Abstract
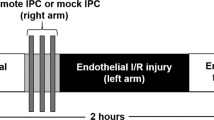
Novel approaches are required to improve clinical outcomes in patients with coronary heart disease (CHD). Ischemic conditioning—the practice of applying brief episodes of nonlethal ischemia and reperfusion to confer protection against a sustained episode of lethal ischemia and reperfusion injury—is one potential therapeutic strategy. Importantly, the protective stimulus can be applied before (ischemic preconditioning) or after (ischemic perconditioning) onset of the sustained episode of lethal ischemia, or even at the onset of myocardial reperfusion (ischemic postconditioning). Furthermore, the protective stimulus can be applied noninvasively by placing a blood-pressure cuff on an upper or lower limb to induce brief episodes of nonlethal ischemia and reperfusion (remote ischemic conditioning), a finding that has greatly facilitated the translation of ischemic conditioning to various clinical settings. In addition to mechanical approaches, elucidation of the signal-transduction pathways underlying ischemic conditioning has identified several novel targets for pharmacological conditioning. This Review highlights findings from proof-of-concept clinical studies conducted in the past 5–6 years, in which the therapeutic potential of ischemic and pharmacological conditioning has been realized. Large, randomized, controlled trials are now required to determine whether pharmacological and ischemic conditioning improve clinical end points and outcomes in patients with CHD.
Key Points
-
Ischemic conditioning describes an endogenous phenomenon, in which one or more brief episodes of nonlethal ischemia and reperfusion confer protection against a sustained lethal episode of ischemia and reperfusion
-
The conditioning stimulus can be applied before (ischemic preconditioning) or after the onset of (ischemic perconditioning) ischemia, or at the transition from sustained ischemia to reperfusion (ischemic postconditioning)
-
The conditioning stimulus can, moreover, be applied either directly to the heart or to a distant organ or tissue, such as a limb (remote ischemic conditioning)
-
Elucidation of the mechanistic pathways underlying ischemic conditioning has identified potential pharmacological cardioprotective strategies (pharmacological conditioning), which have been largely unsuccessful in the clinical setting
-
Proof-of-concept studies reported benefits with ischemic perconditioning, postconditioning, and remote ischemic conditioning in patients with acute myocardial infarction, and those undergoing cardiac surgery or percutaneous coronary intervention
-
Large, multicenter, randomized, placebo-controlled, clinical trials are now required to determine whether ischemic conditioning can improve clinical outcomes in patients with coronary heart disease
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Braunwald, E. & Kloner, R. A. Myocardial reperfusion: a double-edged sword? J. Clin. Invest 76, 1713–1719 (1985).
Yellon, D. M. & Hausenloy, D. J. Myocardial reperfusion injury. N. Engl. J Med. 357, 1121–1135 (2007).
Murry, C. E., Jennings, R. B. & Reimer, K. A. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 74, 1124–1136 (1986).
Schulz, R., Cohen, M. V., Behrends, M., Downey, J. M. & Heusch, G. Signal transduction of ischemic preconditioning. Cardiovasc. Res. 52, 181–198 (2001).
Yellon, D. M. & Downey, J. M. Preconditioning the myocardium: from cellular physiology to clinical cardiology. Physiol. Rev. 83, 1113–1151 (2003).
Downey, J. M., Davis, A. M. & Cohen, M. V. Signaling pathways in ischemic preconditioning. Heart Fail. Rev. 12, 181–188 (2007).
Ovize, M. et al. Postconditioning and protection from reperfusion injury: where do we stand? Position paper from the Working Group of Cellular Biology of the Heart of the European Society of Cardiology. Cardiovasc. Res. 87, 406–423 (2010).
Heusch, G. Postconditioning: old wine in a new bottle? J. Am. Coll. Cardiol. 44, 1111–1112 (2004).
Heusch, G., Boengler, K. & Schulz, R. Cardioprotection: nitric oxide, protein kinases, and mitochondria. Circulation 118, 1915–1919 (2008).
