Abstract
Osteopontin (OPN) is a multifunctional protein, which has recently been shown to be linked to tumorigenesis, progression and metastasis in different malignancies. Since non-small-cell lung cancer (NSCLC)'s prognosis remains bad, with few predictors of outcome, the purpose of this study was to evaluate if OPN might be involved in NSCLC's biology and therefore represent a prognostic marker and a target for new therapeutic trials. Immunohistochemistry was used to detect OPN expression, evaluated as percentage of neoplastic cells with cytoplasmic immunoreactivity, in a wide cohort of patients with stage I NSCLC (136 cases). The median value of this series (20% of positive cells) was used as the cutoff value to distinguish tumours with low (<20%) from tumours with high (⩾20%) OPN expression. A statistically significant correlation between high levels of OPN and shorter overall (P=0.034) and disease-free (P=0.011) survival in our patients was shown. Our results support the hypothesis that high OPN expression is a significantly unfavourable prognostic factor for the survival of patients with stage I NSCLC. This conclusion has notable importance in terms of the biological characterization of early-stage tumours and therapeutic opportunities.
Similar content being viewed by others
Main
Non-small-cell lung cancer (NSCLC) accounts for approximately 75% of all cases of lung cancer, which is one of the most common tumours affecting humans in the world, and is the leading cause of cancer-related deaths for both men and women in the US. Among lung cancers, NSCLC is a subgroup of particular interest because of its heterogeneity in terms of both histopathological classification and clinical behaviour: in fact, up till now, the factors responsible for the different outcomes among patients with the same stage of disease are little known. Despite improvements in detection and in surgical and medical treatments during the past two decades, the clinical behaviour of NSCLC remains bad, with an unsatisfactory survival of even stage I patients, who develop local recurrences and distant metastases, or eventually die, in about 30–40% of the cases, within 5 years after complete surgical resection, which is currently the only potentially curative treatment for NSCLC. This observation underlines how important it is to identify novel pathological parameters in addition to disease stage and, most of all, new biological markers, in order to add further prognostic information, select high-risk patients for aggressive adjuvant treatments and set new anticancer therapies.
Osteopontin (OPN) is one of the factors that seems to be linked to cancer development, progression and metastasis in different malignancies. Osteopontin is a multifunctional protein, with a protein backbone of about 32.5 kDa and multiple sites (up to 28) of phosphorylation (Sorensen et al, 1995) and cleavage. Indeed, OPN takes part in a broad range of physiological events (Sodek et al, 2000), such as bone (Reinholt et al, 1990; Giachelli and Steitz, 2000) and vascular (Shijubo et al, 2000) remodelling and tissue repair, as well as in pathological processes, like cell-mediated immunity, dystrophic calcification, coronary stenosis, wound healing and cancer metastasis (Denhardt et al, 2001).
Moreover, the observation that OPN protein or gene expression levels are increased in many human tumours, including breast (Tuck et al, 1997; Tuck and Chambers, 2001), lung (Chambers et al, 1996), prostate (Thalmann et al, 1999), colon (Agrawal et al, 2002), ovarian (Kim et al, 2002) and gastric (Ue et al, 1998) cancer, confirmed the hypothesis that it plays an important role in tumorigenesis, tumour progression and metastasis (Oates et al, 1997; Furger et al, 2001). A notable consequence of the involvement of OPN in dissemination of various solid tumours is that it could be a specific target for anticancer therapy (Weber, 2001).
However, the impact of OPN on NSCLC outcome remains unclear, with discordant data in spite of the numerous studies on OPN expression conducted up till now using immunohistochemistry (IHC) and Northern blotting (Chambers et al, 1996; Shijubo et al, 1999; Zhang et al, 2001). In the present work, we decided to investigate OPN expression in a large series (136 cases) of stage I NSCLC, in order to clarify the role that OPN plays in these tumours' biology, and to define its usefulness as a prognostic marker in identifying subsets of patients with a high risk of recurrence and who would be suitable for adjuvant and new therapies.
Materials and methods
Patients and clinical data
A total of 136 patients with NSCLC, who consecutively underwent radical surgical resection at the Department of Cardio-Thoracic Surgery of the University of Pisa from December 1991 through December 1994, were prospectively studied. No detectable metastases in distal organs were present at the time of surgery. No patient had received chemotherapy or radiotherapy before surgery. The cohort of patients included 126 (92.6%) male and 10 (7.4%) female subjects, with a combined median age of 66 years (mean age 64.6 years; range, 45–80 years). Follow-up lasted through 30 June 2003, with a median follow-up period of 49 months for living patients (range, 2–137 months). Disease-free survival and overall survival rates were calculated as the period from surgery until the date of disease relapse or of death, respectively.
