Key Points
-
Coeliac disease is a prevalent disorder (affecting 1 in 200 Caucasian individuals) that is caused by an inappropriate immune response to gluten (which consists of the subcomponents gliadin and glutenin). The disease enters complete remission when gluten is eliminated from the diet.
-
Patients with active coeliac disease have immunoglobulin (Ig)A and IgG antibodies that are specific for the autoantigen tissue transglutaminase (TG2). The production of these antibodies is controlled by dietary exposure to gluten.
-
Coeliac disease is a complex inflammatory disorder. The environment and several genes contribute to disease development. HLA is the single most important genetic factor.
-
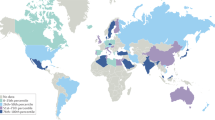
The disease is associated with HLA-DQ2 (DQA1*05/DQB1*02) in most patients, and with HLA-DQ8 (DQA1*03/DQB1*0302) in a minority of patients.
-
Gluten-specific CD4+ T cells can be isolated from the small-intestine mucosa of coeliac-disease patients, but not from non-coeliac controls. These T cells recognize gluten peptides in the context of DQ2 or DQ8, but not other HLA molecules that are expressed by patients.
-
Several gluten epitopes (both in gliadins and glutenins) exist that are recognized by mucosal T cells. Some epitopes are recognized frequently and some infrequently by the T cells of the patients.
-
Most of the gluten T-cell epitopes are recognized in a deamidated form — in other words, some specific glutamine residues have been converted to glutamic acid. This deamidation is mediated by the enzyme TG2.
-
In gliadins, the T-cell epitopes cluster in regions that are rich in proline residues. The influence of proline to protect against digestive proteolysis and to direct TG2-mediated deamidation of glutamines contributes to this epitope clustering.
-
Gluten-specific T cells might help TG2-specific B cells by linked recognition of TG2–gluten-peptide complexes. This could explain how exposure to a foreign antigen controls the formation of autoantibodies.
Abstract
The disease mechanisms of complex inflammatory disorders are difficult to define because of extensive interactions between genetic and environmental factors. Coeliac disease is a typical complex inflammatory disorder, but this disease is unusual in that crucial genetic and environmental factors have been identified. This knowledge has allowed functional studies of the predisposing HLA molecules, the identification of antigenic epitopes and detailed studies of disease-relevant T cells in coeliac disease. This dissection of the pathogenic mechanisms of coeliac disease has uncovered principles that are relevant to other chronic inflammatory diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fasano, A. & Catassi, C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology 120, 636–651 (2001).
Corrao, G. et al. Mortality in patients with coeliac disease and their relatives: a cohort study. Lancet 358, 356–361 (2001).
Mäki, M. in Coeliac Disease (ed. Howdle, P. D.) 231–249 (Baillière Tindall, London, 1995).
Dieterich, W. et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nature Med. 3, 797–801 (1997).This paper identifies tissue transglutaminase (TG2) as the autoantigen that is recognized by coeliac-disease-specific anti-endomysial antibodies.
Sulkanen, S. et al. Tissue transglutaminase autoantibody enzyme-linked immunosorbent assay in detecting celiac disease. Gastroenterology 115, 1322–1328 (1998).
Risch, N. Assessing the role of HLA-linked and unlinked determinants of disease. Am. J. Hum. Genet. 40, 1–14 (1987).
Petronzelli, F. et al. Genetic contribution of the HLA region to the familial clustering of coeliac disease. Ann. Hum. Genet. 61, 307–317 (1997).
Bevan, S. et al. Contribution of the MHC region to the familial risk of coeliac disease. J. Med. Genet. 36, 687–690 (1999).
Greco, L. et al. The first large population-based twin study of coeliac disease. Gut 50, 624–628 (2002).
Keuning, J. J., Pena, A. S., van Leeuwen, A., van Hooff, J. P. & van Rood, J. J. HLA-DW3 associated with coeliac disease. Lancet 1, 506–508 (1976).
Ek, J., Albrechtsen, D., Solheim, B. G. & Thorsby, E. Strong association between the HLA-Dw3-related B-cell alloantigen DRw3 and coeliac disease. Scand. J. Gastroenterol. 13, 229–233 (1978).
Mearin, M. L. et al. HLA-DR phenotypes in Spanish coeliac children: their contribution to the understanding of the genetics of the disease. Gut 24, 532–537 (1983).
