Key Points
-
The most frequently detected human papillomavirus (HPV) type at the time of diagnosis of squamous cell carcinoma (SCC) is HPV16, followed by HPV18. HPV18 is the type most strongly associated with adenocarcinoma of the cervix, which is increasing in incidence at the same time as the incidence of SCC is falling.
-
A bivalent HPV (types 16 and 18) and a quadrivalent HPV (types 6, 11, 16 and 18) vaccine are now being evaluated in phase III clinical trials, and have the potential to prevent about 70% of all cervical cancers. The quadrivalent HPV vaccine (Gardasil, Merck) has recently gained FDA and European Commission approval for use in women between the ages of 9–26.
-
Although most women will at some time be infected with HPV, very few will progress to invasive disease. The identification of more robust markers of disease progression requires a more complete understanding of the natural history of type-specific HPV infections.
-
It is unknown whether persistent HPV infections are characterized by the continuing detection of HPV, or by a state of viral latency during which the virus remains undetectable only to reappear later. A clearer understanding of these issues is essential for the effective implementation of screening strategies that include testing for HPV.
-
Integration of HPV into the host genome results in a loss of negative-feedback control of oncogene expression, following disruption of the viral regulatory early gene E2. Whether the integration event itself is crucial to carcinogenesis is the subject of continuing debate.
-
The prevalence of integrated forms varies with the infecting HPV type. Unlike HPV16, HPV18 integration seems virtually complete in women with cervical intraepithelial neoplasia grade 3 (CIN3) or invasive disease.
-
The association between viral load and cervical disease varies with the HPV type, the physical state of the virus and the heterogeneity of the cervical lesion. The complexity of these relationships indicates that a measurement of viral load is not clinically useful.
-
The concurrent or sequential detection of more than one HPV type is common. There is some evidence to indicate that the life cycles of different HPV types are not independent of each other, as has previously been assumed.
-
HPV oncogenes can activate the cellular methylation machinery. The pattern of HPV gene methylation varies with the viral life cycle, the presence of disease and possibly the HPV type.
-
Aberrant methylation of CpG islands in the promoter regions of tumour suppressor genes is one of several epigenetic changes that can contribute to carcinogenesis. The detection of these epigenetic changes in exfoliated cervical cells could improve the effectiveness of cervical screening programmes.
Abstract
The identification of high-risk human papillomavirus (HPV) types as a necessary cause of cervical cancer offers the prospect of effective primary prevention and the possibility of improving the efficiency of cervical screening programmes. However, for these opportunities to be realized, a more complete understanding of the natural history of HPV infection, and its relationship to the development of epithelial abnormalities of the cervix, is required. We discuss areas of uncertainty, and their possible effect on disease prevention strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Parkin, D. M. & Bray, F. Chapter 2: the burden of HPV-related cancers. Vaccine 24 (Suppl. 3), S11–S25 (2006).
World Health Organization. International Agency for Research on Cancer. GLOBOCAN database 2002. CANCERMondial [online], http://www-dep.iarc.fr/ (2002).
Wang, S. S., Sherman, M. E., Hildesheim, A., Lacey, J. V. Jr & Devesa, S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976–2000. Cancer 100, 1035–1044 (2004).
Bray, F. et al. Incidence trends of adenocarcinoma of the cervix in 13 European countries. Cancer Epidemiol. Biomarkers Prev. 14, 2191–2199 (2005).
de Villiers, E. M., Fauquet, C., Broker, T. R., Bernard, H. U. & zur Hausen, H. Classification of papillomaviruses. Virology 324, 17–27 (2004).
Collins, S. et al. High incidence of cervical human papillomavirus infection in women during their first sexual relationship. BJOG 109, 96–98 (2002).
Castle, P. E. et al. A prospective study of age trends in cervical human papillomavirus acquisition and persistence in Guanacaste, Costa Rica. J. Infect. Dis. 191, 1808–1816 (2005).
Franceschi, S. et al. Variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int. J. Cancer 119, 2677–2684 (2006). This is a cross-sectional study of sexually active women from the general population of 15 areas in four continents; it describes age-specific curves of HPV prevalence, and draws attention to the finding in some societies of a second peak of HPV infection in older women.
Woodman, C. B. et al. Natural history of cervical human papillomavirus infection in young women: a longitudinal cohort study. Lancet 357, 1831–1836 (2001).
de Sanjose, S. et al. Clearance of HPV infection in middle aged men and women after 9 years' follow up. Sex. Transm. Infect. 79, 348 (2003).
Richardson, H. et al. The natural history of type-specific human papillomavirus infections in female university students. Cancer Epidemiol. Biomarkers Prev. 12, 485–490 (2003).
Ho, G. Y. et al. Persistent genital human papillomavirus infection as a risk factor for persistent cervical dysplasia. J. Natl Cancer Inst. 87, 1365–1371 (1995).
Thomas, K. K. et al. Concurrent and sequential acquisition of different genital human papillomavirus types. J. Infect. Dis. 182, 1097–1102 (2000).
Liaw, K. L. et al. A prospective study of human papillomavirus (HPV) type 16 DNA detection by polymerase chain reaction and its association with acquisition and persistence of other HPV types. J. Infect. Dis. 183, 8–15 (2001).
Rousseau, M. C. et al. Cervical coinfection with human papillomavirus (HPV) types as a predictor of acquisition and persistence of HPV infection. J. Infect. Dis. 184, 1508–1517 (2001).
Ho, G. Y. et al. Risk factors for subsequent cervicovaginal human papillomavirus (HPV) infection and the protective role of antibodies to HPV-16 virus-like particles. J. Infect. Dis. 186, 737–742 (2002).