Hausenloy, D. J. Signalling pathways in ischaemic postconditioning. Thromb. Haemost. 101, 626–634 (2009).
Hausenloy, D. J. & Yellon, D. M. Remote ischaemic preconditioning: underlying mechanisms and clinical application. Cardiovasc Res. 79, 377–386 (2008).
Hausenloy, D. J. & Yellon, D. M. The second window of preconditioning (SWOP) where are we now? Cardiovasc. Drugs Ther. 24, 235–254 (2010).
Gülker, H., Krämer, B., Stephan, K. & Meesmann, W. Changes in ventricular fibrillation threshold during repeated short-term coronary occlusion and release. Basic Res. Cardiol. 72, 547–562 (1977).
Marber, M. S., Latchman, D. S., Walker, J. M. & Yellon, D. M. Cardiac stress protein elevation 24 hours after brief ischemia or heat stress is associated with resistance to myocardial infarction. Circulation 88, 1264–1272 (1993).
Kuzuya, T. et al. Delayed effects of sublethal ischemia on the acquisition of tolerance to ischemia. Circ. Res. 72, 1293–1299 (1993).
Przyklenk, K., Bauer, B., Ovize, M., Kloner, R. A. & Whittaker, P. Regional ischemic 'preconditioning' protects remote virgin myocardium from subsequent sustained coronary occlusion. Circulation 87, 893–899 (1993).
Gho, B. C., Schoemaker, R. G., van den Doel, M. A., Duncker, D. J. & Verdouw, P. D. Myocardial protection by brief ischemia in noncardiac tissue. Circulation 94, 2193–2200 (1996).
Birnbaum, Y., Hale, S. L. & Kloner, R. A. Ischemic preconditioning at a distance: reduction of myocardial infarct size by partial reduction of blood supply combined with rapid stimulation of the gastrocnemius muscle in the rabbit. Circulation 96, 1641–1646 (1997).
Kharbanda, R. K. et al. Transient limb ischemia induces remote ischemic preconditioning in vivo. Circulation 106, 2881–2883 (2002).
Schmidt, M. R. et al. Intermittent peripheral tissue ischemia during coronary ischemia reduces myocardial infarction through a KATP-dependent mechanism: first demonstration of remote ischemic perconditioning. Am. J. Physiol. Heart Circ. Physiol. 292, H1883–H1890 (2007).
Andreka, G. et al. Remote ischaemic postconditioning protects the heart during acute myocardial infarction in pigs. Heart 93, 749–752 (2007).
Heusch, G. & Schulz, R. Remote preconditioning. J. Mol. Cell Cardiol. 34, 1279–1281 (2002).
Lim, S. Y., Yellon, D. M. & Hausenloy, D. J. The neural and humoral pathways in remote limb ischemic preconditioning. Basic Res. Cardiol. 105, 651–655 (2010).
Na, H. S. et al. Ventricular premature beat-driven intermittent restoration of coronary blood flow reduces the incidence of reperfusion-induced ventricular fibrillation in a cat model of regional ischemia. Am. Heart J. 132 (Pt 1), 78–83 (1996).
Zhao, Z. Q. et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am. J. Physiol. Heart Circ. Physiol. 285, H579–H588 (2003).
Yellon, D. M. & Opie, L. H. Postconditioning for protection of the infarcting heart. Lancet 367, 456–458 (2006).
Staat, P. et al. Postconditioning the human heart. Circulation 112, 2143–2148 (2005).
Botker, H. E. et al. Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet 375, 727–734 (2010).
Sörensson, P. et al. Effect of postconditioning on infarct size in patients with ST elevation myocardial infarction. Heart 96, 1710–1715 (2010).
Hausenloy, D. J. et al. Translating novel strategies for cardioprotection: the Hatter Workshop Recommendations. Basic Res. Cardiol. 105, 677–686 (2010).
