction was most prominent 15 min after ethanol administration (test time 0 min) and gradually faded over the test period. Similar effects of ethanol were observed for the combination with zolpidem 30 mg/kg (Figure 1e). Zolpidem (30 mg/kg)–vehicle alone reduced rotarod performance to below vehicle–vehicle levels. Combination of zolpidem 30 mg/kg with ethanol 0.32 g/kg had no effect, but combination of zolpidem 30 mg/kg with ethanol 1 g/kg resulted in a further decrease in performance during the first hour after ethanol administration (treatment × time: F8,108=5.6, p<0.001).
Combining almorexant 100 mg/kg with ethanol 0.32 and 1 g/kg resulted in rotarod performance levels comparable with vehicle–vehicle-treated animals (treatment: F2,27=5.1, p<0.05; Figure 1f). Similar results were observed for the combination of the higher almorexant dose of 300 mg/kg with ethanol (treatment: F2,27=1.9, NS; Figure 1g).
In the additional experiment using a 2-h pretreatment time, a significant almorexant pretreatment × ethanol treatment interaction was observed (F1,32=4.7, p<0.05; Figure 2). Although almorexant (300 mg/kg)–vehicle did not affect rotarod performance compared with vehicle–vehicle, almorexant (300 mg/kg)–ethanol (1 g/kg)-treated rats appeared to perform slightly better than vehicle–ethanol (1 g/kg)-treated rats.
Overall, combination of zolpidem with low doses of ethanol, which did not impair motor function per se, further reduced rotarod performance of rats to below vehicle–vehicle and zolpidem–vehicle levels. In contrast, combination of almorexant with low doses of ethanol did never reduce rotarod performance to below vehicle–vehicle or vehicle–ethanol levels.
Grip Strength
Effects of acute ethanol, zolpidem, and almorexant administration on forepaw grip strength
Administration of ethanol significantly decreased grip strength in a dose-dependent manner (treatment: F3,48=7.0, p<0.001; Figure 3a), with an effective dose of 1.5 g/kg. As with the rotarod results, the effect of ethanol on grip strength was strongest 15 min after injection (0 min test time) and faded over the remaining 2.5 h of the test period (treatment × time: F12,192=2.3, p<0.01). Administration of zolpidem also decreased grip strength in a dose-dependent manner (treatment: F3,46=8.5, p<0.001; Figure 3b), with an effective dose of 100 mg/kg. Similar to ethanol, the effect of zolpidem was strongest at early test time points (treatment × time: F12,184=2.0, p<0.05). However, in contrast to ethanol the effect was long lasting and still apparent at the final grip strength test 2.5 h later. Administration of almorexant resulted in a significant treatment effect (F3,47=4.7, p<0.01; Figure 3c). The two lower doses of almorexant (30 and 100 mg/kg) had little effect on grip strength, whereas the highest dose (300 mg/kg) significantly increased grip strength.
Effects of acute administration of (a) vehicle (Veh)–ethanol (Eth; 0.32, 1, and 1.5 g/kg, i.p.), (b) zolpidem (Zol; 10, 30, and 100 mg/kg, p.o.)–vehicle, and (c) almorexant (Alm; 30, 100, and 300 mg/kg, p.o.)–vehicle, and effects of acute combination of ethanol 0.32 g/kg and ethanol 1 g/kg with pretreatment of either zolpidem 10 mg/kg (d), zolpidem 30 mg/kg (e), almorexant 100 mg/kg (f), or almorexant 300 mg/kg (g) on forepaw grip strength in Wistar rats. All values are shown as percentage change from baseline (measured under drug-free conditions before treatment commenced). The vehicle–vehicle group data shown in (a) are repeated in (b and c) to allow better comparison of the respective treatment effects. The data of the respective drug–vehicle treatment groups in (b, c) are repeated in (d, e, f, g) to enable better comparison with the ethanol combination data. All rats received pretreatment (Veh, Zol, Alm) −30 min and treatment (Veh, Eth) −15 min before the first grip strength test at 0 min test time. Testing was repeated five times within the next 2.5 h at the times indicated in the x axis legends. Data are shown as mean±standard error of the mean (SEM); animal numbers are shown within parentheses; *<0.05 versus vehicle–vehicle in (a, b) and versus the respective drug–vehicle treatment group in (d, e, g), Tukey's post hoc test following analysis of variance.
