Abstract
Although singlet oxygen (1O2) has long been proposed as the primary reactive oxygen species in photodynamic therapy (PDT), it has only recently been possible to detect it in biological systems by its luminescence at 1270 nm. Having previously demonstrated this in vitro and in vivo, we showed that cell survival was strongly correlated to the 1O2 luminescence in cell suspensions over a wide range of treatment parameters. Here, we extend this to test the hypothesis that the photobiological response in vivo is also correlated with 1O2 generation, independent of individual treatment parameters. The normal skin of SKH1-HR hairless mice was sensitised with 20% amino-levulinic acid-induced protoporophyrin IX and exposed to 5, 11, 22 or 50 J cm−2 of pulsed 523 nm light at 50 mW cm−2, or to 50 J cm−2 at 15 or 150 mW cm−2. 1O2 luminescence was measured during treatment and the photodynamic response of the skin was scored daily for 2 weeks after treatment. As observed by other authors, a strong irradiance dependence of the PDT effect was observed. However, in all cases the responses increased with the 1O2 luminescence, independent of the irradiance, demonstrating for the first time in vivo an unequivocal mechanistic link between 1O2 generation and photobiological response.
Similar content being viewed by others
Main
Photodynamic therapy (PDT) is an emerging therapy for the treatment of solid tumours and some nonmalignant conditions (Dougherty et al, 1998; Stewart et al, 1998). The therapy involves the activation of light-sensitive drugs with a laser or other light source to generate reactive oxygen species (ROS). For most clinically used photosensitisers, the most important ROS is believed to be singlet oxygen (1O2 (1Δg)) (Weishaupt et al, 1976). The action of 1O2 results in modification or destruction of the target tissue and subsequent clinical effects (Schweitzer and Schmidt, 2003).
Since PDT involves three interdependent and dynamic treatment factors (i.e. light, photosensitiser and oxygen), complete and accurate dosimetry is a difficult problem and is the focus of ongoing research by several groups. Several techniques have been proposed (Wilson et al, 1997a), such as ‘explicit dosimetry’, in which the quantities of light, drug and oxygen are continuously monitored during treatment. Alternatively, ‘implicit dosimetry’ utilises a surrogate for biological damage, such as the photodegradation of the photosensitiser (fluorescence) during treatment to predict treatment outcome (Wilson et al, 1997a; Dysart et al, 2002). The focus of the present work is ‘direct dosimetry’, which entails direct measurement of 1O2 during treatment.
In PDT, 1O2 is generated by the following type-II pathway (Patterson et al, 1990):

where S0, S1 and T1 are the ground singlet, first excited singlet and first excited triplet states of the photosensitiser, respectively and 3O2 and 1O2 are the ground triplet and first excited singlet states of molecular oxygen, respectively. Once generated, 1O2 may undergo radiative decay at 1270 nm with a low probability. This luminescence is routinely measurable in solution (Krasnovsky, 1998), but in vitro and in vivo the lifetime of 1O2 drops dramatically, from approximately 3 μs to around 100 ns (Moan and Berg, 1991; Schweitzer and Schmidt, 2003) because of the rapid reaction of 1O2 with surrounding biomolecules. Likewise, the probability of radiative decay drops, such that measurement of this luminescence in biological media has traditionally not been feasible due to limited detector sensitivity and/or temporal response. Nevertheless, there has been significant interest in doing this, both for basic photobiological research and as a potential PDT dosimetry tool (Parker, 1987; Gorman and Rodgers, 1992).
In 2002, we showed for the first time that this is now possible using a novel near-infrared (NIR)-sensitive photomultiplier tube (PMT) (Niedre et al, 2002b). Specifically, we measured 1O2 luminescence in vitro from leukaemia cells and in vivo in normal liver and skin of Wistar rats, sensitised with aluminium tetrasulphonated phthalocyanine (AlS4Pc). Subsequently, Hirano et al (2002) also showed that this was possible in vivo in implanted murine tumours sensitised with ATX-S10 using the same PMT.