Brown, D. R. et al. A longitudinal study of genital human papillomavirus infection in a cohort of closely followed adolescent women. J. Infect. Dis. 191, 182–192 (2005).
Mendez, F. et al. Cervical coinfection with human papillomavirus (HPV) types and possible implications for the prevention of cervical cancer by HPV vaccines. J. Infect. Dis. 192, 1158–1165 (2005). This study includes women with incident infections and shows that the concurrent acquisition of multiple HPV types occurs more frequently than would be expected by chance.
zur Hausen, H. Papillomaviruses and cancer: from basic studies to clinical application. Nature Rev. Cancer 2, 342–350 (2002). This review details the contribution of HPV to the pathogenesis of cervical neoplasia.
Roden, R. & Wu, T. C. How will HPV vaccines affect cervical cancer? Nature Rev. Cancer 6, 753–763 (2006). This recent review considers the ramifications of prophylactic HPV vaccines.
Doorbar, J. Molecular biology of human papillomavirus infection and cervical cancer. Clin. Sci. 110, 525–541 (2006).
Clifford, G. M., Smith, J. S., Plummer, M., Munoz, N. & Franceschi, S. Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br. J. Cancer 88, 63–73 (2003).
Munoz, N. et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N. Engl. J. Med. 348, 518–527 (2003).
Koutsky, L. A. & Harper, D. M. Chapter 13: current findings from prophylactic HPV vaccine trials. Vaccine 24 (Suppl. 3), S114–S121 (2006).
Tyler, K. and Nathanson, N. in Fields Virology 4th edn (eds Fields BN, Knipe, D.M., and Howley, P.M.), 220–222 (Lippincott Willliams & Wilkins, Philadelphia, 2001). This chapter reviews the characteristics of persistent viral infections.
Koutsky, L. A. et al. A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N. Engl. J. Med. 327, 1272–1278 (1992).
Evander, M. et al. Human papillomavirus infection is transient in young women: a population-based cohort study. J. Infect. Dis. 171, 1026–1030 (1995).
Giuliano, A. R. et al. Antioxidant nutrients: associations with persistent human papillomavirus infection. Cancer Epidemiol. Biomarkers Prev. 6, 917–923 (1997).
Ho, G. Y., Bierman, R., Beardsley, L., Chang, C. J. & Burk, R. D. Natural history of cervicovaginal papillomavirus infection in young women. N. Engl. J. Med. 338, 423–428 (1998).
Liaw, K. L. et al. Detection of human papillomavirus DNA in cytologically normal women and subsequent cervical squamous intraepithelial lesions. J. Natl Cancer Inst. 91, 954–960 (1999).
Nobbenhuis, M. A. et al. Relation of human papillomavirus status to cervical lesions and consequences for cervical-cancer screening: a prospective study. Lancet 354, 20–25 (1999).
Wallin, K. L. et al. Type-specific persistence of human papillomavirus DNA before the development of invasive cervical cancer. N. Engl. J. Med. 341, 1633–1638 (1999). This article shows that a single positive finding of HPV DNA in a Pap smear confers increased risk of future invasive cervical cancer that is positive for the same type of virus as identified earlier; it also shows that HPV DNA can only be detected in cytologically normal samples for a short time before cervical cancer is diagnosed.
Clavel, C. et al. Human papillomavirus detection by the hybrid capture II assay: a reliable test to select women with normal cervical smears at risk for developing cervical lesions. Diagn. Mol. Pathol. 9, 145–150 (2000).
Elfgren, K., Kalantari, M., Moberger, B., Hagmar, B. & Dillner, J. A population-based five-year follow-up study of cervical human papillomavirus infection. Am. J. Obstet. Gynecol. 183, 561–567 (2000).
Hopman, E. H. et al. High risk human papillomavirus in women with normal cervical cytology prior to the development of abnormal cytology and colposcopy. BJOG 107, 600–604 (2000).
Ylitalo, N. et al. A prospective study showing long-term infection with human papillomavirus 16 before the development of cervical carcinoma in situ. Cancer Res. 60, 6027–6032 (2000).
Ahdieh, L. et al. Prevalence, incidence, and type-specific persistence of human papillomavirus in human immunodeficiency virus (HIV)-positive and HIV-negative women. J. Infect. Dis. 184, 682–690 (2001).
Ghaderi, M. et al. Risk of invasive cervical cancer associated with polymorphic HLA DR/DQ haplotypes. Int. J. Cancer 100, 698–701 (2002).
Kjaer, S. K. et al. Type specific persistence of high risk human papillomavirus (HPV) as indicator of high grade cervical squamous intraepithelial lesions in young women: population based prospective follow up study. BMJ 325, 572 (2002).
Sedjo, R. L. et al. Human papillomavirus persistence and nutrients involved in the methylation pathway among a cohort of young women. Cancer Epidemiol. Biomarkers Prev. 11, 353–359 (2002).
van der Graaf, Y. et al. Human papillomavirus and the long-term risk of cervical neoplasia. Am. J. Epidemiol. 156, 158–164 (2002).
van Duin, M. et al. Human papillomavirus 16 load in normal and abnormal cervical scrapes: an indicator of CIN II/III and viral clearance. Int. J. Cancer 98, 590–595 (2002).
Chan, J. K. et al. HPV infection and number of lifetime sexual partners are strong predictors for 'natural' regression of CIN 2 and 3. Br. J. Cancer 89, 1062–1066 (2003).
Giuliano, A. R. et al. Dietary intake and risk of persistent human papillomavirus (HPV) infection: the Ludwig–McGill HPV natural history study. J. Infect. Dis. 188, 1508–1516 (2003).