Specimens
Neoplastic specimens were removed from the periphery of the tumour masses, since the central region of a tumour is more often subject to regressive alterations, and were formalin-fixed and paraffin-embedded for histological and immunohistochemical analysis. The pathologic features of the samples were classified according to World Health Organization histologic criteria (World Health Organization, 1982), and tumour staging was performed according to the International Union Against Cancer (UICC) and tumour-node-metastasis (TNM) classification (Mountain, 1997).
Immunohistochemistry
Osteopontin expression was detected by IHC using an anti-OPN polyclonal antibody (R&D Systems Inc, Minneapolis, MN, USA; dilution at 1 : 40). The antibody was applied to 5 μm sections taken from the most representative formalin-fixed, paraffin-embedded tumour tissue specimen obtained from each of the 136 patients with NSCLC, using the avidin–biotin–peroxidase complex method (Vectastatin Elite ABC kit; Vector Laboratories, Inc., Burlingame, CA, USA), following the manufacturer's instructions. The immunostaining was performed manually at room temperature. The sections, mounted on glass slides, were deparaffinised through serial baths in xylene, and then rehydrated in a graded series of alcohol and water. To remove any endogenous peroxidase activity and nonspecific background staining, the sections were soaked in absolute methanol containing 0.3% hydrogen peroxide for 30 min at room temperature. After being washed with TBS (Tris-Buffer Saline) for 5 min, the slides were blocked with nonimmune rabbit serum for 30 min to inhibit nonspecific binding, followed by incubation with the anti-OPN primary antibody for 60 min at room temperature. After rinsing with TBS for 5 min, the sections were subsequently incubated with biotin-conjugated goat anti-mouse IgG antibody for 30 min. Then, after being washed again with TBS for 5 min, the slides were incubated with avidin–biotin–peroxidase complex for 30 min and washed again with TBS. Finally, the sections were incubated with 0.05% 3,3′-diaminobenzidine tetrahydrochloride (Sigma, St Louis, MO, USA) and then rinsed in distilled water. All slides were lightly counterstained with Mayer's haematoxylin for 30 s, rinsed in running water, dehydrated and mounted with Canadian balsam. No antigen retrieval was performed. A section of thyroid papillary carcinoma, classic variant, previously proven to be OPN positive by Western blot, was used as positive control.
The immunohistochemical expression of OPN was evaluated as the percentage of tumour cells with cytoplasmic immunoreactivity, counting at least 1000 cancer cells (100 cells in 10 HPF) for each section (Figure 1). The median value of this series (20% of positive cells) was used as the cutoff value to distinguish tumours with low (<20%) from tumours with high (⩾20%) OPN expression. Moreover, we analysed the staining intensity by distinguishing four categories: one negative (0), one with a weak staining (+), one with an intermediate staining (++) and one with a strong staining (+++).
Statistical analysis
Statistical analysis was carried out using R 1.8.1 (R Development Core Team, 2003). Univariate analysis was performed by modelling Kaplan–Meier survival curves. Log rank test was used to evaluate the statistical significance of differences in survival distributions. Multivariate analysis was carried out using Cox proportional hazard model. The proportional hazard assumption was tested as proposed by Grambsch and Therneau (1994). Mann–Whitney and Kruskal–Wallis tests were used to evaluate the associations between the continuous-test variable-gene expression and patients' clinicopathological parameters [Mann–Whitney test for dichotomous variables (sex; age: <66 years vs ⩾66 years; squamous-cell carcinomas vs nonsquamous-cell carcinomas; relapse vs no relapse); Kruskal–Wallis test for nondichotomous variables (T, G)]. All tests used are described in Armitage et al (2002). Results were considered statistically significant if P<0.05.