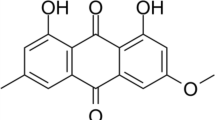
More recently, we published a set of experiments that showed that 1O2 luminescence was a useful PDT dose metric in vitro (Niedre et al, 2002a, 2003). Specifically, this demonstrated that the killing of OCI-AML5 leukaemia cells treated with aminolevulinic acid (ALA)-induced protoporphyrin IX (PpIX) PDT correlated very strongly with the 1O2 luminescence measured during treatment, regardless of initial photosensitiser concentration, irradiance or molecular oxygen concentration. These experiments differed from our initial feasibility study in that the light and photosensitiser conditions were typical of clinical PDT treatments (as opposed to being optimised for generation of 1O2) and, hence, substantial technical upgrades were required to the detection system.
Following this encouraging first step, we report here a set of experiments that extend this concept to an in vivo model, specifically the normal skin of hairless mice sensitised with ALA-PpIX. For this, we used an available green (523 nm) light source, for which the 1O2 generation and PDT effect were both confined to relatively superficial tissue. This model is based on studies conducted by Robinson et al (1998) that attempted to correlate PpIX photobleaching with the observed skin response measured daily for 2 weeks following treatment. Here, we observed (as did Robinson et al) a strong irradiance dependence of the response, despite identical ALA concentrations and total treatment fluence. We show that the 1O2 luminescence generated during treatment correlates well with the observed skin response in all cases, regardless of the treatment fluence or irradiance. To our knowledge, this is the first time that such a correlation has been demonstrated in vivo.
As will be discussed, these data support the hypothesis that 1O2 is the primary ROS involved in PDT in vivo. They are also encouraging for the development of 1O2 luminescence-based preclinical and/or clinical PDT dosimetry systems.
Materials and methods
Theory
As described in detail previously (Niedre et al, 2002b), the local 1O2 concentration as a function of time generated by a short laser pulse is given by:

where N is the number of photons per cm2 in the excitation pulse incident on the sample, σ is the photosensitiser ground state absorption cross-section (cm2), [S0] is the concentration of the photosensitiser ground state, ΦD is the quantum yield of 1O2, and τT and τD are the photosensitiser triplet-state lifetime and 1O2 lifetime, respectively.
The total number of photons emitted in the radiative decay of 1O2 at 1270 nm is given by

where τR is the radiative lifetime of 1O2 in the specific environment. Equation (C) can be integrated over time to give the total number of photons emitted after excitation by a single laser pulse as

Hence, the concentration of 1O2 generated in a sample is directly proportional to the total emitted luminescence.
We approximate integral (D) experimentally by counting the total luminescence in the interval between 2 and 90 μs following the laser pulse and subtracting background contributions. Since the laser was operating at 10 kHz, by counting in this interval the system was actively measuring 88% of the time. As in our earlier work, the contributions from the first 2 μs were rejected due to strong fluorescence contributions to the signal from the photosensitiser and some optical elements. Since the kinetics of the 1O2 luminescence were determined by Equation (B), we could expect that, despite the extremely short τD in tissue, the 1O2 full-time curve would last several τT. Our previous estimates for τT in tissue were between 25 and 30 μs (Niedre et al, 2002b), and in the present experiments were confirmed to be 30 to 40 μs (data not shown). However, even if τT was very long (e.g. due to very low pO2) the loss of counts would be small (i.e. <12%) due to the high duty cycle of the system.
Apparatus
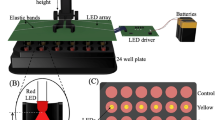
The apparatus used to measure 1O2 luminescence in vivo is shown in Figure 1. This system has been described in detail elsewhere (Niedre et al, 2003), with modifications made for the current experiments as follows: (i) The NIR PMT (R5509-14, Hamamatsu Corp., Bridgewater, NJ, USA) was mounted vertically, so that the detector and collection optics were above the animals. As before, the operating voltage of the PMT was set to −1500 V using a high voltage power supply (model SR445, Stanford Research Systems, Sunnyvale, CA, USA); (ii) a small, 4 mm × 4 mm silver-coated prism (01-PRS-411, Melles Griot Inc., Nepean, ON, Canada) was mounted directly in front of the silicon long-pass filter and used to redirect the laser beam 90° towards the skin surface. This allowed illumination of the skin while maintaining close positioning between it and the detection optics and to give a high numerical aperture for maximum light collection, and (iii) the multichannel scalar was replaced with a high-speed multiscalar module (Becker and Hickl MSA-300, Boston Electronics, Brookline, MA, USA), which allowed us to operate the laser at 10 kHz without loss of signal due to speed limitations of the electronics.