Cuschieri, K. S., Whitley, M. J. & Cubie, H. A. Human papillomavirus type specific DNA and RNA persistence–implications for cervical disease progression and monitoring. J. Med. Virol. 73, 65–70 (2004).
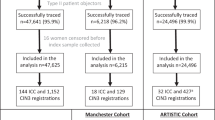
Peto, J. et al. Cervical HPV infection and neoplasia in a large population-based prospective study: the Manchester cohort. Br. J. Cancer 91, 942–953 (2004).
Piyathilake, C. J. et al. Folate is associated with the natural history of high-risk human papillomaviruses. Cancer Res. 64, 8788–8793 (2004).
Wang, S. S. et al. Validation of p16INK4a as a marker of oncogenic human papillomavirus infection in cervical biopsies from a population-based cohort in Costa Rica. Cancer Epidemiol. Biomarkers Prev. 13, 1355–1360 (2004).
Lillo, F. B. et al. Determination of human papillomavirus (HPV) load and type in high-grade cervical lesions surgically resected from HIV-infected women during follow-up of HPV infection. Clin. Infect. Dis. 40, 451–457 (2005).
Moscicki, A. B. et al. Risks for incident human papillomavirus infection and low-grade squamous intraepithelial lesion development in young females. JAMA 285, 2995–3002 (2001).
Woodman, C. B. & Collins, S. A critique of cohort studies examining the role of human papillomavirus infection in cervical neoplasia. BJOG 109, 1311–1318 (2002).
Rothman, K. J. & Greenland, S. in Modern Epidemiology 2nd edn (eds Rothman, K.J., Greenland, S.), 79–91 (Lippincott–Raven, Philadelphia, 1998).
Winer, R. L. et al. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am. J. Epidemiol. 157, 218–226 (2003).
Hall, S. et al. Human papillomavirus DNA detection in cervical specimens by hybrid capture: correlation with cytologic and histologic diagnoses of squamous intraepithelial lesions of the cervix. Gynecol. Oncol. 62, 353–359 (1996).
Nindl, I. et al. Human papillomavirus distribution in cervical tissues of different morphology as determined by hybrid capture assay and PCR. Int. J. Gynecol. Pathol. 16, 197–204 (1997).
Ho, G. Y. et al. Viral characteristics of human papillomavirus infection and antioxidant levels as risk factors for cervical dysplasia. Int. J. Cancer 78, 594–599 (1998).
Swan, D. C. et al. Human papillomavirus (HPV) DNA copy number is dependent on grade of cervical disease and HPV type. J. Clin. Microbiol. 37, 1030–1034 (1999).
Heard, I. et al. Increased risk of cervical disease among human immunodeficiency virus-infected women with severe immunosuppression and high human papillomavirus load(1). Obstet. Gynecol. 96, 403–409 (2000).
Crum, C. P. et al. Dynamics of human papillomavirus infection between biopsy and excision of cervical intraepithelial neoplasia: results from the ZYC101a protocol. J. Infect. Dis. 189, 1348–1354 (2004).
Cricca, M. et al. HPV DNA patterns and disease implications in the follow-up of patients treated for HPV16 high-grade carcinoma in situ. J. Med. Virol. 78, 494–500 (2006).
Berumen, J., Unger, E. R., Casas, L. & Figueroa, P. Amplification of human papillomavirus types 16 and 18 in invasive cervical cancer. Hum. Pathol. 26, 676–681 (1995).
Jeon, S., Allen-Hoffmann, B. L. & Lambert, P. F. Integration of human papillomavirus type 16 into the human genome correlates with a selective growth advantage of cells. J. Virol. 69, 2989–2997 (1995). This is an important paper in that it is consistent with the hypothesis that integration might provide a selective growth advantage for the epithelial precursors of cervical cancer.
Spartz, H., Lehr, E., Zhang, B., Roman, A. & Brown, D. R. Progression from productive infection to integration and oncogenic transformation in human papillomavirus type 59-immortalized foreskin keratinocytes. Virology 336, 11–25 (2005).
Sherman, M. E. et al. Determinants of human papillomavirus load among women with histological cervical intraepithelial neoplasia 3: dominant impact of surrounding low-grade lesions. Cancer Epidemiol. Biomarkers Prev. 12, 1038–1044 (2003).
Gravitt, P. E. et al. A comparison between real-time polymerase chain reaction and hybrid capture 2 for human papillomavirus DNA quantitation. Cancer Epidemiol. Biomarkers Prev. 12, 477–484 (2003). Using real-time PCR this study shows, how the relationship between viral load and disease varies with the infecting HPV type.
Ho, C. M. et al. Detection and quantitation of human papillomavirus type 16, 18 and 52 DNA in the peripheral blood of cervical cancer patients. Gynecol. Oncol. 99, 615–621 (2005).
Woodman, C. B. et al. Human papillomavirus type 18 and rapidly progressing cervical intraepithelial neoplasia. Lancet 361, 40–43 (2003).
Mitchell, H., Medley, G., Gordon, I. & Giles, G. Cervical cytology reported as negative and risk of adenocarcinoma of the cervix: no strong evidence of benefit. Br. J. Cancer 71, 894–897 (1995).
Kovacic, M. B. et al. Relationships of human papilloma-virus type, qualitative viral load, and age with cytologic abnormality. Cancer Res. 66, 10112–10119 (2006).
Jeon, S. & Lambert, P. F. Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc. Natl Acad. Sci. USA 92, 1654–1658 (1995).
Andersson, S. et al. Type distribution, viral load and integration status of high-risk human papillomaviruses in pre-stages of cervical cancer (CIN). Br. J. Cancer 92, 2195–2200 (2005).
