Abstract
Stem cell therapy is a potential treatment for spinal cord injury (SCI), and a variety of different stem cell types have been evaluated in animal models and humans with SCI. No consensus exists regarding the type of stem cell, if any, that will prove to be effective therapeutically. Most data suggest that no single therapy will be sufficient to overcome all the biological complications caused by SCI. Rationales for therapeutic use of stem cells for SCI include replacement of damaged neurons and glial cells, secretion of trophic factors, regulation of gliosis and scar formation, prevention of cyst formation, and enhancement of axon elongation. Most therapeutic approaches that use stem cells involve implantation of these cells into the spinal cord. The attendant risks of stem cell therapy for SCI—including tumor formation, or abnormal circuit formation leading to dysfunction—must be weighed against the potential benefits of this approach. This Review will examine the biological effects of SCI, the opportunities for stem cell treatment, and the types of stem cells that might be used therapeutically. The limited information available on the possible benefits of stem cell therapy to humans will also be discussed.
Key Points
-
Strategies for the therapeutic use of stem cells and their derivatives in spinal cord injury (SCI) include cell replacement, trophic support and facilitation of axon regeneration
-
Stem cell transplantation, either alone or in combination with other treatments, has produced functional improvements in animal models of SCI
-
Caution must be exercised when evaluating the successes of stem cell therapy for SCI, and when developing these therapies for appropriate clinical trials
-
The existing data from clinical trials have shown some stem cell transplants to be safe, but with very limited or no therapeutic efficacy
-
Future strategies for stem cell therapies include the use of induced pluripotent stem cells, as well as the modulation of endogenous progenitor cell populations
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Tator, C. H. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol. 5, 407–413 (1995).
Ackery, A., Tator, C. & Krassioukov, A. A global perspective on spinal cord injury epidemiology. J. Neurotrauma 21, 1355–1370 (2004).
Sekhon, L. H. & Fehlings, M. G. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26 (Suppl. 24), S2–S12 (2001).
Paralysis facts & figures. Christopher & Dana Reeve Foundation Paralysis Resource Center [online], (2010).
Schwab, M. E. Repairing the injured spinal cord. Science 295, 1029–1031 (2002).
Park, E., Velumian, A. A. & Fehlings, M. G. The role of excitotoxicity in secondary mechanisms of spinal cord injury: a review with an emphasis on the implications for white matter degeneration. J. Neurotrauma 21, 754–774 (2004).
Stokes, B. T., Fox, P. & Hollinden, G. Extracellular calcium activity in the injured spinal cord. Exp. Neurol. 80, 561–572 (1983).
Balentine, J. D. Spinal cord trauma: in search of the meaning of granular axoplasm and vesicular myelin. J. Neuropathol. Exp. Neurol. 47, 77–92 (1988).
Basso, D. M., Beattie, M. S. & Bresnahan, J. C. Graded histological and locomotor outcomes after spinal cord contusion using the NYU weight-drop device versus transection. Exp. Neurol. 139, 244–256 (1996).
Kakulas, B. A. Neuropathology: the foundation for new treatments in spinal cord injury. Spinal Cord 42, 549–563 (2004).
Liu, X. Z. et al. Neuronal and glial apoptosis after traumatic spinal cord injury. J. Neurosci. 17, 5395–5406 (1997).
Crowe, M. J., Bresnahan, J. C., Shuman, S. L., Masters, J. N. & Beattie, M. S. Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat. Med. 3, 73–76 (1997).
Emery, E. et al. Apoptosis after traumatic human spinal cord injury. J. Neurosurg. 89, 911–920 (1998).
Fawcett, J. W. & Asher, R. A. The glial scar and central nervous system repair. Brain Res. Bull. 49, 377–391 (1999).
Busch, S. A. & Silver, J. The role of extracellular matrix in CNS regeneration. Curr. Opin. Neurobiol. 17, 120–127 (2007).
Zuo, J., Neubauer, D., Dyess, K., Ferguson, T. A. & Muir, D. Degradation of chondroitin sulfate proteoglycan enhances the neurite-promoting potential of spinal cord tissue. Exp. Neurol. 154, 654–662 (1998).
Moon, L. D., Asher, R. A., Rhodes, K. E. & Fawcett, J. W. Regeneration of CNS axons back to their target following treatment of adult rat brain with chondroitinase ABC. Nat. Neurosci. 4, 465–466 (2001).