Overall, the administration of both ethanol and zolpidem at high doses decreased forepaw grip strength, whereas the highest dose of almorexant increased grip strength.
Effects of acute administration of zolpidem or almorexant combined with low doses of ethanol on forepaw grip strength
Combining zolpidem 10 mg/kg with the 0.32 and 1 g/kg doses of ethanol resulted in a further decrease in the grip strengths of rats (Figure 3d). The decrease was evident over the entire 2.5-h test period for the combination of zolpidem 10 mg/kg with ethanol 0.32 g/kg and evident for the combination of zolpidem 10 mg/kg with ethanol 1 g/kg during the first hour of testing (treatment × time: F8,108=3.2, p<0.01). Combining 30 mg/kg zolpidem with 0.32 and 1 g/kg ethanol revealed similar results to those observed for zolpidem 10 mg/kg. However, the ethanol-dependent decrease in grip strength was even more pronounced for the higher zolpidem dose (treatment × time: F8,108=4.4, p<0.001, Figure 3e), particularly at the earliest test time point (0 min).
Combining almorexant 100 mg/kg with ethanol 0.32 and 1 g/kg revealed a significant co-treatment effect (treatment: F2,27=4.0, p<0.05; Figure 3f). Combination of almorexant with 0.32 g/kg ethanol slightly increased grip strength, whereas combination with 1 g/kg ethanol slightly decreased grip strength. In comparison to the zolpidem–ethanol interactions, these effects were less pronounced. Combining the higher dose of almorexant (300 mg/kg) with ethanol 0.32 and 1 g/kg reversed the slightly improved grip strength performance observed with almorexant (300 mg/kg)–vehicle (treatment: F2,27=5.8, p<0.01; Figure 3g), and resulted in grip strength levels comparable with those achieved for administration of vehicle–ethanol 0.32 and 1 g/kg alone (compare Figure 3a for these groups).
In the experiment investigating the almorexant 300 mg/kg–ethanol 1 g/kg interaction following a 2-h almorexant pretreatment time, neither almorexant (300 mg/kg)–vehicle nor vehicle–ethanol (1 g/kg), nor the almorexant (300 mg/kg)–ethanol (1 g/kg) combination significantly affected grip strength performance (Figure 4).
Effects of acute vehicle (Veh)–ethanol (Eth; 1 g/kg, i.p.) and almorexant (Alm; 300 mg/kg, p.o.)–vehicle administration, and the combination of almorexant 300 mg/kg with ethanol 1 g/kg on forepaw grip strength in Wistar rats following a 2 h pretreatment time. The grip strength values are shown as percentage change from baseline (measured under drug-free conditions before treatment commenced). All rats received pretreatment (Veh, Alm) −2 h and treatment (Veh, Eth) −15 min before the first grip strength test at 0 min test time. Testing was repeated five times within the next 2.5 h at the times indicated in the x axis legends. Data are shown as mean±standard error of the mean (SEM); animal numbers are shown within parentheses.
In general, low doses of zolpidem and ethanol interacted to decrease forepaw grip strength in rats below zolpidem–vehicle and vehicle–vehicle levels, which was not observed with the combination of almorexant and ethanol. However, combination of almorexant with ethanol was able to block the slightly increased grip strength observed with almorexant 300 mg/kg–vehicle treatment.
Plasma and Brain Concentrations of Almorexant in Combination with Ethanol
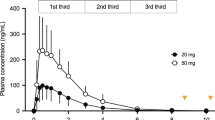
To investigate whether combination of almorexant 300 mg/kg and ethanol 1 g/kg resulted in a pharmacokinetic interaction, brain and plasma concentration of both compounds were measured at the first rotarod/grip test time point (0 min), at which the greatest effects of ethanol were observed. Almorexant concentrations, both 2 h and 30 min after pretreatment, were not affected by the combination with ethanol 105 or 15 min following almorexant administration, respectively (Table 1). Conversely, ethanol brain and plasma concentrations were not affected by almorexant pretreatment either. Plasma and brain concentrations of almorexant were significantly higher when measured 2 h after administration compared with 30 min after administration (p<0.001).