Peitsaro, P., Johansson, B. & Syrjanen, S. Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J. Clin. Microbiol. 40, 886–891 (2002).
Choo, K. B., Pan, C. C. & Han, S. H. Integration of human papillomavirus type 16 into cellular DNA of cervical carcinoma: preferential deletion of the E2 gene and invariable retention of the long control region and the E6/E7 open reading frames. Virology 161, 259–261 (1987).
Meanwell, C. A., Cox, M. F., Blackledge, G. & Maitland, N. J. HPV 16 DNA in normal and malignant cervical epithelium: implications for the aetiology and behaviour of cervical neoplasia. Lancet 1, 703–707 (1987).
Fuchs, P. G., Girardi, F. & Pfister, H. Human papillomavirus 16 DNA in cervical cancers and in lymph nodes of cervical cancer patients: a diagnostic marker for early metastases? Int. J. Cancer 43, 41–44 (1989).
Matsukura, T., Koi, S. & Sugase, M. Both episomal and integrated forms of human papillomavirus type 16 are involved in invasive cervical cancers. Virology 172, 63–72 (1989).
Cooper, K., Herrington, C. S., Graham, A. K., Evans, M. F. & McGee, J. O. In situ evidence for HPV 16, 18, 33 integration in cervical squamous cell cancer in Britain and South Africa. J. Clin. Pathol. 44, 406–409 (1991).
Cullen, A. P., Reid, R., Campion, M. & Lorincz, A. T. Analysis of the physical state of different human papillomavirus DNAs in intraepithelial and invasive cervical neoplasm. J. Virol. 65, 606–612 (1991).
Cooper, K., Herrington, C. S., Lo, E. S., Evans, M. F. & McGee, J. O. Integration of human papillomavirus types 16 and 18 in cervical adenocarcinoma. J. Clin. Pathol. 45, 382–384 (1992).
Das, B. C., Sharma, J. K., Gopalakrishna, V. & Luthra, U. K. Analysis by polymerase chain reaction of the physical state of human papillomavirus type 16 DNA in cervical preneoplastic and neoplastic lesions. J. Gen. Virol. 73, 2327–2336 (1992).
Chen, C. M. et al. Analysis of deletion of the integrated human papillomavirus 16 sequence in cervical cancer: a rapid multiplex polymerase chain reaction approach. J. Med. Virol. 44, 206–211 (1994).
Kristiansen, E., Jenkins, A. & Holm, R. Coexistence of episomal and integrated HPV16 DNA in squamous cell carcinoma of the cervix. J. Clin. Pathol. 47, 253–256 (1994).
Daniel, B., Mukherjee, G., Seshadri, L., Vallikad, E. & Krishna, S. Changes in the physical state and expression of human papillomavirus type 16 in the progression of cervical intraepithelial neoplasia lesions analysed by PCR. J. Gen. Virol. 76, 2589–2593 (1995).
Unger, E. R. et al. Human papillomavirus and disease-free survival in FIGO stage Ib cervical cancer. J. Infect. Dis. 172, 1184–1190 (1995).
Park, J. S. et al. Physical status and expression of HPV genes in cervical cancers. Gynecol. Oncol. 65, 121–129 (1997).
Pirami, L., Giache, V. & Becciolini, A. Analysis of HPV16, 18, 31, and 35 DNA in pre-invasive and invasive lesions of the uterine cervix. J. Clin. Pathol. 50, 600–604 (1997).
Vernon, S. D., Unger, E. R., Miller, D. L., Lee, D. R. & Reeves, W. C. Association of human papillomavirus type 16 integration in the E2 gene with poor disease-free survival from cervical cancer. Int. J. Cancer 74, 50–56 (1997).
Kalantari, M. et al. Disruption of the E1 and E2 reading frames of HPV 16 in cervical carcinoma is associated with poor prognosis. Int. J. Gynecol. Pathol. 17, 146–153 (1998).
Casas, L. et al. Asian-american variants of human papillomavirus type 16 have extensive mutations in the E2 gene and are highly amplified in cervical carcinomas. Int. J. Cancer 83, 449–455 (1999).
Corden, S. A., Sant-Cassia, L. J., Easton, A. J. & Morris, A. G. The integration of HPV-18 DNA in cervical carcinoma. Mol. Pathol. 52, 275–282 (1999).
Eriksson, A., Herron, J. R., Yamada, T. & Wheeler, C. M. Human papillomavirus type 16 variant lineages characterized by nucleotide sequence analysis of the E5 coding segment and the E2 hinge region. J. Gen. Virol. 80, 595–600 (1999).
Kim, C. J. et al. The antibody response to HPV proteins and the genomic state of HPVs in patients with cervical cancer. Int. J. Gynecol. Cancer 9, 1–11 (1999).
Klaes, R. et al. Detection of high-risk cervical intraepithelial neoplasia and cervical cancer by amplification of transcripts derived from integrated papillomavirus oncogenes. Cancer Res. 59, 6132–6136 (1999).
Yoshinouchi, M. et al. Analysis by multiplex PCR of the physical status of human papillomavirus type 16 DNA in cervical cancers. J. Clin. Microbiol. 37, 3514–3517 (1999).
Graham, D. A. & Herrington, C. S. HPV-16 E2 gene disruption and sequence variation in CIN 3 lesions and invasive squamous cell carcinomas of the cervix: relation to numerical chromosome abnormalities. Mol. Pathol. 53, 201–206 (2000).
Szarka, K. et al. Integration status of virus DNA and p53 codon 72 polymorphism in human papillomavirus type 16 positive cervical cancers. Anticancer Res. 20, 2161–2167 (2000).