Friedlander, D. R. et al. The neuronal chondroitin sulfate proteoglycan neurocan binds to the neural cell adhesion molecules Ng-CAM/L1/NILE and N-CAM, and inhibits neuronal adhesion and neurite outgrowth. J. Cell Biol. 125, 669–680 (1994).
Milev, P., Maurel, P., Haring, M., Margolis, R. K. & Margolis, R. U. TAG-1/axonin-1 is a high-affinity ligand of neurocan, phosphacan/protein-tyrosine phosphatase-ζ/β, and N-CAM. J. Biol. Chem. 271, 15716–15723 (1996).
Milev, P. et al. Interactions of the chondroitin sulfate proteoglycan phosphacan, the extracellular domain of a receptor-type protein tyrosine phosphatase, with neurons, glia, and neural cell adhesion molecules. J. Cell Biol. 127, 1703–1715 (1994).
Oohira, A., Matsui, F., Tokita, Y., Yamauchi, S. & Aono, S. Molecular interactions of neural chondroitin sulfate proteoglycans in the brain development. Arch. Biochem. Biophys. 374, 24–34 (2000).
Shen, Y. et al. PTPσ is a receptor for chondroitin sulfate proteoglycan, an inhibitor of neural regeneration. Science 326, 592–596 (2009).
Menet, V., Prieto, M., Privat, A. & Gimenez y Ribotta, M. Axonal plasticity and functional recovery after spinal cord injury in mice deficient in both glial fibrillary acidic protein and vimentin genes. Proc. Natl Acad. Sci. USA 100, 8999–9004 (2003).
Wilhelmsson, U. et al. Absence of glial fibrillary acidic protein and vimentin prevents hypertrophy of astrocytic processes and improves post-traumatic regeneration. J. Neurosci. 24, 5016–5021 (2004).
Bradbury, E. J. et al. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 416, 636–640 (2002).
Faulkner, J. R. et al. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J. Neurosci. 24, 2143–2155 (2004).
Herrmann, J. E. et al. STAT3 is a critical regulator of astrogliosis and scar formation after spinal cord injury. J. Neurosci. 28, 7231–7243 (2008).
Okada, S. et al. Conditional ablation of Stat3 or Socs3 discloses a dual role for reactive astrocytes after spinal cord injury. Nat. Med. 12, 829–834 (2006).
Sahni, V. et al. BMPR1a and BMPR1b signaling exert opposing effects on gliosis after spinal cord injury. J. Neurosci. 30, 1839–1855 (2010).
Blight, A. R. Macrophages and inflammatory damage in spinal cord injury. J. Neurotrauma 9 (Suppl. 1), S83–S91 (1992).
Popovich, P. G., Wei, P. & Stokes, B. T. Cellular inflammatory response after spinal cord injury in Sprague-Dawley and Lewis rats. J. Comp. Neurol. 377, 443–464 (1997).
Kreutzberg, G. W. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 19, 312–318 (1996).
Beattie, M. S. et al. ProNGF induces p75-mediated death of oligodendrocytes following spinal cord injury. Neuron 36, 375–386 (2002).
Filbin, M. T. Myelin-associated inhibitors of axonal regeneration in the adult mammalian CNS. Nat. Rev. Neurosci. 4, 703–713 (2003).
Rapalino, O. et al. Implantation of stimulated homologous macrophages results in partial recovery of paraplegic rats. Nat. Med. 4, 814–821 (1998).
Enzmann, G. U., Benton, R. L., Talbott, J. F., Cao, Q. & Whittemore, S. R. Functional considerations of stem cell transplantation therapy for spinal cord repair. J. Neurotrauma 23, 479–495 (2006).
Okano, H. Stem cell biology of the central nervous system. J. Neurosci. Res. 69, 698–707 (2002).
Parr, A. M., Tator, C. H. & Keating, A. Bone marrow-derived mesenchymal stromal cells for the repair of central nervous system injury. Bone Marrow Transplant. 40, 609–619 (2007).
Sharp, J. & Keirstead, H. S. Therapeutic applications of oligodendrocyte precursors derived from human embryonic stem cells. Curr. Opin. Biotechnol. 18, 434–440 (2007).
Louro, J. & Pearse, D. D. Stem and progenitor cell therapies: recent progress for spinal cord injury repair. Neurol. Res. 30, 5–16 (2008).