As with our earlier studies (Niedre et al, 2002a, 2003), the laser was a 523 nm diode-pumped, Q-switched frequency-doubled Nd : YLF (QG-523-500; Crystalaser Inc., Reno, NV, USA) with a pulse width of ∼10 ns. The irradiance at the skin was controlled using a set of neutral density filters (FW2AND, Thor Labs Inc., Newton, NJ, USA). As also noted in our earlier studies (Niedre et al, 2002b, 2003), there are other potential sources of luminescence in the NIR range besides 1O2 luminescence, including detector dark counts, luminescence from optical components, tissue auto-fluorescence, and photosensitiser fluorescence and phosphorescence. Spectral discrimination of the detected light was, therefore, achieved using a set of five narrow-band filters centred at 1212, 1240, 1272, 1304 and 1332 nm (OD3 blocking, 20 nm FWHM; Omega Optical, Brattleboro, VT, USA) mounted on a motorised filter wheel in front of the detector. For simplicity, these will be referred to as the 1210, 1240, 1270, 1300 and 1330 nm filters. The system was automated with a personal computer so that the filter sequence could be customised between experiments.
The mice were placed on a translatable X–Y–Z platform and the skin was kept flat with small clamping arms during treatment. A pair of small 1 mW, 635 nm lasers (CPS180; Thor Labs) was aligned so as to intersect at the focal point of the collection optics. This ensured that the treated spots were positioned so that the illumination/collection geometry was consistent between experiments. These lasers were shut off immediately after positioning the animal and were on for only a few seconds.
Photodynamic therapy
A total of 39 female hairless mice were used (SKH1-HR, Charles River Laboratories Inc., Wilmington, MA, USA), 7–12 weeks old. These were maintained on a low-fluorescence chow diet for at least 2 weeks prior to treatment. They were sensitised 4 h prior to irradiation with a distilled water solution of 20% ALA (Sigma Chemical Co., St Louis, MO, USA) with 2 M NaOH (Sigma) added to raise the pH to 4 and 5% carboxymethyl cellulose (Sigma) added to increase the viscosity. This solution was applied topically to two spots (each ∼2 × 2 cm2) on the dorsal skin and covered with a transparent adhesive dressing (Tegaderm 1626W, 3M Health Care, St Paul, MN, USA). Two PDT treatments were performed on each mouse in order to minimise the total number of animals used in the study. These treatments were chosen randomly from the set described below, so that the left side and right side generally received different treatments. Immediately before the application of ALA, the stratum corneum was stripped using medical tape to facilitate diffusion of the ALA into the epidermis.
Since we had not shown previously that it was possible to measure 1O2 luminescence in vivo specifically with ALA-PpIX, a pilot study was conducted on a group of nine animals. The first three were sensitised with ALA-PpIX as above, and irradiated with 50 mW cm−2 treatment light, a second set of three were unsensitised controls and the final three were sensitised with ALA-PpIX and euthanised by intracardiac injection of T-61 (Houchst Roussel Vet, Whitby, SK, Canada) 5 min prior to irradiation. The last set allowed us to check the effect of hypoxia on the 1O2 signal.
After this initial investigation, full treatments were performed to investigate the relationship between 1O2 luminescence and PDT treatment response. The treatments were repeated six times in all cases and, as summarised in Table 1, were as follows: (i) a irradiance of either 15, 50 or 150 mW cm−2 was delivered to a constant total fluence of 50 J cm−2; (ii) a total fluence of either 5.5, 11, or 22 J cm−2 was delivered at a constant irradiance of 50 mW cm−2; (iii) unsensitised control animals were irradiated with 50 J cm−2 at either 15, 50 or 150 mW cm−2 and; (iv) control animals were sensitised but not irradiated. In cases (i–iii) the irradiated spot was 7 × 7 mm2. Since the experiments were performed over a period of several months, the order in which they were performed was randomised in order to minimise any bias, for example in the system sensitivity. For practical reasons, these were not exactly the same treatments performed by Robinson et al (1998), but are all in the same range of light and drug parameters used.