Giannoudis, A., Duin, M., Snijders, P. J. & Herrington, C. S. Variation in the E2-binding domain of HPV 16 is associated with high-grade squamous intraepithelial lesions of the cervix. Br. J. Cancer 84, 1058–1063 (2001).
Tonon, S. A. et al. Physical status of the E2 human papilloma virus 16 viral gene in cervical preneoplastic and neoplastic lesions. J. Clin. Virol. 21, 129–134 (2001).
Evans, M. F., Mount, S. L., Beatty, B. G. & Cooper, K. Biotinyl-tyramide-based in situ hybridization signal patterns distinguish human papillomavirus type and grade of cervical intraepithelial neoplasia. Mod. Pathol. 15, 1339–1347 (2002).
Nagao, S. et al. Rapid and sensitive detection of physical status of human papillomavirus type 16 DNA by quantitative real-time PCR. J. Clin. Microbiol. 40, 863–867 (2002).
Watts, K. J., Thompson, C. H., Cossart, Y. E. & Rose, B. R. Sequence variation and physical state of human papillomavirus type 16 cervical cancer isolates from Australia and New Caledonia. Int. J. Cancer 97, 868–874 (2002).
do Horto dos Santos Oliveira, L., Rodrigues Ede, V., de Salles Lopes, A. P., Fernandez Ade, P. & Cavalcanti, S. M. HPV 16 detection in cervical lesions, physical state of viral DNA and changes in p53 gene. Sao Paulo Med. J. 121, 67–71 (2003).
Gallo, G. et al. Study of viral integration of HPV-16 in young patients with LSIL. J. Clin. Pathol. 56, 532–536 (2003).
Lukaszuk, K., Liss, J., Wozniak, I., Emerich, J. & Wojcikowski, C. Human papillomavirus type 16 status in cervical carcinoma cell DNA assayed by multiplex PCR. J. Clin. Microbiol. 41, 608–612 (2003).
Alazawi, W. et al. Genomic imbalances in 70 snap-frozen cervical squamous intraepithelial lesions: associations with lesion grade, state of the HPV16 E2 gene and clinical outcome. Br. J. Cancer 91, 2063–2070 (2004). This is an interesting paper that shows a high prevalence of integrated forms in women with cervical intraepithelial neoplasia.
Hudelist, G. et al. Physical state and expression of HPV DNA in benign and dysplastic cervical tissue: different levels of viral integration are correlated with lesion grade. Gynecol. Oncol. 92, 873–880 (2004).
Sathish, N. et al. Human papillomavirus 16 E6/E7 transcript and E2 gene status in patients with cervical neoplasia. Mol. Diagn. 8, 57–64 (2004).
Chen, Q. Y., Bian, M. L., Chen, Z. H. & Liu, J. Detection of integration status of human papillomavirus 16 in cervical precancerous lesions. Zhonghua Yi Xue Za Zhi 85, 400–404 (2005).
Swan, D. C. et al. Human papillomavirus type 16 E2 and E6/E7 variants. Gynecol. Oncol. 96, 695–700 (2005).
Arias-Pulido, H., Peyton, C. L., Joste, N. E., Vargas, H. & Wheeler, C. M. Human papillomavirus type 16 integration in cervical carcinoma in situ and in invasive cervical cancer. J. Clin. Microbiol. 44, 1755–1762 (2006). This paper is interesting in that it shows that real-time PCR assays can only distinguish integrated forms in the presence of episomal forms when they are at least 100 times as common.
Bhattacharjee, B. & Sengupta, S. HPV16 E2 gene disruption and polymorphisms of E2 and LCR: some significant associations with cervical cancer in Indian women. Gynecol. Oncol. 100, 372–378 (2006).
Bryan, J. T. et al. Detection of specific human papillomavirus types in paraffin-embedded sections of cervical carcinomas. J. Med. Virol. 78, 117–124 (2006).
Ho, C. M., Chien, T. Y., Huang, S. H., Lee, B. H. & Chang, S. F. Integrated human papillomavirus types 52 and 58 are infrequently found in cervical cancer, and high viral loads predict risk of cervical cancer. Gynecol. Oncol. 102, 54–60 (2006).
Kulmala, S. M. et al. Early integration of high copy HPV16 detectable in women with normal and low grade cervical cytology and histology. J. Clin. Pathol. 59, 513–517 (2006).
Zheng, Y., Peng, Z. L., Lou, J. Y. & Wang, H. Detection of physical status of human papillomavirus 16 in cervical cancer tissue and SiHa cell line by multiplex real-time polymerase chain reaction. Ai Zheng 25, 373–377 (2006).
Vinokurova, S. et al. Clonal history of papillomavirus-induced dysplasia in the female lower genital tract. J. Natl Cancer Inst. 97, 1816–1821 (2005).
Wilke, C. M. et al. FRA3B extends over a broad region and contains a spontaneous HPV16 integration site: direct evidence for the coincidence of viral integration sites and fragile sites. Hum. Mol. Genet. 5, 187–195 (1996).
Thorland, E. C. et al. Human papillomavirus type 16 integrations in cervical tumors frequently occur in common fragile sites. Cancer Res. 60, 5916–5921 (2000).
Ferber, M. J. et al. Integrations of the hepatitis B virus (HBV) and human papillomavirus (HPV) into the human telomerase reverse transcriptase (hTERT) gene in liver and cervical cancers. Oncogene 22, 3813–3820 (2003).
Ferber, M. J. et al. Preferential integration of human papillomavirus type 18 near the c-MYC locus in cervical carcinoma. Oncogene 22, 7233–7242 (2003).