Trabace, S. et al. HLA-ABC and DR antigens in celiac disease. A study in a pediatric Italian population. Vox Sang. 46, 102–106 (1984).
Tosi, R. et al. Evidence that celiac disease is primarily associated with a DC locus allelic specificity. Clin. Immunol. Immunopathol. 28, 395–404 (1983).
Sollid, L. M. et al. Evidence for a primary association of celiac disease to a particular HLA-DQ α/β heterodimer. J. Exp. Med. 169, 345–350 (1989).This paper identifies HLA-DQ2 encoded in cis or in trans by the DQA1*05 and DQB1*02 alleles as the primary disease-susceptibility molecule in coeliac disease.
Sollid, L. M. Molecular basis of celiac disease. Annu. Rev. Immunol. 18, 53–81 (2000).
Djilali-Saiah, I. et al. CTLA-4 gene polymorphism is associated with predisposition to coeliac disease. Gut 43, 187–189 (1998).
Holopainen, P. et al. CD28/CTLA4 gene region on chromosome 2q33 confers genetic susceptibility to celiac disease. A linkage and family-based association study. Tissue Antigens 53, 470–475 (1999).
Naluai, A. T. et al. The CTLA4/CD28 gene region on chromosome 2q33 confers susceptibility to celiac disease in a way possibly distinct from that of type-1 diabetes and other chronic inflammatory disorders. Tissue Antigens 56, 350–355 (2000).
King, A. L. et al. CTLA-4/CD28 gene region is associated with genetic susceptibility to coeliac disease in UK families. J. Med. Genet. 39, 51–54 (2002).
Popat, S. et al. Analysis of the CTLA4 gene in Swedish coeliac disease patients. Scand. J. Gastroenterol. 37, 28–31 (2002).
Zhong, F. et al. An autosomal screen for genes that predispose to celiac disease in the western counties of Ireland. Nature Genet. 14, 329–333 (1996).
Greco, L. et al. Genome search in celiac disease. Am. J. Hum. Genet. 62, 669–675 (1998).The first study to provide strong evidence that there is a coeliac-disease risk factor on chromosome 5q.
Houlston, R. S. et al. Linkage analysis of candidate regions for coeliac disease genes. Hum. Mol. Genet. 6, 1335–1339 (1997).
King, A. L. et al. A genome-wide family-based linkage study of coeliac disease. Ann. Hum. Genet. 64, 479–490 (2000).
Greco, L. et al. Existence of a genetic risk factor on chromosome 5q in Italian celiac-disease families. Ann. Hum. Genet. 65, 35–41 (2001).
Holopainen, P. et al. Candidate gene regions and genetic heterogeneity in gluten sensitivity. Gut 48, 696–701 (2001).
Naluai, T. A. et al. Genome-wide linkage analysis of Scandinavian affected sib-pairs supports presence of susceptibility loci for celiac disease on chromosomes 5 and 11. Eur. J. Hum. Genet. 9, 938–944 (2001).
Liu, J. et al. Genome-wide linkage analysis of celiac disease in Finnish families. Am. J. Hum. Genet. 70, 51–59 (2002).
Rioux, J. D. et al. Genetic variation in the 5q31 cytokine gene cluster confers susceptibility to Crohn disease. Nature Genet. 29, 223–228 (2001).
Guler, M. L. et al. Tpm1, a locus controlling IL-12 responsiveness, acts by a cell-autonomous mechanism. J. Immunol. 162, 1339–1347 (1999).
Morahan, G. et al. Linkage disequilibrium of a type-1 diabetes susceptibility locus with a regulatory IL12B allele. Nature Genet. 27, 218–221 (2001).
McIntire, J. J. et al. Identification of Tapr (an airway hyperreactivity regulatory locus) and the linked Tim gene family. Nature Immunol. 2, 1109–1116 (2001).
Louka, A. S. et al. The IL12B gene does not confer susceptibility to coeliac disease. Tissue Antigens 59, 70–72 (2002).
Halstensen, T. S., Scott, H., Fausa, O. & Brandtzaeg, P. Gluten stimulation of coeliac mucosa in vitro induces activation (CD25) of lamina propria CD4+ T cells and macrophages but no crypt-cell hyperplasia. Scand. J. Immunol. 38, 581–590 (1993).