Skin scoring
Following treatment, the irradiated spot was marked and the animals were housed in darkness for 24 h and then observed daily for 2 weeks. On each day, an observer, blinded to the PDT treatment, assigned a numbered skin response score for each treated spot in the range 0–6, as summarised in Table 2. Photographs of the treated spots were taken with a calibrated colour card each day to document the response. All experiments were performed in compliance with the guidelines of the Ontario Cancer Institute Animal Care Committee.
Singlet oxygen measurement and data analysis
The detection wavelength was selected by positioning the appropriate band-pass filter in front of the PMT. In these experiments, the system was set up to acquire for 345 000 laser pulses per filter. This took 37 s, including filter wheel motion and data processing.
Near-infrared luminescence measurements were made during all of the above experiments, including unsensitised controls. All signals were corrected for minor differences in the transmission characteristics of the optics at each wavelength. For the pilot group, measurements were made at all five wavelengths, giving more spectral information. For the animals in which full treatments were given, only three wavelengths (1240, 1270 and 1300 nm) were used in order to reduce the acquisition time, which totaled 111 s.
The measured spectra in the sensitised animals were corrected for background contributions by subtracting the mean spectrum from the control animals irradiated at the same irradiance. The 1O2 luminescence signal was then calculated as the photon counts at 1270 nm minus the average of the counts at 1240 and 1300 nm (i.e. the linearly interpolated background at 1270 nm). The resulting value was then multiplied by 3, since the system acquired at each wavelength only 1/3 of the time.
Results
Figure 2 shows typical, 5-wavelength spectra measured in the pilot group, including the sensitised, unsensitised and euthanised animals (50 mW cm−2). As expected for 1O2 luminescence, a clear 1270 nm peak was observed for the live sensitised animals. As will be demonstrated below, significant variability was observed both in terms of 1O2 generation and treatment response, even between animals receiving PDT under the same conditions. For this reason, representative data from a single sensitised animal are shown, as opposed to the average of the 1O2 luminescence observed from all of the live sensitised animals. A small but still significant peak at 1270 nm was observed in the unsensitised control animals, most likely due to 1O2 generated from naturally occurring porphyrins in the skin. No peak was observed at 1270 nm in the sensitised but euthanised animals, confirming the oxygen dependence of the signal. Hence, the system was capable of measuring 1O2 luminescence in this in vivo model.
Typical NIR spectra measured from single sensitised, unsensitised and hypoxic animals. For the sensitised animal, the individual spectra were measured at different times during treatment. For the control and hypoxic animals, error bars reflect the standard deviation of four spectra acquired for the same animal.
Figure 3 shows the average, cumulative 1O2 luminescence for sensitised animals treated with 15, 50 and 150 mW cm−2 up to a total fluence of 50 J cm−2, after subtracting the mean control (unsensitised) spectra at the same irradiances. The total 1O2 luminescence decreased with increasing irradiance. This trend was statistically significant between the three groups: specifically, one-tailed Student's t-tests yielded P=0.005 comparing the 15 and 50 mW cm−2 treatments and P=0.014 between the 50 and 150 mW cm−2 treatments. Note that the error bars in Figure 3 represent the standard deviation between the six animals in each experiment. The error due to photon counting statistics was negligible compared to this systematic variability. The relevance of this observation is discussed below.
Similar curves were measured for all other treatment groups. Figure 4 summarises the mean total 1O2 luminescence observed in each group. As would be expected, the total 1O2 luminescence increased with radiant exposure (fluence) at a constant irradiance.