Nandoe Tewarie, R. S., Hurtado, A., Bartels, R. H., Grotenhuis, A. & Oudega, M. Stem cell-based therapies for spinal cord injury. J. Spinal Cord Med. 32, 105–114 (2009).
Barnabé-Heider, F. & Frisen, J. Stem cells for spinal cord repair. Cell Stem Cell 3, 16–24 (2008).
McDonald, J. W. & Belegu, V. Demyelination and remyelination after spinal cord injury. J. Neurotrauma 23, 345–359 (2006).
Reier, P. J. Cellular transplantation strategies for spinal cord injury and translational neurobiology. NeuroRx 1, 424–451 (2004).
Johansson, C. B. et al. Identification of a neural stem cell in the adult mammalian central nervous system. Cell 96, 25–34 (1999).
Meletis, K. et al. Spinal cord injury reveals multilineage differentiation of ependymal cells. PLoS Biol. 6, e182 (2008).
Friling, S. et al. Efficient production of mesencephalic dopamine neurons by Lmx1a expression in embryonic stem cells. Proc. Natl Acad. Sci. USA 106, 7613–7618 (2009).
Perrier, A. L. et al. Derivation of midbrain dopamine neurons from human embryonic stem cells. Proc. Natl Acad. Sci. USA 101, 12543–12548 (2004).
Wichterle, H., Lieberam, I., Porter, J. A. & Jessell, T. M. Directed differentiation of embryonic stem cells into motor neurons. Cell 110, 385–397 (2002).
Wada, T. et al. Highly efficient differentiation and enrichment of spinal motor neurons derived from human and monkey embryonic stem cells. PloS ONE 4, e6722 (2009).
Brüstle, O. et al. Embryonic stem cell-derived glial precursors: a source of myelinating transplants. Science 285, 754–756 (1999).
McDonald, J. W. et al. Transplanted embryonic stem cells survive, differentiate and promote recovery in injured rat spinal cord. Nat. Med. 5, 1410–1412 (1999).
Nistor, G. I., Totoiu, M. O., Haque, N., Carpenter, M. K. & Keirstead, H. S. Human embryonic stem cells differentiate into oligodendrocytes in high purity and myelinate after spinal cord transplantation. Glia 49, 385–396 (2005).
Keirstead, H. S. et al. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants remyelinate and restore locomotion after spinal cord injury. J. Neurosci. 25, 4694–4705 (2005).
Sharp, J., Frame, J., Siegenthaler, M., Nistor, G. & Keirstead, H. S. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants improve recovery after cervical spinal cord injury. Stem Cells 28, 152–163 (2010).
Hofstetter, C. P. et al. Allodynia limits the usefulness of intraspinal neural stem cell grafts; directed differentiation improves outcome. Nat. Neurosci. 8, 346–353 (2005).
Karimi-Abdolrezaee, S., Eftekharpour, E., Wang, J., Morshead, C. M. & Fehlings, M. G. Delayed transplantation of adult neural precursor cells promotes remyelination and functional neurological recovery after spinal cord injury. J. Neurosci. 26, 3377–3389 (2006).
Ogawa, Y. et al. Transplantation of in vitro-expanded fetal neural progenitor cells results in neurogenesis and functional recovery after spinal cord contusion injury in adult rats. J. Neurosci. Res. 69, 925–933 (2002).
Pfeifer, K. et al. Autologous adult rodent neural progenitor cell transplantation represents a feasible strategy to promote structural repair in the chronically injured spinal cord. Regen. Med. 1, 255–266 (2006).
Han, S. S., Kang, D. Y., Mujtaba, T., Rao, M. S. & Fischer, I. Grafted lineage-restricted precursors differentiate exclusively into neurons in the adult spinal cord. Exp. Neurol. 177, 360–375 (2002).
Lepore, A. C. & Fischer, I. Lineage-restricted neural precursors survive, migrate, and differentiate following transplantation into the injured adult spinal cord. Exp. Neurol. 194, 230–242 (2005).
Anderson, D. K., Howland, D. R. & Reier, P. J. Fetal neural grafts and repair of the injured spinal cord. Brain Pathol. 5, 451–457 (1995).
Reier, P. J., Stokes, B. T., Thompson, F. J. & Anderson, D. K. Fetal cell grafts into resection and contusion/compression injuries of the rat and cat spinal cord. Exp. Neurol. 115, 177–188 (1992).
