Abstract
The lymphatic system is the primary pathway of metastasis for most human cancers. Recent research efforts in studying lymphangiogenesis have suggested the existence of a relationship between lymphatic vessel density and patient survival. However, current methodology of lymphangiogenesis quantification is still characterised by high intra- and interobserver variability. For the amount of lymphatic vessels in a tumour to be a clinically useful parameter, a reliable quantification technique needs to be developed. With this consensus report, we therefore would like to initiate discussion on the standardisation of the immunohistochemical method for lymphangiogenesis assessment.
Similar content being viewed by others
Main
Metastasis is the leading cause of cancer mortality. Metastatic cancer cells can escape from their site of origin and spread to distant organs through invasion of the vascular system and/or the lymphatic system. Tumour vascularisation is widely accepted as a bona fide indicator of tumour growth, metastases and patient survival. In 1996, Peter Vermeulen et al (1996) published a first international consensus on the methodology and criteria of the evaluation of angiogenesis quantification in solid tumours and 5 years later, a second consensus report, in which new concepts and mechanisms of tumour vascularisation were integrated, appeared (Vermeulen et al, 2002). Both reports were aimed at improving the standardisation of angiogenesis quantification in order to allow intratumourous microvessel density to be applied as a prognostic indicator and, moreover, as a reliable predictor of the risk of malignant transformation of premalignant lesions and of response to cancer treatment. Contrary to angiogenesis, the de novo formation of lymphatic vessels or lymphangiogenesis and its role in promoting the metastatic spread of tumour cells has only recently become a focal point of cancer research with an increasing number of studies showing a relationship between patient survival and lymphatic density in different tumour types. In order to confirm the potential prognostic value of lymphangiogenesis in patients with cancer, a quantification method that is characterised by a low intra- and interobserver variability needs to be developed. In this first consensus report, we would like to provide an overview of current concepts of the lymphatic vasculature and its regulating factors and propose guidelines for the estimation of the ongoing lymphangiogenesis in solid human tumour sections.
Structural and molecular characteristics of the lymphatic vasculature
The vascular and lymphatic systems play complementary roles in tissue perfusion and subsequent extracellular fluid reabsorption. Lymphatic vessels comprise a complex open-ended capillary network that collect lymph from various organs and tissues. Lymphatic vessels are lined by a single layer of nonfenestrated endothelium that is attenuated over most of its surface, except in the perinuclear region which bulges into the lumen (Leak, 1976). Lymphatic endothelium abut an incomplete or absent basement membrane and has overlapping junctional complexes. Lymphatics are attached to the underlying matrix through anchoring filaments (Leak and Burke, 1968), which keep the vessel patent and therefore aid lymphatic flow even in areas with elevated hydrostatic pressure and these filaments may mediate outside-in signalling from the extracellular matrix akin to integrins. The complex anchoring filaments–focal adhesions may also control the permeability of lymphatic endothelium and finely adjust lymph formation to the physiological conditions of the extracellular matrix.
There are some differences in structure in different parts of the lymphatic system. Lymphatic vessels in tissues are absorbing capillaries with walls consisting solely of endothelium that drain into collecting vessels. Collecting lymphatic vessels have a thin circumferential extracellular coat and pericytes that reduce lymphatic fluid extravasation (Pepper and Skobe, 2003b). The transition between the absorbing and collecting vessels occurs gradually and so-called precollectors have been described which drain into prenodal collecting vessels with an irregular and tortuous course. The precollectors and collecting lymphatic vessels also have valves that enable uni-directional lymph flow (Swartz and Skobe, 2001).
Vascular and lymphatic endothelial cells share many similarities (Alitalo et al, 2005). Indeed, although initially thought to be restricted to blood vascular endothelial cells (BVECs), rod-like electrondense Weibel-Palade bodies containing Factor VIII-related antigen (von Willebrand factor) have been reported in lymphatic endothelial cells (LECs) (Di Nucci et al, 1996; Marchetti, 1996; Sacchi et al, 1999). Furthermore, 98% of genes were expressed at comparable levels by BVECs and LECs in culture (Petrova et al, 2002; Podgrabinska et al, 2002; Hirakawa et al, 2003) with the differences in those genes being involved in the regulation of lymphangiogenesis and lymphatic function (Sleeman et al, 2001) (vide infra). Nevertheless, akin to vascular endothelium, comparative studies suggest that different lymphatic endothelia have different phenotypes that are likely to mediate various biological activities (Garrafa et al, 2006).