DISCUSSION
Our study shows that both the positive GABAA-α1 receptor modulator zolpidem and ethanol dose dependently decreased forced motor performance of rats in two neurological tests for motor function. These findings are in agreement with other preclinical results on rotarod and loaded grid test performance (Sanger et al, 1996; Voss et al, 2003), and also correspond to findings in humans on body sway, information processing rate, immediate memory, and sustained attention (Kleykamp et al, 2010; van Steveninck et al, 1996; Wilkinson, 1995). Almorexant, on the contrary, showed no effects on forced motor performance in the rat. Whether these results translate to human subjects is currently under investigation.
GABA is the major inhibitory neurotransmitter. Ionotropic GABAA receptors are comprised of five protein subunits that form the central ion pore. Sixteen different subunits are currently known, α1–6, β1–3, γ1–3, δ, ɛ, π, and θ (Mohler, 2006). Zolpidem is a preferential positive allosteric modulator of GABAA receptors containing the α1-subunit, which is the most abundant GABAA receptor subtype in the brain. As such, zolpidem enhances the inhibitory effects of GABA in a variety of brain structures and thereby exerts its sedative and hypnotic effects. Unlike zolpidem, the exact molecular mechanism by which ethanol exerts its sedative potential is not fully understood. One theory suggests a direct influence of ethanol on ion channels and receptors by nonspecific interactions with neuronal membranes, whereas another theory proposes direct specific binding sites for ethanol on a variety of receptor or ion channel proteins (Harris et al, 2008). Prominent among the suggested specific direct targets for ethanol are GABAA receptors. These have long been suspected because of the similarity of behavioral effects for ethanol and prototypical GABAA modulators. In particular, recent evidence favors the extrasynaptic α4β3δ and α6β3δ subtypes (Hanchar et al, 2005; Olsen et al, 2007). Overall, given the pharmacological profiles of zolpidem and ethanol, which both act by increasing GABA-mediated neuronal inhibition, it is not surprising to observe strong sedative and muscle-relaxant effects at high doses or synergy when they are combined.
In contrast to zolpidem and other conventional hypnotics, which are based on GABAA receptor modulation, almorexant utilizes a completely different mechanism of action. It blocks both OXR-1 and OXR-2 with almost equimolar potency (IC50 of 16 and 15 nM, respectively, as measured by calcium mobilization in Chinese hamster ovary cells; Brisbare-Roch et al, 2007). Orexin signaling is an important innate driving force of vigilance and wakefulness (Saper et al, 2005), which is thus attenuated by the binding of almorexant to the orexin receptors. Consequently, almorexant treatment favors a physiological state of sleep conserving rapid eye movement (REM) and non-REM sleep architecture (Brisbare-Roch et al, 2007).
This study was performed during daylight hours under a regular 12 h dark–light rhythm and, thus, during the sleep period of the nocturnally active rat. Still, rats woken up under almorexant treatment were able to perform normally on a forced motor task. Thus, our results provide evidence that, unlike for zolpidem and ethanol, the effect of almorexant can be immediately reversed to full alertness in the rat. This has the potential to provide a clinical advantage over benzodiazepine-like drugs, which have been shown in several studies to increase the incidence of falls and hip-fractures owing to psychomotor side effects (Chang et al, 2008; Cumming and Le Couteur, 2003; Wang et al, 2001).
Selective OXR-1 blockade was reported to reduce the ability of rats to discriminate visual signals in a two-lever sustained attention task (Boschen et al, 2009), and orexin inputs to the basal forebrain cholinergic system have been proposed to represent an anatomical substrate for the link between arousal and attention (Fadel and Burk, 2010). Although the rotarod is not comparable with a classical discrimination task, it is conceivable that rotarod performance requires a substantial level of attention from the rat to maintain stability on the rod, while it is rotating at increasing speed. From this perspective, our data does not favor the view that orexin receptor blockade by almorexant would dramatically decrease attention.