Lundin, K. E. A. et al. Gliadin-specific, HLA-DQ(α1*0501,β1*0201)-restricted T cells isolated from the small intestinal mucosa of celiac-disease patients. J. Exp. Med. 178, 187–196 (1993).This study shows that coeliac-disease patients have gluten-specific T cells in their small-intestine mucosa, and that these T cells are restricted by the disease-associated HLA-DQ2 heterodimer.
Lundin, K. E. A., Scott, H., Fausa, O., Thorsby, E. & Sollid, L. M. T cells from the small intestinal mucosa of a DR4, DQ7/DR4, DQ8 celiac-disease patient preferentially recognize gliadin when presented by DQ8. Hum. Immunol. 41, 285–291 (1994).
Johansen, B. H., Vartdal, F., Eriksen, J. A., Thorsby, E. & Sollid, L. M. Identification of a putative motif for binding of peptides to HLA-DQ2. Int. Immunol. 8, 177–182 (1996).
van de Wal, Y., Kooy, Y. M. C., Drijfhout, J. W., Amons, R. & Koning, F. Peptide-binding characteristics of the coeliac disease-associated DQ(α1*0501, β1*0201) molecule. Immunogenetics 44, 246–253 (1996).
Vartdal, F. et al. The peptide-binding motif of the disease-associated HLA-DQ(α1*0501, β1*0201) molecule. Eur. J. Immunol. 26, 2764–2772 (1996).
Godkin, A. et al. Use of eluted peptide sequence data to identify the binding characteristics of peptides to the insulin-dependent diabetes susceptibility allele HLA-DQ8 (DQ3.2). Int. Immunol. 9, 905–911 (1997).
Kwok, W. W., Domeier, M. L., Raymond, F. C., Byers, P. & Nepom, G. T. Allele-specific motifs characterize HLA-DQ interactions with a diabetes-associated peptide derived from glutamic acid decarboxylase. J. Immunol. 156, 2171–2177 (1996).
Lee, K. H., Wucherpfennig, K. W. & Wiley, D. C. Structure of a human insulin peptide–HLA-DQ8 complex and susceptibility to type 1 diabetes. Nature Immunol. 2, 501–507 (2001).
Sjöström, H. et al. Identification of a gliadin T-cell epitope in coeliac disease: general importance of gliadin deamidation for intestinal T-cell recognition. Scand. J. Immunol. 48, 111–115 (1998).The first paper to show the importance of gluten deamidation for T-cell recognition. The paper reports the first HLA-DQ2-restricted epitope of γ-gliadin.
Molberg, Ø. et al. Tissue transglutaminase selectively modifies gliadin peptides that are recognized by gut-derived T cells. Nature Med. 4, 713–717 (1998).The first demonstration that the deamidation of glutamine residues in gliadin epitopes is mediated by TG2.
Molberg, Ø. et al. T cells from celiac-disease lesions recognize gliadin epitopes deamidated in situ by endogenous tissue transglutaminase. Eur. J. Immunol. 31, 1317–1323 (2001).
van de Wal, Y. et al. Selective deamidation by tissue transglutaminase strongly enhances gliadin-specific T-cell reactivity. J. Immunol. 161, 1585–1588 (1998).
Fleckenstein, B. et al. Gliadin T-cell epitope selection by tissue transglutaminase in celiac disease: role of enzyme specificity and pH influence on the transamidation vs. deamidation reactions. J. Biol. Chem. July 1 2002 (DOI 10.1074/jbc. M204521200)This paper shows that TG2 is involved in the selection of T-cell epitopes in gliadins, characterizes the specificity of TG2 and shows that its propensity for the deamidation reaction is stronger at a slightly acidic pH.
Bruce, S. E., Bjarnason, I. & Peters, T. J. Human jejunal transglutaminase: demonstration of activity, enzyme kinetics and substrate specificity with special relation to gliadin and coeliac disease. Clin. Sci. 68, 573–579 (1985).
Evans, D. F. et al. Measurement of gastrointestinal pH profiles in normal ambulant human subjects. Gut 29, 1035–1041 (1988).
Sollid, L. M., Molberg, Ø., McAdam, S. & Lundin, K. E. A. Autoantibodies in coeliac disease: tissue transglutaminase — guilt by association? Gut 41, 851–852 (1997).
Murtaugh, M. P., Arend, W. P. & Davies, P. J. Induction of tissue transglutaminase in human peripheral-blood monocytes. J. Exp. Med. 159, 114–125 (1984).