Molecular players of tumour lymphangiogenesis
Similar to angiogenesis, the growth of lymphatic vessels is regulated by a large number of growth factors (Table 1, Figure 1). Initially, members of the vascular endothelial growth factor (VEGF) family, VEGF-C and VEGF-D, were thought to be the only lymphangiogenic factors that stimulate lymphangiogenesis via activation of VEGFR-3 specifically expressed on normal LECs (Oh et al, 1997; Achen et al, 1998). The observation that a number of tumours expressing these two factors at low or undetectable levels that metastasize via the lymphatic system suggests that additional signalling systems probably exist (Cao, 2005a).
In xenographic and transgenic mouse tumour models, the overexpression of VEGF-A in tumours leads to lymphatic metastasis via intra- and peritumourous lymphatic vessels (Hirakawa et al, 2005; Bjorndahl et al, 2005b). It appears that VEGF-A indirectly induces lymphangiogenesis by recruiting VEGFR-1 expressing inflammatory cells including monocytes/macrophages and neutrophils that produce VEGF-C/-D because VEGFR-3 antagonists are able to block VEGF-A-induced lymphangiogenesis (Cursiefen et al, 2004). However, the direct effect of VEGF-A on lymphangiogenesis has also been reported since VEGFR-2 is expressed in LECs (Hong et al, 2004). Similar to VEGF-A, FGF-2 can indirectly induce lymphangiogenesis via the VEGF-C/-D/VEGFR-3 pathway by the recruitment of inflammatory cells, although a recent study also shows that FGF-2 may also directly stimulate the growth of LECs in vitro and lymphangiogenesis in vivo (Kubo et al, 2002; Chang et al, 2004; Shin et al, 2005). PDGF-BB was only recently described as a direct lymphangiogenic factor that promotes lymphatic metastasis (Cao et al, 2004). Both PDGF receptor alpha (PDGFR-a) and beta (PDGFR-b) are expressed on isolated LECs and all three prototypes of PDGFs, PDGF-AA, PDGF-BB and PDGF-CC, are able to induce lymphangiogenesis (Cao et al, 2004). Members of the angiopoietin (Ang-1 and -2), hepatocyte growth factor (HGF) and insulin-like growth factor (IGF-1 and IGF-2) family are newly reported direct lymphangiogenic factors (Gale et al, 2002; Morisada et al, 2005; Bjorndahl et al, 2005a; Cao, 2005b).
These known lymphangiogenic factors exhibit overlapping angiogenic activity on blood vessels. Thus, exposure of these growth factors to blood vessels and lymphatic vessels leads to simultaneous stimulation of angiogenesis and lymphangiogenesis (Cao, 2005b). However, under certain circumstances, both FGF-2 and VEGF-A have been reported to specifically induce only lymphangiogenesis and not angiogenesis (Chang et al, 2004; Bjorndahl et al, 2005b). The molecular mechanism underlying the differential effects of the same factor is currently unknown.
Quantification of tumour lymphangiogenesis: prognostic/predictive value in oncology
In most cancers, lymph node (LN) metastasis is an important prognostic factor. However, LN status does not allow a solid prediction of prognosis for patients presenting with small tumours without LN involvement. Other reliable markers predictive of LN metastasis might improve prognostication and might be useful for therapeutic decision-making in these early cancers. Information about lymphatic invasion and the number of lymphatic vessels has been shown promising in this regard. In breast cancer, for example, the invasion of tumour cells into lymphatic vessels was shown to be predictive of LN involvement and a prognostic factor for overall and disease-free survival (Schoppmann et al, 2004; Lee et al, 2006). Indeed, peritumourous vascular invasion, especially lymphovascular invasion (LVI), has been included as a novel adverse prognostic factor in a series of guidelines and recommendations for postoperative adjuvant systemic therapies of early breast cancer developed by an International Consensus Panel during the St Gallen Conference, 2005 (Goldhirsch et al, 2005). The presence of peritumourous vascular invasion defined an intermediate risk for patients with node-negative breast disease, but its value in patients with node-positive breast disease was considered uncertain and insufficient at that time. Another clear example is early gastric cancer, in which the incidence of LN micrometastasis has been shown to be higher in patients with, than without LVI, indicating a close link between LVI and the initial stage of LN metastasis (Arigami et al, 2005). Lymphovascular invasion was found to be an adverse prognostic indicator in several studies of gastric cancer (Hyung et al, 2002; Kooby et al, 2003; Dicken et al, 2006). Other examples are node-negative bladder carcinoma (Lotan et al, 2005) and node-negative oesophageal carcinoma (Vazquez-Sequeiros et al, 2002) in which LVI was shown to be correlated with outcome. These data suggest that LVI may provide useful information for prognosis and clinical management in those patients who present with early tumours without LN involvement.