Results
Clinicopathological characteristics
The mean age of the 126 male patients and 10 female patients was 64.6 years (range, 45–80 years; median age, 66 years). The most common histologic type of tumour was squamous-cell carcinoma (61.8%; 84 cases), followed by adenocarcinoma (30%; 41 cases), large-cell anaplastic carcinoma (6%; eight cases) and bronchioloalveolar carcinoma (2.2%; three cases). According to the degree of differentiation, the primary tumours were histopathologically graded as well differentiated (G1, 28.7%), moderately differentiated (G2, 41.9%) and poorly differentiated (G3, 29.4%). With respect to tumour size, 54 (39.7%) cancers were classified as T1 and 82 (60.3%) were classified as T2. A total of 52 (38.23%) patients presented relapses during follow-up: 13 of them developed local recurrence, whereas 39 developed distant metastases. At the end of the follow-up, 48 patients (35.3%) were alive, while 88 (64.7%) had died.
Association between clinicopathological characteristics and survival
In the sample of 136 stage I patients, among the clinicopathological characteristics, only tumour grade was significantly associated with disease-free survival (P=0.0059). Indeed, none of the other parameters showed a statistically significant correlation with outcome (Table 1).
Association of OPN expression with clinicopathological characteristics and survival
Osteopontin expression was analysed as a dichotomous variable, using the median value of 20% as the cutoff point, and distinguishing two categories: one with a high OPN expression (⩾20%) and one with a low or null OPN expression (<20%). In total, 65 (47.8%) cases showed high OPN expression, whereas in 71 (52.2%) cases OPN expression was low. Regarding the staining intensity, 40 tumours showed a weak immunoreactivity, 36 an intermediate staining and 22 a strong staining (Table 1).
Osteopontin expression was significantly correlated with sex (P=0.006) and tumour grade (P=0.00004), and was also significantly correlated with relapse (P=0.02). In fact, a significantly lower OPN expression was observed in female patients (10 out of 136), in poorly differentiated (G3) tumours, and in patients who did not relapse. On the other hand, there were no significant associations of OPN expression with age (P=0.25) and histology (P=0.75) (Table 2).
Univariate analysis showed that OPN expression was significantly correlated with overall (P=0.034) and disease-free (P=0.011) survival (Table 1). In multivariate analysis, both Cox models contain only OPN expression. A high value of OPN expression is unfavourable both to survival (risk ratio 1.88 : 1) (P=0.037) (Table 3) and relapse (risk ratio 2.08 : 1) (P=0.013) (data not shown).
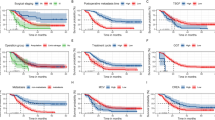
Figures 2 and 3 represent Kaplan–Meier curves for overall survival (Figure 2) and disease-free survival (Figure 3), respectively. Patients were divided according to high or low OPN expression. One can see that patients were significantly split by OPN expression regarding both overall (P=0.034) and disease-free (P=0.011) survival; in fact, stage I NSCLC patients with high OPN expression had shorter overall and disease-free survival than those with low OPN expression.
Discussion
The observation that OPN is involved in tumorigenesis, progression and metastatic dissemination of different types of human tumours, such as breast (Tuck et al, 1997; Tuck and Chambers, 2001), prostate (Thalmann et al, 1999), colon (Agrawal et al, 2002), ovarian (Kim et al, 2002), gastric (Ue et al, 1998) and lung (Chambers et al, 1996) cancer, has opened an interesting field of research, both for its possible prognostic significance in terms of disease-free and overall survival, and for its eventual role as a specific target in designing new anticancer therapies. Recently, an interesting study has shown an OPN immunostaining in many other tumours, such as pancreatic, renal, endometrial, oesophageal and head and neck carcinomas (Coppola et al, 2004).
As a consequence, in the present study, we decided to focus our interest on OPN protein expression detected by IHC in a large sample (136 cases) of NSCLCs, since these tumours still have a poor prognosis, in spite of remarkable advances in diagnosis, staging, treatment and biological characterisation. In order to establish whether OPN could be a prognostic marker for NSCLC, we analysed the correlations between OPN expression and many clinicopathological parameters, such as age and sex of patients, primary tumour size, histological type, local recurrence and, particularly, disease-free and overall survival. We decided to study in particular the subgroup of NSCLC with stage I (T1/2N0) tumours, because we think it could be very important to identify subsets of patients, who could possibly benefit from adjuvant chemoradiotherapy and, eventually, from new therapeutic trials, from among those with tumours resected in early stage.