Figure 5 (inset) shows the skin scores for spots treated with 50 J cm−2 at varying irradiances, corresponding to the treatments in Figure 3, as well as the unsensitised controls at 50 mW cm−2. The unsensitised animals had no observable response to light alone at 15 or 150 mW cm−2 or to ALA alone (data not shown for brevity). For the sensitised animals, the skin response increased significantly with decreasing irradiance. This was statistically significant: P=0.001 between 15 and 50 mW cm−2 and P=0.003 between 50 and 150 mW cm−2. This irradiance dependence was also observed by Robinson et al (1998), and similar effects have been reported by other authors in different in vitro and in vivo models (Feins et al, 1990; Gibson et al, 1990; Foster et al, 1993; Sitnik et al, 1998), and has usually been attributed to photochemical depletion of oxygen at high irradiances. The total skin scores as a function of fluence for all treatments are summarised in Figure 5. These were defined as the sum of the 14 individual daily scores over the 2-week period in each case. Again, these are generally consistent with those obtained by Robinson et al (1998).
A striking feature in Figures 3, 4 and 5 is the relatively large variability in the measurements for nominally identical PDT treatments. As will be discussed, this variability was primarily due to animal-to-animal differences in ALA uptake and/or PpIX synthesis, local skin pO2 and relative photosensitivity of the skin, as opposed to true ‘experimental error’. The variability observed here was not atypically large, but serves to illustrate the difficulty inherent in predicting the outcome of PDT treatments based on administered light and photosensitiser dose alone.
The total skin score as a function of the total 1O2 luminescence for all treatments is shown in Figure 6. There is a strong correlation with the 1O2 luminescence, regardless of the fluence or irradiance used. Figure 7 shows the individual data points that comprise Figure 6, together with the best χ2 fit to a three-parameter sigmoidal curve (constrained to pass through the origin) of the form:

where TSS is the total skin score and L is the total 1O2 luminescence measured. The use of this functional form for the response has no a priori mechanistic basis at this time, but is a convenient way to summarise the data. This fit was performed with four outliers removed (dotted symbols in Figure 7) and this fit yielded A=71, B=1.6 and C=108 000 and a reduced χ2 of 2.0 (χ2/NDF=5.1 with all data points included).
Total skin score as a function of total 1O2 luminescence for all individual data points that comprise the figure. The curve is the fit to Equation (E) after removal of the four outliers (open points). The error bars indicate the assumed systematic uncertainty in the visual scoring, taken as ±0.5 units on each score.
Discussion
Technical issues
As with our previous work (Patterson et al, 1990; Niedre et al, 2002a, 2002b; Niedre et al, 2003), we chose to use a set of NIR band-pass filters for spectral discrimination of the detected light rather than a monochromator (Hirano et al, 2002), since it allowed for maximum optical throughput and minimised the distance between the source and detector. Furthermore, after we verified that our system was capable of measuring 1O2 luminescence in this in vivo model, we were able to use a set of only three filters, since the 1270 nm peak was unambiguous.
The addition of a small, 4 × 4 mm prism in front of the collection optics allowed close positioning of the animals while allowing irradiation of the treatment spot. Since less than 1% of the field of view of the detector was blocked by this prism, the impact on signal collection was minimal.
Accurate positioning of the skin spot during 1O2 luminescence measurements was important, since different animals were measured over an extended period of time and absolute 1O2 luminescence measurements were compared. The pair of alignment lasers ensured that the animals were positioned reproducibly with an accuracy (height) of about ±0.5 mm at the focal plane of the detection system, so that the complete system response was consistent. Furthermore, the laser irradiance, measured before each treatment was stable to ±5% RMS, while the power supply for the PMT was stable to ±1 V.
Singlet oxygen as an in vivo dose metric
The key finding in this study is that treatment response in normal mouse skin in vivo correlates strongly 1O2 luminescence measured during PDT. Furthermore, this was the case even for a range of radiant exposures and irradiances over which the response showed significant variation. In addition, as discussed earlier, significant variability was observed in both 1O2 luminescence and skin response for nominally identical treatments. The fact that the points from the individual experiments follow a single (sigmoidal) curve (Figure 7) illustrates the ability of this technique to account for variability in treatment factors such as PpIX concentration and skin pO2. Although significantly more scatter (and outlying data points) from the parent curve is evident in Figure 7 than in our analogous in vitro studies (Niedre et al, 2003), this was not unexpected, since more variability should exist in the photobiological response between individual mice than between sets of cells from clonal populations. Also, the skin scoring system used in these experiments is somewhat subjective and may have contributed to this scatter.