A correlation of lymphatic vessel density (LVD) detected by immunohistochemistry with an unfavourable prognosis has been observed in breast cancer, head and neck cancer, melanoma, cervical cancer, non-small-cell lung cancer, bladder cancer, colorectal cancer and gastric cancer. However, for the amount of lymphatic vessels in a solid tumour to be a reliable marker of prognosis, the quantification technique has to be characterised by a low intra- and interobserver variability. Results obtained at different institutes should be comparable in order to allow meta-analyses. Recently, the Programme for the Assessment of Clinical Cancer Tests Strategy group and a working group of a NCI-EORTC collaboration have reported guidelines for tumour marker studies with the objectives of facilitating the evaluation of the appropriateness and quality of study design, methods, analyses, and improving the ability to compare results across studies (McShane et al, 2005). In Table 2 we listed prognostic studies showing an association of LVD with the survival of patients with cancer and indicated how well the REporting Recommendations for tumour MARKer (REMARK) were followed as a tool for the reader. This consensus report aims to lower the methodological variability of lymphangiogenesis quantification in tumour tissue sections, bearing the REMARK guidelines for prognostic studies in mind.
Lymphatic endothelial-specific antibodies for immunohistochemistry
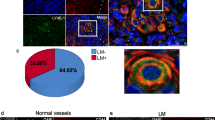
The selection of the optimal marker of the lymphatic endothelium is clearly a critical step in the assessment of LVD since false data arising from low specificity of the staining must be avoided. Major research efforts during these last years have lead to the discovery of a large spectrum of candidate lymphatic markers (Figure 2). The following paragraphs focus on markers for which antibodies are available and provide a discussion on the specificity of each marker for LECs.
VEGFR-3
The vascular endothelial growth factor receptor 3 (VEGFR-3/Flt4) is a tyrosine kinase that is predominantly expressed in LECs in adult tissues (Kaipainen et al, 1995; Kukk et al, 1996). As VEGFR-3 expression has also been found in fenestrated capillaries of several organs including the bone marrow, splenic and hepatic sinusoids, kidney glomeruli and endocrine glands (Partanen et al, 1999) and in endothelial cells of the proliferating neovasculature in breast cancer (Valtola et al, 1999), this marker is not reliable for discriminating between lymphatic and blood vascular endothelium.
Desmoplakin
The glycoprotein desmoplakin locates exclusively to the intracellular junctions between the endothelial cells of lymphatic vessels (Schmelz and Franke, 1993). Antibodies against desmoplakin have indicated specificity for lymphatic endothelium in human tongue (Ebata et al, 2001) but further studies are required to confirm the distinctive nature of desmoplakin staining in other tissue types.
β-chemokine receptor D6
By using in situ binding assays it was shown that the β-chemokine receptor D6 is expressed on LECs in the skin (Hub and Rot, 1998). Monoclonal antibodies raised against the receptor specifically stained endothelial cells that were also stained with antipodoplanin antibodies (see below) and showed no immunoreactivity with endothelial cells lining the blood vessels (Nibbs et al, 2001). D6-immunoreactive lymphatic vessels were also abundant in mucosa and submucosa of small and large intestine and appendix, but were not observed in heart, kidney, liver, skeletal muscle, brain, cerebellum, pancreas, prostate and thyroid. This demonstrates the emerging heterogeneity of lymphatic endothelium, and it may be necessary to use specific markers depending on which tissue is being investigated.