As far as we know, our study is the largest prospective analysis of the prognostic role of OPN expression in patients with NSCLC treated with curative surgery. In our sample, OPN expression was analysed as a dichotomous variable, using the median value of 20% as the cutoff point, and distinguishing two categories: one with a high OPN expression (⩾20%) and one with a low OPN expression (<20%). In contrast to recent studies (Shijubo et al, 1999; Zhang et al, 2001; Coppola et al, 2004), we did not use a score, which combines the percentage of immunoreactive tumour cells with their staining intensity, because we considered this latter to be a highly subjective parameter (we evaluated staining intensity only as a descriptive parameter). According to the criteria we adopted, we found that 65 (47.8%) NSCLC had a high OPN expression, whereas in 71 (52.2%) cases OPN expression was low.
Osteopontin expression level was significantly correlated with overall and disease-free survival, both in univariate and in multivariate analyses; so, a high value of OPN expression is seen to be unfavourable both to survival (risk ratio 1.88 : 1) and relapse (risk ratio 2.08 : 1).
This result agreed with the conclusions of the study conducted on 82 NSCLCs by Schneider et al (2004), who showed a statistically significant association between high OPN expression and shorter survival, and with the results of one of the first works on OPN expression in 25 lung cancer patients carried out by Chambers et al (1996), who observed a higher OPN immunoreactivity in tumour specimens from patients who had died during follow-up.
As regards the association between OPN expression and clinicopathological parameters, such as age, sex, histological type, primary tumour size, histological grading, relapses during follow-up and status (alive vs dead), we observed statistically significant correlations between OPN expression and grading (P=0.00004), sex (P=0.006) and relapse (P=0.02).
The fact that patients with poorly differentiated (G3) tumours showed a significantly lower OPN expression than those with well-(G1) or moderately (G2) differentiated carcinomas could be explained by considering that in highly undifferentiated tumours the loss of cellular differentiation could be responsible for an increasing reduction of OPN protein expression.
The observation that OPN was expressed at lower levels in stage I female patients compared to male patients needs to be considered with caution, because in our study there was an imbalance in sample collection between men (126 cases) and women (10 cases); this imbalance did not depend on the way we selected our case history, because we chose to study a cohort of patients who had consecutively undergone surgical resection.
Interestingly, we did not describe significant differences between histological subgroups in terms of OPN expression (P=0.75). Our conclusion differs from those arrived at by Zhang et al (2001), who observed a preferential OPN expression in squamous-cell carcinomas (OPN immunoreactivity in 68.8% of squamous-cell carcinomas vs 20.8% of adenocarcinomas), and from those of Shijubo et al (1999), who described a significantly worse prognosis of stage I adenocarcinomas as compared to other groups, but matches that of the Schneider group's study (Schneider et al, 2004).
To sum up, in our study, a high OPN expression results as an unfavourable prognostic factor for relapse and outcome in stage I patients, and is a valid parameter by which to split this subpopulation into two groups, both for overall and for disease-free survival. This conclusion has notable importance in terms of both the biological characterisation of early-stage tumours and new therapeutic opportunities.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Agrawal D, Chen T, Irby R, Quackenbush J, Chambers AF, Szabo M, Cantor A, Coppola D, Yeatman TJ (2002) Osteopontin identified as lead marker of colon cancer progression, using pooled sample expression profiling. J Natl Cancer Inst 94: 513–521
Armitage P, Berry G, Matthews JNS (2002) Statistical Methods in Medical Research. Oxford, UK: Blackwell Publishing
Chambers AF, Wilson SM, Kerkvliet N, O'Malley FP, Harris JF, Casson AG (1996) Osteopontin expression in lung cancers. Lung Cancer 15: 311–323
Coppola D, Szabo M, Boulware D, Muraca P, Alsarra M, Chambers AF, Yeatman TJ (2004) Correlation of osteopontin protein expression and pathological stage across a wide variety of tumor histologies. Clin Cancer Res 10: 184–190