The orexin system is also involved in some parts of the learning and memory processes. The exact underlying processes have been controversially discussed, but the question whether pharmacological blockade of both OXR-1 and OXR-2 has any influence on memory acquisition in the rat has recently been addressed by testing almorexant in the Morris water maze and passive avoidance tasks (Dietrich and Jenck, 2010). Rats under almorexant treatment were fully capable of spatial and avoidance learning. In the present study, we did not directly assess the effect of almorexant on rotarod task acquisition as the rats were trained under drug-free conditions. However, rats had to retrieve their procedural rotarod memory on the testing day under the exposure of almorexant. As almorexant-treated rats did perform in this motor task equally well as vehicle-treated rats, we can conclude that almorexant did not interfere with the retrieval of procedural memory in this motor learning paradigm (rotarod). In fact, these data are in accordance with previous findings showing that almorexant did not interfere with the retrieval of spatial memory in the Morris water maze (Dietrich and Jenck, 2010).
The sedative effects of GABAA receptor modulators are known to increase when combined with low doses of alcohol in both animals and humans (van Steveninck et al, 1996; Voss et al, 2003). As alcohol is commonly consumed in the general population and is also frequently used as a self-medication by insomnia patients (Stein and Friedmann, 2005), an interaction with hypnotic drugs can further increase the risk of accidents associated with psychomotor impairments. In this study, we explored potential interactions of zolpidem 10 and 30 mg/kg and almorexant 100 and 300 mg/kg with low doses of ethanol 0.32 and 1 g/kg. For zolpidem, consistent interactions with ethanol were observed across dose levels on both the rotarod and grip strength tests. Low doses of ethanol significantly increased the sedative effects of zolpidem as evidenced by reduced rotarod and grip strength performance of rats to below vehicle–ethanol and zolpidem–vehicle levels. The observed interaction effects were strongest at the first testing time point (15 min after ethanol administration), which was closest to the peak ethanol blood levels that usually occur within 5–10 min of i.p. injection (Adalsteinsson et al, 2006). These findings are in accordance with results from other laboratories that have shown zolpidem–ethanol or benzodiazepine–ethanol interactions in the rat (Liljequist and Engel, 1982; Tang et al, 1995; Voss et al, 2003).
Almorexant 100 and 300 mg/kg was also tested in combination with low doses of ethanol. In contrast to zolpidem–ethanol combinations, no reduction of rotarod performance to below levels of vehicle–ethanol-treated rats was observed. Similarly, no reduction of grip strength performance to below vehicle–ethanol levels was detected. However, combination of almorexant with ethanol did prevent the slightly advantageous effects of almorexant alone on both motor tasks. The lack of pharmacokinetic interaction between ethanol and almorexant at test time 0 min (peak sedative effects of ethanol) indicates that these effects were not of pharmacokinetic, but rather of pharmacodynamic nature. A broad in vitro receptor/channel affinity screen has shown that almorexant is at least 600-fold selective for both orexin receptors over GABAA receptor channels (Brisbare-Roch et al, 2007). In contrast, for ethanol GABAA receptors have been proposed as both direct and indirect targets (Harris et al, 2008) that mediate at least part of its sedative effects. In light of these data, the interaction of ethanol with zolpidem, and the lack of interaction of ethanol with almorexant could potentially be explained from this molecular mechanistic perspective. Nevertheless, because of the high brain concentrations of almorexant in rats reached at 300 mg/kg a full characterization of the brain almorexant binding profile in vivo or ex vivo would be necessary to fully exclude GABAA receptor binding under these conditions.
Maximal plasma concentrations of almorexant in the rat at the high dose of 300 mg/kg in this study (∼5800 ng/ml) were significantly larger than those reported in human at the highest investigated oral dose of 1000 mg (∼290 ng/ml; Hoever et al, 2010). Both rat and human threshold doses for maintenance of sleep are 30 mg/kg in rat and 400 mg in human. The respective maximal plasma concentrations are 520 ng/ml in rats (unpublished results) and 115 ng/ml in human (Hoever et al, 2010). Two related factors may explain species differences in almorexant plasma concentrations: first, the high metabolic rate in rats, and second, the fact that almorexant is a substrate for efflux P-glycoproteins in rats but not in humans (unpublished data).