Prox-1
Another marker of the lymphatic endothelium is the homeodomain protein Prox-1, which is required for the regulation of lymphatic vascular development from pre-existing embryonic veins (Wigle and Oliver, 1999). Prox-1 expression has also been found in other cell types, including nonendothelial cells in the lens, heart, liver, pancreas and nervous system (Stacker et al, 2002). Antibodies against human Prox-1 to visualise lymphatic vessels in tumour sections have only been used in a limited number of studies (Agarwal et al, 2005; Van der Auwera et al, 2005). Although its nuclear localisation makes Prox-1 not the most ideal marker for quantifying lymphatic vessels microscopically, it could be a useful marker for double immunostaining with other markers such as podoplanin and LYVE-1.
LYVE-1
LYVE-1 is an integral membrane glycoprotein that functions as a receptor for hyaluronan (GlcNAcb1–4GlcUAb1–3)n, a ubiquitous extracellular matrix glycosaminoglycan involved in cell migration and differentiation. The expression of LYVE-1 in endothelial cells of lymphatic vessels and LN sinuses and its absence from blood vessel endothelium was first demonstrated by immunohistochemical staining with polyclonal antibodies generated against recombinant human and murine LYVE-1 Fc fusion protein which showed characteristic staining of lymphatic vascular structures in skin, intestine and secondary lymphoid tissue (Banerji et al, 1999; Prevo et al, 2001). During embryogenesis, LYVE-1 is expressed in cardinal vein endothelium, just before budding of the primordial lymph sacs (E12.5 in the mouse), almost simultaneous with the expression of the lymphogenic transcription factor Prox-1 (Wigle and Oliver, 1999); expression then persists into adulthood in most afferent vessels and lymphatic sinuses, but is absent from thoracic duct. LYVE-1 is also abundant in discontinuous endothelia including human and mouse liver sinusoids and human spleen sinusoids but is absent from the ‘normal’ haemovasculature. Extensive analyses in many different laboratories have confirmed these findings and demonstrated that LYVE-1 is a reliable marker for distinguishing lymphatic vessels from blood vessels in a range of different human cancers (e.g. head and neck squamous cell carcinoma (Beasley et al, 2002; Maula et al, 2003), cutaneous melanoma (Dadras et al, 2003; Straume et al, 2003) and carcinomas of the thyroid (Hall et al, 2003), lung (Koukourakis et al, 2005), pancreas (Von Marschall et al, 2005), breast (Williams et al, 2003; Bono et al, 2004), cervix (Van Trappen et al, 2003) and prostate (Trojan et al, 2004)), as well as normal tissues in both adult and foetus. Nevertheless, the observation that expression of LYVE-1 can be downmodulated in some tissues, for example, in response to inflammation (Johnson L and Jackson DG, unpublished), and is absent in some tumour-associated lymphatics (Rubbia-Brandt et al, 2004; Stessels et al, 2004; Van der Auwera et al, 2004) underlines the importance of utilising multiple markers (e.g. LYVE-1/podoplanin, LYVE-1/Prox-1, etc.) to characterise lymphatic vessels in comprehensive studies of lymphangiogenesis. Besides lymphatic and sinusoidal vessel endothelium, LYVE-1 is also expressed in some macrophage-like cells present in inflamed tissue and in tumour infiltrates. The special significance of these findings has been revealed in recent studies of lymphangiogenesis occurring during corneal neovascularisation (Maruyama et al, 2005) and in transplanted kidney rejection (Kerjaschki et al, 2006) where LYVE-1+/CD68+ cells were shown to be incorporated into newly dividing lymphatic vessels. These findings indicate the fascinating possibility that LYVE-1+ macrophage-like cells may represent bone marrow derived progenitors with the capacity to differentiate towards lymphatic vessel endothelium as well as regulators of VEGF-C induced lymphoproliferation (vide infra).