Denhardt DT, Noda M, O'Regan AW, Pavlin D, Berman JS (2001) Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodelling, and cell survival. J Clin Invest 107: 1055–1061
Furger KA, Menon RK, Tuck AB, Bramwell VH, Chambers AF (2001) The functional and clinical roles of osteopontin in cancer and metastasis. Curr Mol Med 1: 621–632
Giachelli CM, Steitz S (2000) Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol 19: 615–622
Grambsch P, Therneau T (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81: 515–526
Kim JH, Skates SJ, Uede T, Wong KK, Schorge JO, Feltmate CM, Berkowitz RS, Cramer DW, Mok SC (2002) Osteopontin as a potential diagnostic biomarker for ovarian cancer. J Am Med Assoc 287: 1671–1679
Mountain CF (1997) Revisions in the international system for staging lung cancer. Chest 111: 1710–1717
Oates AJ, Barraclough R, Rudland PS (1997) The role of osteopontin in tumorigenesis and metastasis. Invas Metast 17: 1–15
R Development Core Team (2003) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing
Reinholt FP, Hultenby K, Oldberg A, Heinegard D (1990) Osteopontin – a possible anchor of osteoclasts to bone. Proc Natl Acad Sci USA 87: 4473–4475
Schneider S, Yochim J, Brabender J, Uchida K, Danenberg KD, Metzger R, Schneider PM, Salonga D, Holscher AH, Danenberg PV (2004) Osteopontin but not osteonectin messenger RNA expression is a prognostic marker in curatively resected non-small lung cancer. Clin Cancer Res 10: 1588–1596
Shijubo N, Uede T, Kon S, Maeda K, Segawa T, Imado A, Hirasawa H, Abe S (1999) Vascular endothelial growth factor in stage I lung adenocarcinoma. Am J Resp Crit Care Med 160: 1269–1273
Shijubo N, Uede T, Kon S, Nagata M, Abe S (2000) Vascular endothelial growth factor and osteopontin in tumor biology. Crit Rev Oncol 11: 135–146
Sodek J, Ganss B, McKee MD (2000) Osteopontin. Crit Rev Oral Biol Med 11: 279–303
Sorensen ES, Hojruo P, Petersen TE (1995) Posttranslational modifications of bovine osteopontin: identification of twenty-eight phosphorylation and three O-glycosilation sites. Protein Sci 4: 2040–2049
Thalmann GN, Sikes RA, Devoll RE, Kiefer JA, Markwalder R, Klima I, Farach-Carson CM, Studer UE, Chung LW (1999) Osteopontin: possible role in prostate cancer progression. Clin Cancer Res 5: 2271–2277
Tuck AB, Chambers AF (2001) The role of osteopontin in breast cancer: clinical and experimental studies. J Mamm Gland Biol Neoplasia 6: 419–429
Tuck AB, O'Malley FP, Singhal H, Tonkin KS, Harris JF, Bautista D, Chambers AF (1997) Osteopontin and p53 expression are associated with tumor progression in a case of synchronous, bilateral, invasive mammary carcinomas. Arch Pathol Lab Med 121: 578–584
Ue T, Yokozaki H, Kitadai Y, Yamamoto S, Yasui W, Ishikawa T, Tahara E (1998) Co-expression of osteopontin and CD44v9 in gastric cancer. Int J Cancer 79: 127–132
Weber GF (2001) The metastasis gene osteopontin: a candidate target for cancer therapy. Biochem Biophys Acta 1552: 61–85
World Health Organization (1982) Histological typing of lung tumours. Am J Clin Pathol 77: 123–136
Zhang J, Takahashi K, Takahashi F, Shimizu K, Ohshita F, Kameda Y, Maeda K, Nishio K, Fukuchi Y (2001) Differential osteopontin expression in lung cancer. Cancer Lett 171: 215–222
Acknowledgements
This work was supported by grants from the Associazione Italiana per la Ricerca sul Cancro (AIRC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Boldrini, L., Donati, V., Dell'Omodarme, M. et al. Prognostic significance of osteopontin expression in early-stage non-small-cell lung cancer. Br J Cancer 93, 453–457 (2005). https://doi.org/10.1038/sj.bjc.6602715
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602715
Keywords
This article is cited by
-
Osteopontin: A Novel Therapeutic Target for Respiratory Diseases
Lung (2024)
-
Extracellular matrix profiles determine risk and prognosis of the squamous cell carcinoma subtype of non-small cell lung carcinoma
Genome Medicine (2022)
-
GOLM1 predicts poor prognosis of patients with NSCLC and is associated with the proliferation and chemo‐sensitivity of cisplatin in NSCLC cells: bioinformatics analysis and laboratory validation
Journal of Bioenergetics and Biomembranes (2021)
-
Prognostic significance of serum osteopontin levels in small cell lung cancer
BMC Pulmonary Medicine (2020)
-
Abnormally activated OPN/integrin αVβ3/FAK signalling is responsible for EGFR-TKI resistance in EGFR mutant non-small-cell lung cancer
Journal of Hematology & Oncology (2020)