In conclusion, this study in rats shows that the positive GABAA-α1 receptor modulator zolpidem induced significant dose-dependent sedative and myorelaxant effects in both the rotarod and grip strength tests, whereas, in contrast, the dual orexin receptor antagonist almorexant did not. This indicates that in rats the sleep-enabling effect of almorexant can be fully and immediately surmounted, like under natural sleep conditions. Furthermore, low doses of ethanol significantly enhanced the sedative effects of zolpidem, whereas combination of ethanol with almorexant revealed no deleterious effects on rotarod performance or grip strength. These preclinical studies predict that in humans almorexant treatment should be less likely than zolpidem to show unwanted side effects of strong sedation, excessive myorelaxation, or interaction with ethanol.
References
Adalsteinsson E, Sullivan EV, Mayer D, Pfefferbaum A (2006). In vivo quantification of ethanol kinetics in rat brain. Neuropsychopharmacology 31: 2683–2691.
Allain H, Bentue-Ferrer D, Polard E, Akwa Y, Patat A (2005). Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging 22: 749–765.
Boschen KE, Fadel JR, Burk JA (2009). Systemic and intrabasalis administration of the orexin-1 receptor antagonist, SB-334867, disrupts attentional performance in rats. Psychopharmacology (Berl) 206: 205–213.
Brisbare-Roch C, Dingemanse J, Koberstein R, Hoever P, Aissaoui H, Flores S . et al (2007). Promotion of sleep by targeting the orexin system in rats, dogs and humans. Nat Med 13: 150–155.
Carter ME, Borg JS, de Lecea L (2009). The brain hypocretins and their receptors: mediators of allostatic arousal. Curr Opin Pharmacol 9: 39–45.
Chang CM, Wu EC, Chang IS, Lin KM (2008). Benzodiazepine and risk of hip fractures in older people: a nested case–control study in Taiwan. Am J Geriatr Psychiatry 16: 686–692.
Cumming RG, Le Couteur DG (2003). Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 17: 825–837.
Dietrich H, Jenck F (2010). Intact learning and memory in rats following treatment with the dual orexin receptor antagonist almorexant. Psychopharmacology (Berl) 212: 145–154.
Estabrooke IV, McCarthy MT, Ko E, Chou TC, Chemelli RM, Yanagisawa M et al (2001). Fos expression in orexin neurons varies with behavioral state. J Neurosci 21: 1656–1662.
Fadel J, Burk JA (2010). Orexin/hypocretin modulation of the basal forebrain cholinergic system: role in attention. Brain Res 1314: 112–123.
Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE (2005). Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 331: 1169.
Greenblatt DJ, Shader RI, Harmatz JS (1989). Implications of altered drug disposition in the elderly: studies of benzodiazepines. J Clin Pharmacol 29: 866–872.
Hanchar HJ, Dodson PD, Olsen RW, Otis TS, Wallner M (2005). Alcohol-induced motor impairment caused by increased extrasynaptic GABA(A) receptor activity. Nat Neurosci 8: 339–345.
Harris RA, Trudell JR, Mihic SJ (2008). Ethanol's molecular targets. Sci Signal 1: re7.
Hemmelgarn B, Suissa S, Huang A, Boivin JF, Pinard G (1997). Benzodiazepine use and the risk of motor vehicle crash in the elderly. JAMA 278: 27–31.
Hoever P, de Haas S, Winkler J, Schoemaker RC, Chiossi E, van Gerven J et al (2010). Orexin receptor antagonism, a new sleep-promoting paradigm: an ascending single-dose study with almorexant. Clin Pharmacol Ther 87: 593–600.
Kallin K, Jensen J, Olsson LL, Nyberg L, Gustafson Y (2004). Why the elderly fall in residential care facilities, and suggested remedies. J Fam Pract 53: 41–52.
Kleykamp BA, Griffiths RR, Mintzer MZ (2010). Dose effects of triazolam and alcohol on cognitive performance in healthy volunteers. Exp Clin Psychopharmacol 18: 1–16.
Liljequist S, Engel J (1982). Effects of GABAergic agonists and antagonists on various ethanol-induced behavioral changes. Psychopharmacology (Berl) 78: 71–75.
Mieda M, Sakurai T (2009). Integrative physiology of orexins and orexin receptors. CNS Neurol Disord Drug Targets 8: 281–295.
Mohler H (2006). GABA(A) receptor diversity and pharmacology. Cell Tissue Res 326: 505–516.
Olsen RW, Hanchar HJ, Meera P, Wallner M (2007). GABAA receptor subtypes: the ‘one glass of wine’ receptors. Alcohol 41: 201–209.