Podoplanin
Podoplanin is a ∼38-kd surface glycoprotein that is expressed in osteoblastic cells, lung alveolar type I cells and kidney podocytes (Wetterwald et al, 1996; Breiteneder-Geleff et al, 1997). The specificity of podoplanin expression on lymphatic but not blood vascular endothelium has been demonstrated in the skin (Breiteneder-Geleff et al, 1999). However, podoplanin appears to be only present in small lymphatic vessels and not in larger ones that have smooth-muscle cells (Stacker et al, 2002). So far, there is no evidence of podoplanin expression in BVECs (Stacker et al, 2002), suggesting that it can be considered as a reliable marker of the lymphatic endothelium. Recently, it was indicated by Schacht et al (2005) that the commercially available monoclonal D2–40 antibody specifically recognises human podoplanin. The antibody has been shown to be a highly selective marker of lymphatic endothelium in sections of both frozen and formalin-fixed paraffin-embedded normal and neoplastic tissues (Kahn et al, 2002a) and has been proven valuable in detecting lymphatic invasion in various malignant neoplasms (Kahn and Marks, 2002b). In a direct comparison of the D2–40 antibody and an antibody against podoplanin on paraffin sections of a series of head and neck squamous cell carcinomas, both antibodies were shown to have extremely high specificity (99.7 and 98.8% for podoplanin and D2–40) and sensitivity (92.6 and 97.3% for podoplanin and D2–40) for lymphatic endothelium (Evangelou et al, 2005).
A comparative study of antibodies directed at LYVE-1, podoplanin, Prox-1 and the D2–40 antibody on serial sections of breast carcinomas indicated that significantly more intratumourous lymphatic vessels stained with D2–40 (Van der Auwera et al, 2005), thus demonstrating that this marker is highly sensitive for lymphatic endothelium. Besides being reactive with lymphatic vessels, D2–40-staining has also been observed in basal epithelial cell layers of the epidermis (Niakosari et al, 2005) and of human breast and prostate gland (Agarwal et al, 2005; Zeng et al, 2005).
Just as tumour vasculature has a markedly different phenotype from normal vessels, so it is highly likely that tumour lymphatic vessels will differ from normal and gene array studies on lymphatic endothelium isolated from tumours will be of major interest to help develop new markers relevant to tumour therapy and outcome. Fiedler et al (2006) very recently reported that the CD34 protein, a recognised vascular endothelial marker, is selectively expressed in tumour-associated LECs and not in resting organ LECs. The expression of CD34 by tumour-associated LECs was identified in colon cancer, breast cancer, lung cancer and melanoma. These findings underline the importance of CD34 as an activation antigen of human LECs and as a potential diagnostic and prognostic tumour marker.
Methodology of lymphangiogenesis quantification in solid tumours by histomorphometry
Lymphatic vessel density
By analogy with angiogenesis, tumour-associated LVD is most frequently assessed by counting the number of immunostained vessels in tumour sections, as defined by Weidner et al (1991) in 1991. Microvessel density (MVD) is determined in vascular ‘hot spots’ or areas giving the impression at low magnification of containing numerous microvessels. Vascular ‘hot spots’ are thought to represent localised areas of biological importance since they originate from tumour cell clones with the highest angiogenic potential which will predominantly enter the circulation and give rise to vascularised metastases. Localised changes in oxygen tension are indeed a strong angiogenic drive. The reproducibility of the assignment of these ‘hot spots’ is a critical variable in the analysis of MVD and the success of finding the relevant ‘hot spot’ depends on the training and experience of the investigator (Vermeulen et al, 2002). The methodology of counting the number of microvessel entities in regions with an elevated vascular density has been adapted for the assessment of LVD, although this is based on the assumption that a functional increase in lymphatic vessels occurs in ‘hot spots’. Since data on the association of lymphangiogenesis with hypoxia are still contradictory, the relevance of counting lymphatic vessels in ‘hot spots’, as opposed to an overall lymphatic vessel count, has been questioned (Shields et al, 2004).
The number of lymphatic vessels in a microscopic field is the net result of previous phases of tumour lymphangiogenesis and of lymphatic vessel remodelling or regression, which implicates that the measurement of LVD is not necessarily a reflection of the ongoing tumour lymphangiogenesis. Nevertheless, several studies in different cancer types have found a correlation of LVD with lymphangiogenic factor expression, and with the occurrence of lymphatic metastases and survival, suggesting that LVD contains important information on the degree of tumour lymphatic vasculature.