Thorland, E. C., Myers, S. L., Gostout, B. S. & Smith, D. I. Common fragile sites are preferential targets for HPV16 integrations in cervical tumors. Oncogene 22, 1225–1237 (2003).
Ferber, M. J. et al. Positioning of cervical carcinoma and Burkitt lymphoma translocation breakpoints with respect to the human papillomavirus integration cluster in FRA8C at 8q24.13. Cancer Genet. Cytogenet. 154, 1–9 (2004).
Yu, T. et al. The role of viral integration in the development of cervical cancer. Cancer Genet. Cytogenet. 158, 27–34 (2005).
Wentzensen, N. et al. Characterization of viral-cellular fusion transcripts in a large series of HPV16 and 18 positive anogenital lesions. Oncogene 21, 419–426 (2002).
Ziegert, C. et al. A comprehensive analysis of HPV integration loci in anogenital lesions combining transcript and genome-based amplification techniques. Oncogene 22, 3977–3984 (2003).
Wentzensen, N., Vinokurova, S. & von Knebel Doeberitz, M. Systematic review of genomic integration sites of human papillomavirus genomes in epithelial dysplasia and invasive cancer of the female lower genital tract. Cancer Res. 64, 3878–3884 (2004). This is an important review of the sites of HPV integration into the human genome.
Peter, M. et al. MYC activation associated with the integration of HPV DNA at the MYC locus in genital tumors. Oncogene 25, 5985–5993 (2006). This paper describes transcriptional and protein overexpression of MYC associated with HPV16 or HPV18 integration at 8q24, which includes the MYC locus.
Melsheimer, P., Vinokurova, S., Wentzensen, N., Bastert, G. & von Knebel Doeberitz, M. DNA aneuploidy and integration of human papillomavirus type 16 E6/-E7 oncogenes in intraepithelial neoplasia and invasive squamous cell carcinoma of the cervix uteri. Clin. Cancer Res. 10, 3059–3063 (2004).
Pett, M. R. et al. Selection of cervical keratinocytes containing integrated HPV16 associates with episome loss and an endogenous antiviral response. Proc. Natl Acad. Sci. USA 103, 3822–3827 (2006). This paper offers an interesting hypothesis: it proposes that it is the loss of episomal E2 in cells in which integration has already occurred that confers the growth advantage on selected cells.
Bechtold, V., Beard, P. & Raj, K. Human papillomavirus type 16 E2 protein has no effect on transcription from episomal viral DNA. J. Virol. 77, 2021–2028 (2003).
Herdman, M. T. et al. Interferon-β treatment of cervical keratinocytes naturally infected with human papillomavirus 16 episomes promotes rapid reduction in episome numbers and emergence of latent integrants. Carcinogenesis 27, 2341–2353 (2006).
Kjaer, S. K. et al. Acquisition and persistence of human papillomavirus infection in younger men: a prospective follow-up study among Danish soldiers. Cancer Epidemiol. Biomarkers Prev. 14, 1528–1533 (2005).
Lajous, M. et al. Determinants of prevalence, acquisition, and persistence of human papillomavirus in healthy mexican military men. Cancer Epidemiol. Biomarkers Prev. 14, 1710–1716 (2005).
Giuliano, A. R., Papenfuss, M., Abrahamsen, M. & Inserra, P. Differences in factors associated with oncogenic and nononcogenic human papillomavirus infection at the United States-Mexico border. Cancer Epidemiol. Biomarkers Prev. 11, 930–934 (2002).
Rousseau, M. C. et al. Predictors of cervical coinfection with multiple human papillomavirus types. Cancer Epidemiol. Biomarkers Prev. 12, 1029–1037 (2003).
Weissenborn, S. J. et al. Oncogenic human papillomavirus DNA loads in human immunodeficiency virus-positive women with high-grade cervical lesions are strongly elevated. J. Clin. Microbiol. 41, 2763–2767 (2003).
Badaracco, G. & Venuti, A. Physical status of HPV types 16 and 18 in topographically different areas of genital tumours and in paired tumour-free mucosa. Int. J. Oncol. 27, 161–167 (2005). This paper indicates that the integration status of HPV16 might vary with the presence or absence of HPV18.
Kim, K., Garner-Hamrick, P. A., Fisher, C., Lee, D. & Lambert, P. F. Methylation patterns of papillomavirus DNA, its influence on E2 function, and implications in viral infection. J. Virol. 77, 12450–12459 (2003).
Badal, S. et al. The human papillomavirus-18 genome is efficiently targeted by cellular DNA methylation. Virology 324, 483–492 (2004).
Kalantari, M. et al. Conserved methylation patterns of human papillomavirus type 16 DNA in asymptomatic infection and cervical neoplasia. J. Virol. 78, 12762–12772 (2004).
Turan, T. et al. Methylation of the human papillomavirus-18 L1 gene: a biomarker of neoplastic progression? Virology 349, 175–183 (2006).
Remus, R. et al. Insertion of foreign DNA into an established mammalian genome can alter the methylation of cellular DNA sequences. J. Virol. 73, 1010–1022 (1999).
Badal, V. et al. CpG methylation of human papillomavirus type 16 DNA in cervical cancer cell lines and in clinical specimens: genomic hypomethylation correlates with carcinogenic progression. J. Virol. 77, 6227–6234 (2003).
Van Tine, B. A. et al. Clonal selection for transcriptionally active viral oncogenes during progression to cancer. J. Virol. 78, 11172–11186 (2004).
Esteller, M. Epigenetics provides a new generation of oncogenes and tumour-suppressor genes. Br. J. Cancer 94, 179–183 (2006).