Thibault, H. et al. Long-term benefit of postconditioning. Circulation 117, 1037–1044 (2008).
Limalanathan, S. et al. Rationale and design of the POSTEMI (postconditioning in ST-elevation myocardial infarction) study. Cardiology 116, 103–109 (2010).
Tarantini, G. et al. Design and methodologies of the POSTconditioning during coronary angioplasty in acute myocardial infarction (POST-AMI) trial. Cardiology 116, 110–116 (2010).
Rentoukas, I. et al. Cardioprotective role of remote ischemic periconditioning in primary percutaneous coronary intervention: enhancement by opioid action. JACC Cardiovasc. Interv. 3, 49–55 (2010).
Selvanayagam, J. B., Searle, N., Neubauer, S. & Taggart, D. P. Correlation of coronary artery bypass surgery-related myonecrosis with grafted vessel calibre: insights from cardiovascular magnetic resonance imaging. Heart 92, 1329–1330 (2006).
Brener, S. J., Lytle, B. W., Schneider, J. P., Ellis, S. G. & Topol, E. J. Association between CK-MB elevation after percutaneous or surgical revascularization and three-year mortality. J. Am. Coll. Cardiol. 40, 1961–1967 (2002).
Fellahi, J. L. et al. Short- and long-term prognostic value of postoperative cardiac troponin I concentration in patients undergoing coronary artery bypass grafting. Anesthesiology 99, 270–274 (2003).
Lehrke, S. et al. Cardiac troponin T for prediction of short- and long-term morbidity and mortality after elective open heart surgery. Clin. Chem. 50, 1560–1567 (2004).
Croal, B. L. et al. Relationship between postoperative cardiac troponin I levels and outcome of cardiac surgery. Circulation 114, 1468–1475 (2006).
Venugopal, V., Ludman, A., Yellon, D. M. & Hausenloy, D. J. 'Conditioning' the heart during surgery. Eur. J. Cardiothorac. Surg. 35, 977–987 (2009).
Heusch, G. et al. Coronary microembolization: from bedside to bench and back to bedside. Circulation 120, 1822–1836 (2009).
Yellon, D. M., Alkhulaifi, A. M. & Pugsley, W. B. Preconditioning the human myocardium. Lancet 342, 276–277 (1993).
Jenkins, D. P. et al. Ischaemic preconditioning reduces troponin T release in patients undergoing coronary artery bypass surgery. Heart 77, 314–318 (1997).
Walsh, S. R. et al. Ischaemic preconditioning during cardiac surgery: systematic review and meta-analysis of perioperative outcomes in randomised clinical trials. Eur. J. Cardiothorac. Surg. 34, 985–994 (2008).
Cheung, M. M. et al. Randomized controlled trial of the effects of remote ischemic preconditioning on children undergoing cardiac surgery: first clinical application in humans. J. Am. Coll. Cardiol. 47, 2277–2282 (2006).
Günaydin, B. et al. Does remote organ ischaemia trigger cardiac preconditioning during coronary artery surgery? Pharmacol. Res. 41, 493–496 (2000).
Hausenloy, D. J. et al. Effect of remote ischaemic preconditioning on myocardial injury in patients undergoing coronary artery bypass graft surgery: a randomised controlled trial. Lancet 370, 575–579 (2007).
Rahman, I. A. et al. Remote ischemic preconditioning in human coronary artery bypass surgery: from promise to disappointment? Circulation 122 (Suppl.), S53–S59 (2010).
US National Library of Medicine. ClinicalTrials.gov. Effect of Remote Ischaemic Preconditioning on Clinical Outcomes in CABG Surgery (ERICCA), [online]. (2010).
US National Library of Medicine. ClinicalTrials.gov. Remote Ischaemic Preconditioning for Heart Surgery (RIPHeart-Study), [online]. (2010).
Luo, W., Li, B., Lin, G. & Huang, R. Postconditioning in cardiac surgery for tetralogy of Fallot. J. Thorac. Cardiovasc. Surg. 133, 1373–1374 (2007).