Kerr, D. A. et al. Human embryonic germ cell derivatives facilitate motor recovery of rats with diffuse motor neuron injury. J. Neurosci. 23, 5131–5140 (2003).
Harper, J. M. et al. Axonal growth of embryonic stem cell-derived motoneurons in vitro and in motoneuron-injured adult rats. Proc. Natl Acad. Sci. USA 101, 7123–7128 (2004).
Bonner, J. F., Blesch, A., Neuhuber, B. & Fischer, I. Promoting directional axon growth from neural progenitors grafted into the injured spinal cord. J. Neurosci. Res. 88, 1182–1192 (2010).
Cao, Q. et al. Functional recovery in traumatic spinal cord injury after transplantation of multineurotrophin-expressing glial-restricted precursor cells. J. Neurosci. 25, 6947–6957 (2005).
Davies, J. E. et al. Transplanted astrocytes derived from BMP- or CNTF-treated glial-restricted precursors have opposite effects on recovery and allodynia after spinal cord injury. J. Biol. 7, 24 (2008).
Syková, E. et al. Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant. 15, 675–687 (2006).
Kopen, G. C., Prockop, D. J. & Phinney, D. G. Marrow stromal cells migrate throughout forebrain and cerebellum, and they differentiate into astrocytes after injection into neonatal mouse brains. Proc. Natl Acad. Sci. USA 96, 10711–10716 (1999).
Eglitis, M. A. & Mezey, E. Hematopoietic cells differentiate into both microglia and macroglia in the brains of adult mice. Proc. Natl Acad. Sci. USA 94, 4080–4085 (1997).
Liu, Y. & Rao, M. S. Transdifferentiation—fact or artifact. J. Cell Biochem. 88, 29–40 (2003).
Mori, F., Himes, B. T., Kowada, M., Murray, M. & Tessler, A. Fetal spinal cord transplants rescue some axotomized rubrospinal neurons from retrograde cell death in adult rats. Exp. Neurol. 143, 45–60 (1997).
Tang, B. L. & Low, C. B. Genetic manipulation of neural stem cells for transplantation into the injured spinal cord. Cell. Mol. Neurobiol. 27, 75–85 (2007).
Tobias, C. A. et al. Delayed grafting of BDNF and NT-3 producing fibroblasts into the injured spinal cord stimulates sprouting, partially rescues axotomized red nucleus neurons from loss and atrophy, and provides limited regeneration. Exp. Neurol. 184, 97–113 (2003).
Schwab, M. E. & Bartholdi, D. Degeneration and regeneration of axons in the lesioned spinal cord. Physiol. Rev. 76, 319–370 (1996).
Richardson, P. M., McGuinness, U. M. & Aguayo, A. J. Axons from CNS neurons regenerate into PNS grafts. Nature 284, 264–265 (1980).
Houle, J. D. Demonstration of the potential for chronically injured neurons to regenerate axons into intraspinal peripheral nerve grafts. Exp. Neurol. 113, 1–9 (1991).
Levi, A. D. et al. Peripheral nerve grafts promoting central nervous system regeneration after spinal cord injury in the primate. J. Neurosurgery 96, 197–205 (2002).
Silver, J. & Miller, J. H. Regeneration beyond the glial scar. Nat. Rev. Neurosci. 5, 146–156 (2004).
Chen, A., Xu, X. M., Kleitman, N. & Bunge, M. B. Methylprednisolone administration improves axonal regeneration into Schwann cell grafts in transected adult rat thoracic spinal cord. Exp. Neurol. 138, 261–276 (1996).
Paino, C. L. & Bunge, M. B. Induction of axon growth into Schwann cell implants grafted into lesioned adult rat spinal cord. Exp. Neurol. 114, 254–257 (1991).
Ramón-Cueto, A., Plant, G. W., Avila, J. & Bunge, M. B. Long-distance axonal regeneration in the transected adult rat spinal cord is promoted by olfactory ensheathing glia transplants. J. Neurosci. 18, 3803–3815 (1998).
Féron, F. et al. Autologous olfactory ensheathing cell transplantation in human spinal cord injury. Brain 128, 2951–2960 (2005).