Kang, G. H. et al. Epstein-Barr virus-positive gastric carcinoma demonstrates frequent aberrant methylation of multiple genes and constitutes CpG island methylator phenotype-positive gastric carcinoma. Am. J. Pathol. 160, 787–794 (2002).
Vo, Q. N. et al. Epstein-Barr virus in gastric adenocarcinomas: association with ethnicity and CDKN2A promoter methylation. J. Clin. Pathol. 55, 669–675 (2002).
Yang, B., Guo, M., Herman, J. G. & Clark, D. P. Aberrant promoter methylation profiles of tumor suppressor genes in hepatocellular carcinoma. Am. J. Pathol. 163, 1101–1107 (2003).
Li, X. et al. p16INK4A hypermethylation is associated with hepatitis virus infection, age, and gender in hepatocellular carcinoma. Clin. Cancer Res. 10, 7484–7489 (2004).
Sakuma, K. et al. High-density methylation of p14ARF and p16INK4A in Epstein-Barr virus-associated gastric carcinoma. Int. J. Cancer 112, 273–278 (2004).
Sudo, M. et al. Promoter hypermethylation of E-cadherin and its abnormal expression in Epstein-Barr virus-associated gastric carcinoma. Int. J. Cancer 109, 194–199 (2004).
Kim, N. R., Lin, Z., Kim, K. R., Cho, H. Y. & Kim, I. Epstein-Barr virus and p16INK4A methylation in squamous cell carcinoma and precancerous lesions of the cervix uteri. J. Korean Med. Sci. 20, 636–642 (2005).
Suzuki, M. et al. Aberrant methylation profile of human malignant mesotheliomas and its relationship to SV40 infection. Oncogene 24, 1302–1308 (2005).
Chang, M. S. et al. CpG island methylation status in gastric carcinoma with and without infection of Epstein-Barr virus. Clin. Cancer Res. 12, 2995–3002 (2006).
Jicai, Z. et al. Persistent infection of hepatitis B virus is involved in high rate of p16 methylation in hepatocellular carcinoma. Mol. Carcinog. 45, 530–536 (2006).
Katoh, H. et al. Epigenetic instability and chromosomal instability in hepatocellular carcinoma. Am. J. Pathol. 168, 1375–1384 (2006).
Kusano, M. et al. Genetic, epigenetic, and clinicopathologic features of gastric carcinomas with the CpG island methylator phenotype and an association with Epstein-Barr virus. Cancer 106, 1467–1479 (2006).
O'Nions, J. et al. p73 is over-expressed in vulval cancer principally as the δ 2 isoform. Br. J. Cancer 85, 1551–1556 (2001).
Gasco, M. et al. Epigenetic inactivation of 14-3-3 σ in oral carcinoma: association with p16(INK4a) silencing and human papillomavirus negativity. Cancer Res. 62, 2072–2076 (2002).
Dong, S. M. et al. Epigenetic inactivation of RASSF1A in head and neck cancer. Clin. Cancer Res. 9, 3635–3640 (2003).
Marsit, C. J., McClean, M. D., Furniss, C. S. & Kelsey, K. T. Epigenetic inactivation of the SFRP genes is associated with drinking, smoking and HPV in head and neck squamous cell carcinoma. Int. J. Cancer 119, 1761–1766 (2006). This paper draws attention to an interaction between smoking and HPV16 infection, and promoter methylation at another HPV-associated site of cancer.
Santin, A. D. et al. Gene expression profiles of primary HPV16- and HPV18-infected early stage cervical cancers and normal cervical epithelium: identification of novel candidate molecular markers for cervical cancer diagnosis and therapy. Virology 331, 269–291 (2005).
Wilting, S. M. et al. Increased gene copy numbers at chromosome 20q are frequent in both squamous cell carcinomas and adenocarcinomas of the cervix. J. Pathol. 209, 220–230 (2006).
Tsai, C. N., Tsai, C. L., Tse, K. P., Chang, H. Y. & Chang, Y. S. The Epstein-Barr virus oncogene product, latent membrane protein 1, induces the downregulation of E-cadherin gene expression via activation of DNA methyltransferases. Proc. Natl Acad. Sci. USA 99, 10084–10089 (2002).
Etoh, T. et al. Increased DNA methyltransferase 1 (DNMT1) protein expression correlates significantly with poorer tumor differentiation and frequent DNA hypermethylation of multiple CpG islands in gastric cancers. Am. J. Pathol. 164, 689–699 (2004).
Lee, J. O. et al. Hepatitis B virus X protein represses E-cadherin expression via activation of DNA methyltransferase 1. Oncogene 24, 6617–6625 (2005).
Li, H. P., Leu, Y. W. & Chang, Y. S. Epigenetic changes in virus-associated human cancers. Cell Res. 15, 262–271 (2005).
Liu, J. et al. Downregulation of E-cadherin by hepatitis B virus X antigen in hepatocellullar carcinoma. Oncogene 25, 1008–1017 (2006).
Burgers, W. A. et al. Viral oncoproteins target the DNA methyltransferases. Oncogene 18 Sep 2006 (doi: 10./sj.onc.1209950). This is an important paper that shows that HPV oncogenes can activate DNA methyltransferases.
Robertson, K. D. et al. DNMT1 forms a complex with RB, E2F1 and HDAC1 and represses transcription from E2F-responsive promoters. Nature Genet. 25, 338–342 (2000).
McCabe, M. T., Davis, J. N. & Day, M. L. Regulation of DNA methyltransferase 1 by the pRb/E2F1 pathway. Cancer Res. 65, 3624–3632 (2005).