Akimov, S. S., Krylov, D., Fleischman, L. F. & Belkin, A. M. Tissue transglutaminase is an integrin-binding adhesion coreceptor for fibronectin. J. Cell Biol. 148, 825–838 (2000).
Akimov, S. S. & Belkin, A. M. Cell-surface tissue transglutaminase is involved in adhesion and migration of monocytic cells on fibronectin. Blood 98, 1567–1576 (2001).
Le Naour, F. et al. Profiling changes in gene expression during differentiation and maturation of monocyte-derived dendritic cells using both oligonucleotide microarrays and proteomics. J. Biol. Chem. 276, 17920–17931 (2001).
Piper, J. L., Gray, G. M. & Khosla, C. High selectivity of human tissue transglutaminase for immunoactive gliadin peptides: implications for celiac sprue. Biochemistry 41, 386–393 (2002).
Nilsen, E. M. et al. Gluten-specific, HLA-DQ-restricted T cells from coeliac mucosa produce cytokines with TH1 or TH0 profile dominated by interferon-γ. Gut 37, 766–776 (1995).
Nilsen, E. M. et al. Gluten induces an intestinal cytokine response strongly dominated by interferon-γ in patients with celiac disease. Gastroenterology 115, 551–563 (1998).
Salvati, V. M. et al. Interleukin-18 and associated markers of T helper cell type 1 activity in coeliac disease. Gut 50, 186–190 (2002).
Monteleone, G. et al. Role of interferon-α in promoting T helper cell type 1 responses in the small intestine in coeliac disease. Gut 48, 425–429 (2001).
Bardella, M. T., Marino, R. & Meroni, P. L. Celiac disease during interferon treatment. Ann. Intern. Med. 131, 157–158 (1999).
Cammarota, G., Cuoco, L., Cianci, R., Pandolfi, F. & Gasbarrini, G. Onset of coeliac disease during treatment with interferon for chronic hepatitis C. Lancet 356, 1494–1495 (2000).
Monteleone, G., Pender, S. L., Wathen, N. C. & MacDonald, T. T. Interferon-α drives T-cell-mediated immunopathology in the intestine. Eur. J. Immunol. 31, 2247–2255 (2001).
Cerf-Bensussan, N., Cuénod-Jabri, B. & Guy-Grand, D. in Coeliac Disease (eds Mäki, M., Collin, P. & Visakorpi, J. K.) 291–309 (Coeliac Disease Study Group, Tampere, 1997).
Pender, S. L. et al. A major role for matrix metalloproteinases in T-cell injury in the gut. J. Immunol. 158, 1582–1590 (1997).
Deem, R. L., Shanahan, F. & Targan, S. R. Triggered human mucosal T cells release tumour necrosis factor-α and interferon-γ which kill human colonic epithelial cells. Clin. Exp. Immunol. 83, 79–84 (1991).
Maiuri, L. et al. Definition of the initial immunologic modifications upon in vitro gliadin challenge in the small intestine of celiac patients. Gastroenterology 110, 1368–1378 (1996).
van de Wal, Y. et al. Small intestinal T cells of celiac-disease patients recognize a natural pepsin fragment of gliadin. Proc. Natl Acad. Sci. USA 95, 10050–10054 (1998).This paper reports the identification of the first HLA-DQ8-restricted epitope of α-gliadin.
van de Wal, Y. et al. Glutenin is involved in the gluten-driven mucosal T-cell response. Eur. J. Immunol. 29, 3133–3139 (1999).
Arentz-Hansen, H. et al. The intestinal T-cell response to α-gliadin in adult celiac disease is focused on a single deamidated glutamine targeted by tissue transglutaminase. J. Exp. Med. 191, 603–612 (2000).This paper characterizes two immunodominant epitopes of α-gliadin that bind to DQ2 and that are recognized by mucosal T cells of almost all adult coeliac-disease patients. The epitopes overlap and deamidation of a single glutamine residue by TG2 is crucial for T-cell recognition, which indicates a role for TG2 in epitope selection.
Anderson, R. P., Degano, P., Godkin, A. J., Jewell, D. P. & Hill, A. V. In vivo antigen challenge in celiac disease identifies a single transglutaminase-modified peptide as the dominant A-gliadin T-cell epitope. Nature Med. 6, 337–342 (2000).This paper identifies a peptide containing the same two epitopes that are described in reference 70 . The T cells that recognize this peptide were found in the peripheral blood after short-term antigenic challenge.