Saberi, H. et al. Treatment of chronic thoracic spinal cord injury patients with autologous Schwann cell transplantation: an interim report on safety considerations and possible outcomes. Neurosci. Lett. 443, 46–50 (2008).
Hofstetter, C. P. et al. Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc. Natl Acad. Sci. USA 99, 2199–2204 (2002).
Gu, W. et al. Transplantation of bone marrow mesenchymal stem cells reduces lesion volume and induces axonal regrowth of injured spinal cord. Neuropathology doi:10.1111/j.1440-1789.2009.01063.x.
Jin, Y., Fischer, I., Tessler, A. & Houle, J. D. Transplants of fibroblasts genetically modified to express BDNF promote axonal regeneration from supraspinal neurons following chronic spinal cord injury. Exp. Neurol. 177, 265–275 (2002).
Liu, Y. et al. Transplants of fibroblasts genetically modified to express BDNF promote regeneration of adult rat rubrospinal axons and recovery of forelimb function. J. Neurosci. 19, 4370–4387 (1999).
Taylor, L., Jones, L., Tuszynski, M. H. & Blesch, A. Neurotrophin-3 gradients established by lentiviral gene delivery promote short-distance axonal bridging beyond cellular grafts in the injured spinal cord. J. Neurosci. 26, 9713–9721 (2006).
Lu, P., Yang, H., Jones, L. L., Filbin, M. T. & Tuszynski, M. H. Combinatorial therapy with neurotrophins and cAMP promotes axonal regeneration beyond sites of spinal cord injury. J. Neurosci. 24, 6402–6409 (2004).
Bregman, B. S. et al. Transplants and neurotrophic factors increase regeneration and recovery of function after spinal cord injury. Prog. Brain Res. 137, 257–273 (2002).
Kadoya, K. et al. Combined intrinsic and extrinsic neuronal mechanisms facilitate bridging axonal regeneration one year after spinal cord injury. Neuron 64, 165–172 (2009).
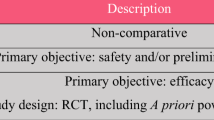
Tator, C. H. Review of treatment trials in human spinal cord injury: issues, difficulties, and recommendations. Neurosurgery 59, 957–982 (2006).
Steeves, J. D. et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 45, 206–221 (2007).
Fawcett, J. W. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 45, 190–205 (2007).
Lammertse, D. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial design. Spinal Cord 45, 232–242 (2007).
Tuszynski, M. H. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP Panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord 45, 222–231 (2007).
Magnus, T., Liu, Y., Parker, G. C. & Rao, M. S. Stem cell myths. Philos. Trans. R. Soc. Lond. B Biol. Sci. 363, 9–22 (2008).
Blight, A. et al. Position statement on the sale of unproven cellular therapies for spinal cord injury: the international campaign for cures of spinal cord injury paralysis. Spinal Cord 47, 713–714 (2009).
Hawryluk, G. W., Rowland, J., Kwon, B. K. & Fehlings, M. G. Protection and repair of the injured spinal cord: a review of completed, ongoing, and planned clinical trials for acute spinal cord injury. Neurosurg. Focus 25, E14 (2008).
Knafo, S. & Choi, D. Clinical studies in spinal cord injury: moving towards successful trials. Br. J. Neurosurg. 22, 3–12 (2008).
Geffner, L. F. et al. Administration of autologous bone marrow stem cells into spinal cord injury patients via multiple routes is safe and improves their quality of life: comprehensive case studies. Cell Transplant. 17, 1277–1293 (2008).
Pal, R. et al. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study. Cytotherapy 11, 897–911 (2009).
Yoon, S. H. et al. Complete spinal cord injury treatment using autologous bone marrow cell transplantation and bone marrow stimulation with granulocyte macrophage-colony stimulating factor: phase I/II clinical trial. Stem Cells 25, 2066–2073 (2007).
Mackay-Sim, A. et al. Autologous olfactory ensheathing cell transplantation in human paraplegia: a 3-year clinical trial. Brain 131, 2376–2386 (2008).
Lima, C. et al. Olfactory mucosal autografts and rehabilitation for chronic traumatic spinal cord injury. Neurorehabil. Neural Repair 24, 10–22 (2010).
Knoller, N. et al. Clinical experience using incubated autologous macrophages as a treatment for complete spinal cord injury: phase I study results. J. Neurosurg. Spine 3, 173–181 (2005).