Panneman MJ, Goettsch WG, Kramarz P, Herings RM (2003). The costs of benzodiazepine-associated hospital-treated fall Injuries in the EU: a Pharmo study. Drugs Aging 20: 833–839.
Sanger DJ, Morel E, Perrault G (1996). Comparison of the pharmacological profiles of the hypnotic drugs, zaleplon and zolpidem. Eur J Pharmacol 313: 35–42.
Saper CB, Scammell TE, Lu J (2005). Hypothalamic regulation of sleep and circadian rhythms. Nature 437: 1257–1263.
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 4: 487–504.
Stein MD, Friedmann PD (2005). Disturbed sleep and its relationship to alcohol use. Subst Abus 26: 1–13.
Sullivan SS, Guilleminault C (2009). Emerging drugs for insomnia: new frontiers for old and novel targets. Expert Opin Emerg Drugs 14: 411–422.
Tang AH, Smith MW, Carter DB, Im WB, VonVoigtlander PF (1995). U-90042, a sedative/hypnotic compound that interacts differentially with the GABAA receptor subtypes. J Pharmacol Exp Ther 275: 761–767.
van Steveninck AL, Gieschke R, Schoemaker RC, Roncari G, Tuk B, Pieters MS et al (1996). Pharmacokinetic and pharmacodynamic interactions of bretazenil and diazepam with alcohol. Br J Clin Pharmacol 41: 565–573.
Voss J, Sanchez C, Michelsen S, Ebert B (2003). Rotarod studies in the rat of the GABAA receptor agonist gaboxadol: lack of ethanol potentiation and benzodiazepine cross-tolerance. Eur J Pharmacol 482: 215–222.
Wafford KA, Ebert B (2008). Emerging anti-insomnia drugs: tackling sleeplessness and the quality of wake time. Nat Rev Drug Discov 7: 530–540.
Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J (2001). Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. Am J Psychiatry 158: 892–898.
Wilkinson CJ (1995). The acute effects of zolpidem, administered alone and with alcohol, on cognitive and psychomotor function. J Clin Psychiatry 56: 309–318.
Zammit G (2009). Comparative tolerability of newer agents for insomnia. Drug Saf 32: 735–748.
Acknowledgements
We thank Alex Dorr (Actelion Pharmaceuticals Ltd, Switzerland) and Gail Rickard (Medi Cine International, sponsored by Actelion Pharmaceuticals Ltd, Switzerland) for editorial assistance with the manuscript. We thank Stephane Delahaye, Julie Hoerner, Malvina Louis, Cedric Fischer, Carla Sciarretta, and Helene Roellinger (Actelion Pharmaceuticals Ltd, Switzerland) for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors MAS, HL, DSS, CBR, and FJ are all employees of Actelion Pharmaceuticals Ltd, Switzerland. They declare that no financial support or compensation has been received over the past 3 years or is anticipated to be received in the near future for research or professional services from any other corporate entity than Actelion.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Steiner, M., Lecourt, H., Strasser, D. et al. Differential Effects of the Dual Orexin Receptor Antagonist Almorexant and the GABAA-α1 Receptor Modulator Zolpidem, Alone or Combined with Ethanol, on Motor Performance in the Rat. Neuropsychopharmacol 36, 848–856 (2011). https://doi.org/10.1038/npp.2010.224
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2010.224
Keywords
This article is cited by
-
Orexin Receptor Antagonists as Emerging Treatments for Psychiatric Disorders
Neuroscience Bulletin (2020)
-
Orexin Receptor Antagonists
Current Sleep Medicine Reports (2017)
-
Sodium Butyrate, a Histone Deacetylase Inhibitor, Exhibits Neuroprotective/Neurogenic Effects in a Rat Model of Neonatal Hypoxia-Ischemia
Molecular Neurobiology (2017)
-
The Dual Hypocretin Receptor Antagonist Almorexant is Permissive for Activation of Wake-Promoting Systems
Neuropsychopharmacology (2016)
-
Assessment of the Abuse Liability of a Dual Orexin Receptor Antagonist: A Crossover Study of Almorexant and Zolpidem in Recreational Drug Users
CNS Drugs (2014)