Vader, W. et al. The gluten response in children with celiac disease is directed toward multiple gliadin and glutenin peptides. Gastroenterology 122, 1729–1737 (2002).
Arentz-Hansen, H. et al. Celiac-lesion T cells recognize epitopes that cluster in regions of gliadins rich in proline residues. Gastroenterology (in the press).
Vanhoof, G., Goossens, F., De Meester, I., Hendriks, D. & Scharpe, S. Proline motifs in peptides and their biological processing. FASEB J. 9, 736–744 (1995).
Cunningham, D. F. & O'Connor, B. Proline-specific peptidases. Biochim. Biophys. Acta 1343, 160–186 (1997).
Hausch, F., Santiago, N. A., Gray, G. M. & Khosla, C. Digestive resistance of immunodominant gliadin peptides: implications for enzyme therapy in celiac sprue. Am. J. Physiol. Gastroenterol. Liver Physiol. June 5 2002 (DOI 10.1152/ajpgi.00136.2002)
Nelson, C. A., Vidavsky, I., Viner, N. J., Gross, M. L. & Unanue, E. R. Amino-terminal trimming of peptides for presentation on major histocompatibility complex class II molecules. Proc. Natl Acad. Sci. USA 94, 628–633 (1997).
Falk, K., Rötzschke, O., Stevanovic, S., Jung, G. & Rammensee, H. G. Pool sequencing of natural HLA-DR, -DQ and -DP ligands reveals detailed peptide motifs, constraints of processing and general rules. Immunogenetics 39, 230–242 (1994).
Vader, L. W. et al. Specificity of tissue transglutaminase explains cereal toxicity in celiac disease. J. Exp. Med. 195, 643–649 (2002).This study determines the specificity of TG2 by elegant use of gliadin-peptide libraries and mass spectrometry.
Rötzschke, O., Falk, K. & Strominger, J. L. Superactivation of an immune response triggered by oligomerized T-cell epitopes. Proc. Natl Acad. Sci. USA 94, 14642–14647 (1997).
Jardetzky, T. S. et al. Crystallographic analysis of endogenous peptides associated with HLA-DR1 suggests a common, polyproline-II-like conformation for bound peptides. Proc. Natl Acad. Sci. USA 93, 734–738 (1996).
Quarsten, H., Molberg, Ø., Fugger, L., McAdam, S. N. & Sollid, L. M. HLA binding and T-cell recognition of a tissue transglutaminase-modified gliadin epitope. Eur. J. Immunol. 29, 2506–2514 (1999).
Weiner, H. L. Oral tolerance: immune mechanisms and treatment of autoimmune diseases. Immunol. Today 18, 335–343 (1997).
Brandtzaeg, P. E. Current understanding of gastrointestinal immunoregulation and its relation to food allergy. Ann. NY Acad. Sci. 964, 13–45 (2002).
Haroon, Z. A., Hettasch, J. M., Lai, T. S., Dewhirst, M. W. & Greenberg, C. S. Tissue transglutaminase is expressed, active and directly involved in rat dermal wound healing and angiogenesis. FASEB J. 13, 1787–1795 (1999).
Ikura, K., Shinagawa, R., Suto, N. & Sasaki, R. Increase caused by interleukin-6 in promoter activity of guinea-pig liver transglutaminase gene. Biosci. Biotechnol. Biochem. 58, 1540–1541 (1994).
Kuncio, G. S. et al. TNF-α modulates expression of the tissue transglutaminase gene in liver cells. Am. J. Physiol. 274, G240–G245 (1998).
Williamson, E., Westrich, G. M. & Viney, J. L. Modulating dendritic cells to optimize mucosal immunization protocols. J. Immunol. 163, 3668–3675 (1999).
Nagler-Anderson, C. Man the barrier! Strategic defences in the intestinal mucosa. Nature Rev. Immunol. 1, 59–67 (2001).
Persson, L. A., Ivarsson, A. & Hernell, O. Breast-feeding protects against celiac disease in childhood — epidemiological evidence. Adv. Exp. Med. Biol. 503, 115–123 (2002).
Doyle, H. A. & Mamula, M. J. Post-translational protein modifications in antigen recognition and autoimmunity. Trends Immunol. 22, 443–449 (2001).
Girbal-Neuhauser, E. et al. The epitopes targeted by the rheumatoid arthritis-associated antifilaggrin autoantibodies are posttranslationally generated on various sites of (pro)filaggrin by deimination of arginine residues. J. Immunol. 162, 585–594 (1999).