Li, B., Chen, R., Huang, R. & Luo, W. Clinical benefit of cardiac ischemic postconditioning in corrections of tetralogy of Fallot. Interact. Cardiovasc. Thorac. Surg. 8, 17–21 (2009).
Luo, W., Li, B., Chen, R., Huang, R. & Lin, G. Effect of ischemic postconditioning in adult valve replacement. Eur. J. Cardiothorac. Surg. 33, 203–208 (2008).
Cavallini, C. et al. Impact of the elevation of biochemical markers of myocardial damage on long-term mortality after percutaneous coronary intervention: results of the CK-MB and PCI study. Eur. Heart J. 26, 1494–1498 (2005).
Selvanayagam, J. B. et al. Troponin elevation after percutaneous coronary intervention directly represents the extent of irreversible myocardial injury: insights from cardiovascular magnetic resonance imaging. Circulation 111, 1027–1032 (2005).
Babu, G. G., Walker, J. M., Yellon, D. M. & Hausenloy, D. J. Peri-procedural myocardial injury during percutaneous coronary intervention: an important target for cardioprotection. Eur. Heart J. 32, 23–31 (2011).
Shimizu, M., Konstantinov, E. G., Kharbanda, R. K., Cheung, M. H. & Redington, A. N. Effects of intermittent lower limb ischaemia on coronary blood flow and coronary resistance in pigs. Acta Physiol. (Oxf.) 190, 103–109 (2007).
Zhou, K. et al. Effects of remote ischemic preconditioning on the flow pattern of the left anterior descending coronary artery in normal subjects. Int. J. Cardiol. 122, 250–251 (2007).
Hoole, S. P. et al. Remote ischemic preconditioning stimulus does not reduce microvascular resistance or improve myocardial blood flow in patients undergoing elective percutaneous coronary intervention. Angiology 60, 403–411 (2009).
Iliodromitis, E. K. et al. Increased C reactive protein and cardiac enzyme levels after coronary stent implantation. Is there protection by remote ischaemic preconditioning? Heart 92, 1821–1826 (2006).
Hoole, S. P. et al. Cardiac Remote Ischemic Preconditioning in Coronary Stenting (CRISP Stent) Study: a prospective, randomized control trial. Circulation 119, 820–827 (2009).
Piot, C. et al. Effect of cyclosporine on reperfusion injury in acute myocardial infarction. N. Engl. J. Med. 359, 473–481 (2008).
Mewton, N. et al. Effect of cyclosporine on left ventricular remodeling after reperfused myocardial infarction. J. Am. Coll. Cardiol. 55, 1200–1205 (2010).
Bolli, R. et al. Myocardial protection at a crossroads: the need for translation into clinical therapy. Circ. Res. 95, 125–134 (2004).
Kloner, R. A. & Rezkalla, S. H. Cardiac protection during acute myocardial infarction: where do we stand in 2004? J. Am. Coll. Cardiol. 44, 276–286 (2004).
Downey, J. M. & Cohen, M. V. Why do we still not have cardioprotective drugs? Circ. J. 73, 1171–1177 (2009).
Ludman, A. J., Yellon, D. M. & Hausenloy, D. J. Cardiac preconditioning for ischaemia: lost in translation. Dis. Model. Mech. 3, 35–38 (2010).
Ferdinandy, P., Schulz, R. & Baxter, G. F. Interaction of cardiovascular risk factors with myocardial ischemia/reperfusion injury, preconditioning, and postconditioning. Pharmacol. Rev. 59, 418–458 (2007).
Ali, Z. A. et al. Remote ischemic preconditioning reduces myocardial and renal injury after elective abdominal aortic aneurysm repair: a randomized controlled trial. Circulation 116 (Suppl.), I98–I105 (2007).
Venugopal, V. et al. Remote ischaemic preconditioning reduces myocardial injury in patients undergoing cardiac surgery with cold-blood cardioplegia: a randomised controlled trial. Heart 95, 1567–1571 (2009).