There is still a considerable debate about the role of intratumourous vs peritumourous lymphatic vessels in the pathology of primary human tumours. Several studies have shown that the density of lymphatic vessels located immediately adjacent to the tumour is associated with the presence of LN metastases (Dadras et al, 2003; Bono et al, 2004; Franchi et al, 2004; Gombos et al, 2005; Hachisuka et al, 2005; Kyzas et al, 2005; Mou et al, 2005; Renyi-Vamos et al, 2005; Zeng et al, 2005; Massi et al, 2006; Roma et al, 2006). Moreover, in a retrospective prognostic study, Dadras et al (2003) found that the size of peritumourous lymphatic vessels was the most significant independent factor that correlates with LN metastasis in human malignant melanomas. However, other studies show that intratumourous and not peritumourous lymphatic vessels are vital for lymphatic metastasis (Beasley et al, 2002; Hall et al, 2003; Maula et al, 2003; Audet et al, 2005; Kuroyama et al, 2005; Kyzas et al, 2005; Massi et al, 2006).
The infiltration of lymphatic vessels into the tumour may have a passive role in cancer metastasis by creating an increased opportunity for metastatic tumour cells to leave the primary tumour site but might also establish a paracrine signalling pathway for tumour cell growth and invasion through the release of specific growth factors or chemokines (Cassella and Skobe, 2002). Michaela Skobe et al have shown that lymphatic capillaries activated by factors produced by tumours, such as VEGF-C, promote tumour cell invasion by increasing tumour cell transendothelial migration through the expression of the CC-type chemokine ligand 1 on LECs and its receptor CC-type chemokine receptor 8 on tumour cells (Alitalo et al, 2004). Moreover, secondary lymphoid chemokine is constitutively produced by LECs in the skin (Saeki et al, 1999) and other organs (Gunn et al, 1998) and was found to attract dendritic cells to the lymphatic vessels by interaction with its primary receptor CCR7. This chemokine receptor is highly expressed in human breast cancer cells, malignant breast tumours and metastases, triggering actin polymerisation, pseudopodia formation, and the directional migration and invasion of these cells (Muller et al, 2001).
Chalkley counting
Although tumour-associated lymphangiogenesis has mainly been assessed by counting the number of immunostained lymphatic vessels, other techniques, such as Chalkley point overlap morphometry, are available. This method involves the use of an eyepiece graticule containing 25 randomly positioned dots, which is rotated so that the maximum number of points is on or within the vessels of the vascular ‘hot spot’. Thus, instead of counting the individual microvessel, the overlaying dots are counted. Hall et al (2003) investigated the relationship between LVD, determined by Chalkley counting, and clinical and pathological variables in patients with well-differentiated papillary thyroid carcinoma. In a multivariate analysis, the Chalkley score was found to be significantly associated with the presence of nodal metastases at presentation. A similar association has also been shown in head and neck cancer (Audet et al, 2005).
The Chalkley count is a reflection of the relative area taken by the lymphatic vasculature and offers a suitable alternative for LVD assessment according to Weidner's guidelines. As no decisions have to be made on whether adjacent stained structures are separate microvessel or not, Chalkley point counting should be a more objective approach. The most observer-dependent step though still remains, that is, the selection of the vascular ‘hot spot’.
Lymphatic endothelial cell proliferation (LECP)
LECP is measured by a double immunostaining of tumour sections with antibodies directed at a LEC marker (antipodoplanin or anti-LYVE-1) and a marker of proliferating cells (anti-Ki67 or anti-PCNA). Lymphatic vessels containing proliferating nuclei have been observed in breast cancer (Van der Auwera et al, 2005), endometrial cancer (Koukourakis et al, 2005), head and neck cancer (Beasley et al, 2002) and melanoma (Dadras et al, 2003; Straume et al, 2003). This suggests the presence of active intratumourous lymphangiogenesis, at least in some tumour types. In addition to the sprouting of lymphatic vessels, the enlargement of lymphatic vessels is also accompanied by the proliferation of LECs. It has been reported that both lymphangiogenesis and lymphatic hyperplasia play a role in tumour dissemination (Skobe et al, 2001; Stacker et al, 2001; He et al, 2005). In a VEGF-C overexpressing animal model, a tumour-induced increase in the diameter of collecting lymphatic vessels was associated with an enhanced passage of clusters of tumour cells to the sentinel LNs (He et al, 2005). Increased lymphatic vessel perimeters and areas were also found to be correlated with the occurrence of lymphatic metastasis in some human tumours (Nathanson et al, 1997; Dadras et al, 2003; Franchi et al, 2004; Van der Auwera et al, 2005; Liang et al, 2006; Massi et al, 2006).