Schellekens, G. A., de Jong, B. A., van den Hoogen, F. H., van de Putte, L. B. & van Venrooij, W. J. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J. Clin. Invest. 101, 273–281 (1998).
Masson-Bessiere, C. et al. The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the α- and β-chains of fibrin. J. Immunol. 166, 4177–4184 (2001).
Mamula,.M. J. et al. Isoaspartyl post-translational modification triggers autoimmune responses to self-proteins. J. Biol. Chem. 274, 22321–22327 (1999).
McAdam, S. N. et al. T-cell recognition of the dominant I-Ak-restricted hen egg lysozyme epitope: critical role for asparagine deamidation. J. Exp. Med. 193, 1239–1246 (2001).
Gjertsen, H. A., Sollid, L. M., Ek, J., Thorsby, E. & Lundin, K. E. A. T cells from the peripheral blood of celiac-disease patients recognize gluten antigens when presented by HLA-DR, -DQ or -DP molecules. Scand. J. Immunol. 39, 567–574 (1994).
Aeschlimann, D. & Paulsson, M. Transglutaminases: protein cross-linking enzymes in tissues and body fluids. Thromb. Haemost. 71, 402–415 (1994).
Appel, H., Seth, N. P., Gauthier, L. & Wucherpfennig, K. W. Anergy induction by dimeric TCR ligands. J. Immunol. 166, 5279–5285 (2001).
Sette, A., Wentworth, P. & Grey, H. M. Major histocompatibility complex binding peptides: a target for therapeutic development. Curr. Opin. Biotechnol. 2, 877–881 (1991).
Folk, J. E. Mechanism and basis for specificity of transglutaminase-catalyzed ɛ-(γ-glutamyl) lysine bond formation. Adv. Enzymol. Relat. Areas Mol. Biol. 54, 1–56 (1983).
Acknowledgements
This work was supported by grants from the Research Council of Norway and the European Commission. I thank the former and present members of my laboratory and other collaborators for their contributions to the work cited. Thanks are also extended to S. McAdam, K. E. A. Lundin, Ø. Molberg and A. S. Louka for critical review of the manuscript.
Author information
Authors and Affiliations
Related links
Related links
DATABASES
Locus Link
OMIM
FURTHER INFORMATION
National Digestive Diseases Information Clearinghouse, Celiac Disease
Farrp (Food Allergy Research and Resource Program) Allergen Database
Glossary
- SIBLING RELATIVE RISK
-
The clustering of a disease in families is indicative of genetic effects. The degree of familial clustering is often expressed as the sibling relative risk (λs), which is the disease risk for a sibling of an affected individual compared with the disease risk in the general population.
- T HELPER 1/2
-
(TH1/TH2). At least two distinct subsets of activated CD4+ T cells have been described. TH1 cells produce IFN-γ, lymphotoxin and TNF, and support cell-mediated immunity. TH2 cells produce IL-4, IL-5 and IL-13, support humoral immunity and downregulate TH1 responses.
- DEAMIDATION
-
The modification of glutamine to glutamic acid, or asparagine to aspartic acid. Deamidation leads to a mass increase of 1 Da, which can be detected by mass spectrometry.
- HAPTEN
-
A molecule that can bind antibody but cannot by itself elicit an adaptive immune response. Antibodies specific for a hapten can be generated when the hapten is chemically linked to a protein carrier that is able to elicit a T-cell response.
Rights and permissions
About this article
Cite this article
Sollid, L. Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol 2, 647–655 (2002). https://doi.org/10.1038/nri885
Issue Date:
DOI: https://doi.org/10.1038/nri885
This article is cited by
-
Metabolomics and lipidomics signature in celiac disease: a narrative review
Clinical and Experimental Medicine (2024)
-
Autoimmune amelogenesis imperfecta in patients with APS-1 and coeliac disease
Nature (2023)
-
Individual variability in patterns and dynamics of fecal gluten immunogenic peptides excretion after low gluten intake
European Journal of Nutrition (2022)
-
Cutaneous and systemic anti-allergic potential of xylopic acid in rodents
Advances in Traditional Medicine (2022)
-
Distribution of celiac disease predisposing genes HLA-DQ2 and HLA-DQ8 in the native population of southern India
Indian Journal of Gastroenterology (2022)