Hu, S. et al. Effects of remote ischemic preconditioning on biochemical markers and neurologic outcomes in patients undergoing elective cervical decompression surgery: a prospective randomized controlled trial. J. Neurosurg. Anesthesiol. 22, 46–52 (2010).
Jean-St-Michel, E. et al. Remote preconditioning improves maximal performance in highly-trained athletes. Med. Sci. Sports Exerc. doi:10.1249/MSS.0b013e318206845d.
Zhou, W. et al. Limb ischemic preconditioning reduces heart and lung injury after an open heart operation in infants. Pediatr. Cardiol. 31, 22–29 (2010).
Thielmann, M. et al. Remote ischemic preconditioning reduces myocardial injury after coronary artery bypass surgery with crystalloid cardioplegic arrest. Basic Res. Cardiol. 105, 657–664 (2010).
Wagner, R. et al. Myocardial injury is decreased by late remote ischaemic preconditioning and aggravated by tramadol in patients undergoing cardiac surgery: a randomised controlled trial. Interact. Cardiovasc. Thorac. Surg. 11, 758–762 (2010).
Hong, D. M. et al. The effect of remote ischaemic preconditioning on myocardial injury in patients undergoing off-pump coronary artery bypass graft surgery. Anaesth. Intensive Care 38, 924–929 (2010).
Ali, N., Rizwi, F., Iqbal, A. & Rashid, A. Induced remote ischemic pre-conditioning on ischemia–reperfusion injury in patients undergoing coronary artery bypass. J. Coll. Physicians Surg. Pak. 20, 427–431 (2010).
Laskey, W. K. Brief repetitive balloon occlusions enhance reperfusion during percutaneous coronary intervention for acute myocardial infarction: a pilot study. Catheter. Cardiovasc. Interv. 65, 361–367 (2005).
Ma, X., Zhang, X., Li, C. & Luo, M. Effect of postconditioning on coronary blood flow velocity and endothelial function and LV recovery after myocardial infarction. J. Interv. Cardiol. 19, 367–375 (2006).
Yang, X. C. et al. Reduction in myocardial infarct size by postconditioning in patients after percutaneous coronary intervention. J. Invasive Cardiol. 19, 424–430 (2007).
Laskey, W. K., Yoon, S., Calzada, N. & Ricciardi, M. J. Concordant improvements in coronary flow reserve and ST-segment resolution during percutaneous coronary intervention for acute myocardial infarction: a benefit of postconditioning. Catheter. Cardiovasc. Interv. 72, 212–220 (2008).
Zhao, W. S. et al. A 60-s postconditioning protocol by percutaneous coronary intervention inhibits myocardial apoptosis in patients with acute myocardial infarction. Apoptosis 14, 1204–1211 (2009).
Xue, F. et al. Postconditioning the human heart in percutaneous coronary intervention. Clin. Cardiol. 33, 439–444 (2010).
Lin, X. M. et al. Attenuation of tumor necrosis factor-α elevation and improved heart function by postconditioning for 60 seconds in patients with acute myocardial infarction. Chin. Med. J. (Engl.) 123, 1833–1839 (2010).
Lønborg, J. et al. Cardioprotective effects of ischemic postconditioning in patients treated with primary percutaneous coronary intervention, evaluated by magnetic resonance. Circ. Cardiovasc. Interv. 3, 34–41 (2010).
Garcia, S. et al. Long-term follow-up of patients undergoing postconditioning during ST-elevation myocardial infarction. J. Cardiovasc. Transl. Res. 4, 92–98 (2011).
Fan, Q. et al. Postconditioning attenuates myocardial injury by reducing nitro-oxidative stress in vivo in rats and in humans. Clin. Sci. (Lond.) 120, 251–261 (2010).
Voors, A. A. et al. A single dose of erythropoietin in ST-elevation myocardial infarction. Eur. Heart J. 31, 2593–2600 (2010).