McCabe, M. T., Low, J. A., Imperiale, M. J. & Day, M. L. Human polyomavirus BKV transcriptionally activates DNA methyltransferase 1 through the pRb/E2F pathway. Oncogene 25, 2727–2735 (2006).
Uren, A. et al. Activation of the canonical Wnt pathway during genital keratinocyte transformation: a model for cervical cancer progression. Cancer Res. 65, 6199–6206 (2005).
Yukawa, K., Butz, K., Yasui, T., Kikutani, H. & Hoppe-Seyler, F. Regulation of human papillomavirus transcription by the differentiation-dependent epithelial factor Epoc-1/skn-1a. J. Virol. 70, 10–16 (1996).
Sun, S. & Steinberg, B. M. PTEN is a negative regulator of STAT3 activation in human papillomavirus-infected cells. J. Gen. Virol. 83, 1651–1658 (2002).
Kamio, M. et al. SOCS1 inhibits HPV-E7-mediated transformation by inducing degradation of E7 protein. Oncogene 23, 3107–3115 (2004).
Liu, L. et al. A methylation profile of in vitro immortalized human cell lines. Int. J. Oncol. 26, 275–285 (2005).
Gustafson, K. S., Furth, E. E., Heitjan, D. F., Fansler, Z. B. & Clark, D. P. DNA methylation profiling of cervical squamous intraepithelial lesions using liquid-based cytology specimens: an approach that utilizes receiver-operating characteristic analysis. Cancer 102, 259–268 (2004). This study shows how the detection of methylated forms in cervical material might assist in the triage of women with cytological abnormality.
Maliukova, A. V. et al. Methylation of the putative tumor suppressor gene, RASSF1A, in primary cervical tumors. Mol. Biol. (Mosk.) 38, 1005–1013 (2004).
Chan, A. O. et al. Eradication of Helicobacter pylori infection reverses E-cadherin promoter hypermethylation. Gut 55, 463–468 (2006). This study reports how the effective treatment of an infectious agent can reverse the hypermethylation of a TSG.
Acknowledgements
We gratefully acknowledge the support of Cancer Research UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Lawrence S. Young has a paid consultancy with Glaxo Smith Kline.
Supplementary information
Related links
Related links
DATABASES
National Cancer Institute
FURTHER INFORMATION
Glossary
- Adenocarcinoma
-
A malignant tumour originating in glandular tissue.
- Cross-sectional study
-
A study examining the association between disease and exposure at one point in time (a prevalence study). The temporal sequence of cause and effect cannot be determined with this study design.
- Episome
-
A piece of hereditary material that can exist as free, autonomously replicating DNA.
- Cervical intraepithelial neoplasia
-
(CIN) A disease characterized by precancerous changes in, and confined to, the epithelial cells lining the cervix.
- Dysplasia
-
An epithelial abnormality in which the cells becomes disorganized, which is charac-terized by developmental changes in cell growth, shape and organization.
- Natural history
-
The course of disease or infection from onset to resolution.
- Epigenetic
-
Inherited changes in gene expression resulting from altered chromatin structure or DNA modification rather than changes in DNA sequence.
- Latent infection
-
The persistence of an infection in a host without symptoms and/or without being detectable.
- Incident
-
A new occurrence of disease or infection in someone previously free of disease or infection.
- Longitudinal study
-
A study in which subjects are followed over a period of time so that the temporal sequence of potential cause and effect can be established.
- Triage
-
The classification of patients according to priority of need.
- Squamous intraepithelial lesion
-
(SIL). A disease characterized by the abnormal growth of squamous cells on the surface of the cervix. It is classified cytologically as low-grade (LSIL) or high-grade (HSIL) according to how much of the cervix is affected and how abnormal the cells are.
- Colposcopy
-
The visual examination of the uterine cervix with a magnifying lens to detect abnormal cells.
- Fragile site
-
A site on a chromosome that tends to break more often than other sites.
- Insertional mutagenesis
-
The occurrence of a mutation that is caused by the introduction of foreign DNA sequences into a gene.
- Keratinocyte
-
An epidermal cell that produces the protein keratin.
- CpG island
-
A region of genomic DNA in which the frequency of the CG sequence is higher than in other regions.
- DNA methyltransferase
-
An enzyme that transfers a methyl group to DNA. DNMT1 is the most abundant methyltransferase and is the main maintenance methyltransferase. DNMT3A and DNMT3B are the main de novo methyltransferases.
- Pocket protein
-
The pocket protein family includes three proteins, RB (retinoblastoma), RBL1 (retinoblastoma-like 1) and RBL2. They have a crucial role in cell-cycle regulation through interaction with the E2F transcription factors.
Rights and permissions
About this article
Cite this article
Woodman, C., Collins, S. & Young, L. The natural history of cervical HPV infection: unresolved issues. Nat Rev Cancer 7, 11–22 (2007). https://doi.org/10.1038/nrc2050
Issue Date:
DOI: https://doi.org/10.1038/nrc2050
This article is cited by
-
The interplay between human papillomavirus and vaginal microbiota in cervical cancer development
Virology Journal (2023)
-
Identification of a methylation panel as an alternative triage to detect CIN3+ in hrHPV-positive self-samples from the population-based cervical cancer screening programme
Clinical Epigenetics (2023)
-
Regulatory T cell frequency in peripheral blood of women with advanced cervical Cancer including women living with HIV
BMC Cancer (2023)
-
Carcinogenesis and management of human papillomavirus-associated cervical cancer
International Journal of Clinical Oncology (2023)
-
Role of Host Cervicovaginal Microbiota in Persistence of High-Risk HPV Infection in Women Attending Gynecology Outpatient Department in a Tertiary Hospital
Indian Journal of Gynecologic Oncology (2023)