The fraction of 1O2 that undergoes radiative decay relative to all 1O2 generated in the treatment volume (regardless of de-excitation pathway) is given by the ratio of the 1O2 lifetime to the luminescence lifetime, that is, τD/τL (Lamola, 1971). Hence, although the probability of radiative decay is extremely low in vivo (Niedre et al, 2002b), the emitted luminescence is tightly coupled to the ‘active’, nonradiating fraction of 1O2. The fact that the 1O2 luminescence measured here correlates extremely well with the treatment response further demonstrates this relationship. In addition, the 1O2 luminescence signal was undoubtedly heterogeneous in origin in that, for example, the photosensitiser was likely concentrated in specific tissue and/or cellular compartments (e.g. mitochondrial membrane; Wilson et al, 1997b) and the oxygenation is higher in membranes than in cytosol. However, the proportion of radiative vs nonradiative 1O2 was consistent between experiments, since we used the same photosensitiser and application conditions in all cases. This might be a complicating factor if, for example, 1O2 luminescence was compared to treatment response using different photosensitisers and administration conditions. Moreover, the effect of tissue optics in these experiments was minimal, since we deliberately chose a relatively homogeneous tissue model as opposed to, for example, a murine tumour model (Robinson et al, 1998).
This work, together along with our earlier dose–response studies in cells, supports the generally-held hypothesis that 1O2 is the important cytotoxin involved in PDT. Furthermore, since the relationship between 1O2 generation and treatment response holds in vivo, this work further demonstrates the utility of using 1O2 luminescence as a PDT dosimetry tool. However, the possibility that 1O2 is only one of the ROS generated cannot be discounted, nor can the possibility that other ROS are more important for different photosensitisers.
Irradiance effects
Strong irradiance effects were observed in these experiments, both in terms of 1O2 luminescence generation and treatment response. Irradiance effects have been observed by other authors (Feins et al, 1990; Gibson et al, 1990; Foster et al, 1993; Robinson et al, 1998; Sitnik et al, 1998) and have usually been attributed to rapid photochemical depletion of molecular oxygen at higher irradiances. The 1O2 luminescence measurements here appear to be consistent with this interpretation. Specifically, Figure 8 shows the cumulative 1O2 luminescence (as in Figure 3) as a function of total treatment time. The fact that all of the curves appear to reach approximately the same terminal slope regardless of irradiance implies that 1O2 generation was not limited by the number of excitation photons in each laser pulse, but rather by the available molecular oxygen and/or photosensitiser ground state. We are currently investigating both of these possibilities in more detail.
Other observations
Robinson et al (1998) observed rapid photobleaching of the photosensitiser: for example, greater than 90% of the PpIX was bleached after 10 J cm−2 at their lowest irradiance. This appears to contradict our data, since the incremental 1O2 generation at 15 mW cm−2 appeared unaffected by the bleaching of the photosensitiser and decreased only slightly at later time points (Figure 8). A possible explanation for this is the formation of photosensitive photoproducts during PpIX irradiation (Finlay et al, 2001). These photoproducts are known to absorb at 523 nm and therefore may have acted as secondary photosensitisers, allowing sustained photodynamic generation of 1O2. Alternatively, it is possible that sufficient PpIX was always present during treatment, so that the concentration of molecular oxygen was the limiting factor in 1O2 generation even after several orders of magnitude of photosensitiser photobleaching. This further illustrates the potential value of 1O2 luminescence-based dosimetry, since complicating factors such as photobleaching, formation of photosensitive photoproducts and tissue oxygenation are all implicitly incorporated into a single measurement.