Moviglia, G. A. et al. Combined protocol of cell therapy for chronic spinal cord injury. Report on the electrical and functional recovery of two patients. Cytotherapy 8, 202–209 (2006).
Lithium and blood cord cell for spinal cord injury. Chinese Spinal Cord Injury Network [online], (2007).
Spinal Cord Injury Network USA [online], (2009).
Alper, J. Geron gets green light for human trial of ES cell-derived product. Nat. Biotechnol. 27, 213–214 (2009).
Couzin, J. Biotechnology. Celebration and concern over US trial of embryonic stem cells. Science 323, 568 (2009).
Horner, P. J. et al. Proliferation and differentiation of progenitor cells throughout the intact adult rat spinal cord. J. Neurosci. 20, 2218–2228 (2000).
Horky, L. L., Galimi, F., Gage, F. H. & Horner, P. J. Fate of endogenous stem/progenitor cells following spinal cord injury. J. Comp. Neurol. 498, 525–538 (2006).
Mothe, A. J. & Tator, C. H. Proliferation, migration, and differentiation of endogenous ependymal region stem/progenitor cells following minimal spinal cord injury in the adult rat. Neuroscience 131, 177–187 (2005).
Kitada, M., Chakrabortty, S., Matsumoto, N., Taketomi, M. & Ide, C. Differentiation of choroid plexus ependymal cells into astrocytes after grafting into the pre-lesioned spinal cord in mice. Glia 36, 364–374 (2001).
Cao, Q. L., Howard, R. M., Dennison, J. B. & Whittemore, S. R. Differentiation of engrafted neuronal-restricted precursor cells is inhibited in the traumatically injured spinal cord. Exp. Neurol. 177, 349–359 (2002).
Yang, H. et al. Endogenous neurogenesis replaces oligodendrocytes and astrocytes after primate spinal cord injury. J. Neurosci. 26, 2157–2166 (2006).
Pearse, D. D. & Bunge, M. B. Designing cell- and gene-based regeneration strategies to repair the injured spinal cord. J. Neurotrauma 23, 438–452 (2006).
Ohori, Y. et al. Growth factor treatment and genetic manipulation stimulate neurogenesis and oligodendrogenesis by endogenous neural progenitors in the injured adult spinal cord. J. Neurosci. 26, 11948–11960 (2006).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872 (2007).
Nakagawa, M. et al. Generation of induced pluripotent stem cells without Myc from mouse and human fibroblasts. Nat. Biotechnol. 26, 101–106 (2008).
Yu, J. et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 318, 1917–1920 (2007).
Kim, D. et al. Generation of human induced pluripotent stem cells by direct delivery of reprogramming proteins. Cell Stem Cell 4, 472–476 (2009).
Feng, Q. et al. Hemangioblastic derivatives from human induced pluripotent stem cells exhibit limited expansion and early senescence. Stem Cells 28, 704–712 (2010).
Robbins, R. D., Prasain, N., Maier, B. F., Yoder, M. C. & Mirmira, R. G. Inducible pluripotent stem cells: not quite ready for prime time? Curr. Opin. Organ Transplant. 15, 61–67 (2009).
Bulte, J. W. In vivo MRI cell tracking: clinical studies. AJR Am. J. Roentgenol. 193, 314–325 (2009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Sahni, V., Kessler, J. Stem cell therapies for spinal cord injury. Nat Rev Neurol 6, 363–372 (2010). https://doi.org/10.1038/nrneurol.2010.73
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2010.73
This article is cited by
-
Endometrium Derived Stem Cells as Potential Candidates in Nervous System Repair
Annals of Biomedical Engineering (2022)
-
Nerve growth factor (NGF) with hypoxia response elements loaded by adeno-associated virus (AAV) combined with neural stem cells improve the spinal cord injury recovery
Cell Death Discovery (2021)
-
Adipose mesenchymal stem cell transplantation alleviates spinal cord injury-induced neuroinflammation partly by suppressing the Jagged1/Notch pathway
Stem Cell Research & Therapy (2020)
-
Tissue-type plasminogen activator-primed human iPSC-derived neural progenitor cells promote motor recovery after severe spinal cord injury
Scientific Reports (2019)
-
Is cell transplantation a reliable therapeutic strategy for spinal cord injury in clinical practice? A systematic review and meta-analysis from 22 clinical controlled trials
European Spine Journal (2019)