Lipsic, E. et al. A single bolus of a long-acting erythropoietin analogue darbepoetin alfa in patients with acute myocardial infarction: a randomized feasibility and safety study. Cardiovasc. Drugs Ther. 20, 135–141 (2006).
Ozawa, T. et al. Single-dose intravenous administration of recombinant human erythropoietin is a promising treatment for patients with acute myocardial infarction —randomized controlled pilot trial of EPO/AMI-1 study. Circ. J. 74, 1415–1423 (2010).
Taniguchi, N. et al. Erythropoietin prevention trial of coronary restenosis and cardiac remodeling after ST-elevated acute myocardial infarction (EPOC-AMI): a pilot, randomized, placebo-controlled study. Circ. J. 74, 2365–2371 (2010).
Ott, I. et al. Erythropoietin in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a randomized, double-blind trial. Circ. Cardiovasc. Interv. 3, 408–413 (2010).
Najjar, S. S. et al. Intravenous erythropoietin in patients with ST-segment elevation myocardial infarction: REVEAL: a randomized clinical trial. JAMA 305, 1863–1872 (2011).
Nikolaidis, L. A. et al. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 109, 962–965 (2004).
Kitakaze, M. et al. Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (J-WIND): two randomised trials. Lancet 370, 1483–1493 (2007).
Direct Inhibition of δ-Protein Kinase C Enzyme to Limit Total Infarct Size in Acute Myocardial Infarction (DELTA MI) Investigators et al. Intracoronary KAI-9803 as an adjunct to primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction. Circulation 117, 886–896 (2008).
Kim, J. S. et al. Efficacy of high-dose atorvastatin loading before primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: the STATIN STEMI trial. JACC Cardiovasc. Interv. 3, 332–339 (2010).
Ferrario, M. et al. High-dose erythropoietin in patients with acute myocardial infarction: a pilot, randomised, placebo-controlled study. Int. J. Cardiol. 147, 124–131 (2011).
Suh, J. W. et al. The effect of intravenous administration of erythropoietin on the infarct size in primary percutaneous coronary intervention. Int. J. Cardiol. 149, 216–220 (2011).
US National Library of Medicine. ClinicalTrials.gov. Safety and Efficacy Study of KAI-9803 to Treat Subjects With ST Elevation Myocardial Infarction [Heart Attack] (PROTECTION AMI), [online]. (2011).
Acknowledgements
D. J. Hausenloy's research is funded by the British Heart Foundation (FS/10/039/28270). His work was undertaken at University College London Hospital/University College London, which received a portion of funding from the UK Department of Health's NIH Research Biomedical Research Center's funding scheme.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to all aspects of the manuscript, including researching data for the article, discussions of the content, writing the article, and review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Hausenloy, D., Yellon, D. The therapeutic potential of ischemic conditioning: an update. Nat Rev Cardiol 8, 619–629 (2011). https://doi.org/10.1038/nrcardio.2011.85
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2011.85
This article is cited by
-
Targeting PI3K/Akt in Cerebral Ischemia Reperfusion Injury Alleviation: From Signaling Networks to Targeted Therapy
Molecular Neurobiology (2024)
-
RIC in COVID-19—a Clinical Trial to Investigate Whether Remote Ischemic Conditioning (RIC) Can Prevent Deterioration to Critical Care in Patients with COVID-19
Cardiovascular Drugs and Therapy (2022)
-
Effect of Remote Ischaemic Conditioning on the Inflammatory Cytokine Cascade of COVID-19 (RIC in COVID-19): a Randomized Controlled Trial
Cardiovascular Drugs and Therapy (2022)
-
Hepatic cell mobilization for protection against ischemic myocardial injury
Scientific Reports (2021)
-
Induced neuroprotection by remote ischemic perconditioning as a new paradigm in ischemic stroke at the acute phase, a systematic review
BMC Neurology (2020)