Analysis of the data of Figure 7 showed that the lowest 1O2 luminescence counts measured from any treatment that resulted in an individual skin response score of 5 or higher (i.e. scab formation/necrosis) at any day post-treatment was 61 000 photon counts. Given the system geometric collection efficiency (0.02), quantum efficiency of the detector (0.01), optical throughput of the collection optics (0.2) and the probability of radiative decay of 1O2 in tissue (=τD/τL∼100 ns/5.55 s ∼2 × 10−8) (Niedre et al, 2002b), this was equivalent to ∼7 × 1016 molecules of 1O2 in the treatment volume. Assuming a typical cell density in tissue of around 109cm−3 and, given that the effective treatment volume was approximately 0.5 cm2 with a depth of 25 μm (Robinson et al, 1998), the 1O2 necrosis threshold for this model was about 5.8 × 1010 molecules of 1O2 per cell. This is can be compared to Georgakoudi et al's (1997) estimate of ∼7 × 109 molecules of 1O2 per cell in EMT6 spheroids treated with Photofrin-PDT, and Farrel et al's (1991) estimate of ∼5 × 108 per cell in rat liver treated with Photofrin-PDT, Interestingly, it is also significantly higher than our own estimate of the 5.6 × 107 molecules 1O2 per cell to achieve 1/e cell death in OCI-AML5 cells in vitro with ALA-PpIX (Niedre et al, 2003). This apparently higher threshold for the skin response likely reflects the relative insensitivity of normal mouse epidermal cells vs leukaemia cells, and the lack of a vascular component in the treatment response to ALA-PpIX PDT vs that of Photofrin-PDT. It should also be noted that this result is sensitive to the assumed treatment depth; here, we have assumed that PpIX synthesis is confined to the epidermis as described by Kennedy and Pottier (1992) and Robinson et al (1998), but there may have been contributions from the dermis as well. This would lead to the above threshold value being overestimated.
Conclusions
In summary, this work demonstrates the potential value of 1O2 luminescence as a dose metric in vivo. Combined with our previous studies, the prospect of further extending this work towards a clinical dosimetry system is encouraging. We plan to repeat these studies next in an implanted tumour model that has an increased level of complexity due to inherent heterogeneity in optical properties, photosensitiser uptake and oxygenation. This may require further modification of the system to provide spatial information as well as single, volume-averaged 1O2 luminescence measurements. If successful, we then plan to perform a clinical demonstration of 1O2 luminescence measurements during PDT, probably initially on skin cancer patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Dougherty TJ, Gomer CJ, Henderson BW, Jori G, Kessel D, Korbelik M, Moan J, Peng Q (1998) Review: photodynamic therapy. J Natl Cancer Inst 90: 889–905
Dysart JS, Patterson MS, Farrell TJ, Singh G (2002) Relationship between mTHPC fluorescence photobleaching and cell viability during in vitro photodynamic treatment of DP16 cells. Photochem Photobiol 75: 289–295
Farrel TJ, Wilson BC, Patterson MS, Chow R (1991) The dependence of photodynamic threshold dose on treatment parameters in normal rat liver in vivo. Proc SPIE 1426: 146–155
Feins RH, Hilf R, Ross H, Gibson SL (1990) Photodynamic therapy for human malignant mesothelioma in the nude mouse. J Surg Res 49: 311–314
Finlay JC, Conover DL, Hull EL, Foster TH (2001) Porphyrin bleaching and PDT-induced spectral changes are irradiance dependent in ALA-sensitized normal rat skin in vivo. Photochem Photobiol 73: 53–63
Foster TH, Hartley DF, Nichols MG, Hilf R (1993) Fluence rate effects in photodynamic therapy of multicell tumor spheroids. Cancer Res 53: 1249–1254
Georgakoudi I, Nichols MG, Foster TH (1997) The mechanism of photofrin photobleaching and its consequences for photodynamic dosimetry. Photochem Photobiol 65: 135–144
Gibson SL, VanDerMeid KR, Murant RS, Raubertas RF, Hilf R (1990) Effects of various photoradiation regimens on the antitumor efficacy of photodynamic therapy for R3230AC mammary carcinomas. Cancer Res 50: 7236–7241
Gorman AA, Rodgers MAJ (1992) Current perspectives of singlet oxygen detection in biological environments. J Photochem Photobiol B 14: 159–176
Hirano T, Kohno E, Nishiwaki M (2002) Detection of near infrared emission from singlet oxygen in PDT with an experimental tumor bearing mouse. J Jpn Soc Laser Surg Med 22: 99–108, (in Japanese)
Kennedy JC, Pottier RH (1992) Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J Photochem Photobiol B 14: 275–292
Krasnovsky AA (1998) Singlet molecular oxygen in photobiochemical systems: IR luminescence studies. Membrane Cell Biol 12: 665–690
Lamola AA (1971) Creation and Detection of the Excited State. New York: Marcel Dekker Inc
Moan J, Berg K (1991) The photodegradation of porphyrins in cell can be used to estimate the lifetime of singlet oxygen. Photochem Photobiol 53: 549–553
Niedre MJ, Patterson MS, Boruvka N, Wilson BC (2002a) Measurement of singlet oxygen luminescence from AML5 cells sensitized with ALA-induced PpIX in suspension during photodynamic therapy and correlation with cell viability after treatment. Proc SPIE 4612: 93–101
Niedre M, Patterson MS, Wilson BC (2002b) Direct near-infrared luminescence detection of singlet oxygen generated by photodynamic therapy in cells in vitro and tissues in vivo. Photochem Photobiol 75: 382–391
Niedre MJ, Secord AJ, Patterson MS, Wilson BC (2003) In vitro tests of the validity of singlet oxygen luminescence measurements as a dose metric in photodynamic therapy. Cancer Res 63: 7986–7994
Parker JG (1987) Optical monitoring of singlet oxygen during photodynamic treatment of tumors. IEEE Circ Devices Mag 3: 10–21
Patterson MS, Madsen SJ, Wilson BC (1990) Experimental tests of singlet oxygen luminescence monitoring in vivo during photodynamic therapy. J Photochem Photobiol B 5: 69–84
Robinson DJ, de Bruijn HS, van der Veen N, Stringer MR, Brown SB, Star WM (1998) Fluorescence photobleaching of ALA-induced protoporphyrin IX during photodynamic therapy of normal hairless mouse skin: the effect of light dose and irradiance and the resulting biological effect. Photochem Photobiol 67: 140–149
Schweitzer C, Schmidt R (2003) Physical mechanisms of generation and deactivation of singlet oxygen. Chem Rev 103: 1685–1757
Sitnik TM, Hampton JA, Henderson BW (1998) Reduction of tumor oxygenation before and after photodynamic therapy in vivo: effects of fluence rate. Br J Cancer 77: 1386–1394
Stewart F, Baas P, Star W (1998) What does photodynamic therapy have to offer radiation oncologists (or their cancer patients)? Radiother Oncol 48: 233–248
Weishaupt KR, Gomer CJ, Dougherty TJ (1976) Identification of singlet oxygen as the cytotoxic agent in photo-inactivation of a murine tumor. Cancer Res 36: 2326–2392
Wilson BC, Olivo M, Singh G (1997b) Subcellular localization of Photofrin and aminolevulinic acid and photodynamic cross-resistance in vitro in radiation-induced fibrosarcoma cells sensitive or resistant to Photofrin-mediated photodynamic therapy. Photochem Photobiol 65: 166–176
Wilson BC, Patterson MS, Lilge L (1997a) Implicit and explicit dosimetry in photodynamic therapy: a new paradigm. Lasers Med Sci 12: 182–199
Acknowledgements
This work was supported by the Canadian Cancer Society under a grant from the National Cancer Institute of Canada. We also thank Hamamatsu Corp., Hamamatsu City, Japan, and in particular Dr Ken Kaufmann (Hamamatsu, Bridgewater, NJ, USA), for supporting the acquisition of the PMT system, and the Canadian Foundation for Innovation and the Princess Margaret Hospital Foundation for equipment support. The assistance of Anoja Giles, Sandra Lafranc, and Dr Kai Zhang is also gratefully acknowledged. Dr Tom Foster provided invaluable advice on the interpretation of the above results, for which we are most grateful.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Niedre, M., Yu, C., Patterson, M. et al. Singlet oxygen luminescence as an in vivo photodynamic therapy dose metric: validation in normal mouse skin with topical amino-levulinic acid. Br J Cancer 92, 298–304 (2005). https://doi.org/10.1038/sj.bjc.6602331
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602331
Keywords
This article is cited by
-
Evaluation of fractionated and repeated sonodynamic therapy by using dual frequency for murine model of breast adenocarcinoma
Journal of Therapeutic Ultrasound (2015)
-
Dynamics of photosensitized singlet oxygen generation and photophysical characteristics of chlorin e 6 in photolon ointment
Journal of Applied Spectroscopy (2011)