Computerised image analysis systems
The major drawbacks of the visual MVD counting method are its inherent subjectivity and the difficulty of standardisation between laboratories. In contrast, image cytometry is more objective and reproducible and moreover, many image cytometry software packages allow additional information on vessel luminal area and vessel luminal perimeter. However, the widespread application of image cytometry is hampered by the need for specialised equipment to perform the analyses. Another limitation of this method is the possibility of confounding signals of nonendothelial structures in the stromal compartment. Choi et al (2005) performed a direct comparison of visual and image cytometric lymphatic vessel density counting on D2–40-immunostained sections of invasive breast carcinomas. They used an automated scanning microscope and an automated image analysis application that identified stained ring-like structures based on colour and morphometry in areas marked during direct microscopic microvessel counting. D2–40 microvessel densities determined by direct microscopy and image cytometry were significantly correlated. However, only the visual D2–40 data were associated with LN status and VEGF-family gene expression.
Surrogate markers of tumour-associated lymphangiogenesis
Histopathological markers
Fibrotic focus
Similar to angiogenesis, the fibrotic focus and the growth pattern might be considered as surrogate histopathological markers for tumour-associated lymphangiogenesis (Vermeulen et al, 2002). A fibrotic focus is defined as a fibrosclerotic scar-like area replacing necrosis in the centre of a carcinoma. The presence of a fibrotic focus in breast cancer is considered to be a surrogate marker of hypoxia-driven angiogenesis as it was shown to predict for higher MVD and for a higher fraction of proliferating endothelial cells (Jitsuiki et al, 1999; Colpaert et al, 2003a). Similarly, its presence in breast cancer is associated with a higher LECP but not with a higher LVD (Van der Auwera et al, 2005).
Tumour growth pattern
It has been previously shown that different growth patterns in primary breast cancer reflect differences in angiogenesis. In the infiltrative growth pattern, the carcinoma cells invade between pre-existing structures without a significant disturbance of the tissue architecture. Expansively growing breast tumours form a well-circumscribed nodule consisting of carcinoma cells and desmoplastic connective tissue. The endothelial cell proliferation fraction and the Chalkley count were highest in the expansive growth pattern (Colpaert et al, 2003b; Van den Eynden et al, 2005). Recently, it became clear that the growth pattern is also a histological surrogate marker of lymphangiogenesis (Van der Auwera et al, 2005). LECP, both in the tumour parenchyma and at the tumour periphery, was significantly higher in the expansive growth pattern compared with the infiltrative growth pattern. In addition, the intratumourous LVD was highest in the infiltrative growth pattern. An association between the growth pattern and the presence of lymphangiogenesis has also been observed in human non-small-cell lung cancer (Renyi-Vamos et al, 2005).
Tumour levels of lymphangiogenic growth factors
The expression, in various human cancers, of lymphangiogenic factors such as VEGF-C and VEGF-D, is closely related to tumour-induced lymphatic dilatation or lymphangiogenesis (less frequent) and thereby to LN metastasis (Pepper et al, 2003a).
In breast cancer, increased expressions of VEGF-C and VEGF-D in the tumour cells, both on the mRNA and protein level, are known to be associated with high LVD, lymphatic invasion and LN metastasis (Nakamura et al, 2003; Choi et al, 2005; Nakamura et al, 2005; Huang et al, 2006; Li et al, 2006). Straume et al (2003) have compared LVD, evaluated by counting the number of LYVE-1-positive vessels in hot spots, with the protein expression of several (lymph)angiogenic growth factors in cutaneous melanoma specimens. Among the factors tested (VEGF-A, VEGF-C, VEGFR-1, VEGFR-2, VEGFR-3, FGF-2, ephrin-A1/2, interleukin-8 and thrombospondin-1), only the expression of FGF-2 was significantly associated with increased LVD. Furthermore, evidence for the existence of an association between VEGF-C or VEGF-D expressions and the number of tumour lymphatic vessels has also been provided for colorectal cancer (Ohno et al, 2003; Jia et al, 2004; Wang et al, 2005), gastric cancer (Yonemura et al, 2001; Onogawa et al, 2005; Shida et al, 2005; Juttner et al, 2006), thyroid cancer (Yasuoka et al, 2005), early-stage squamous cell cancer of the urerine cervix (Gombos et al, 2005) and pancreatic cancer (Sipos et al, 2004). In non-small-cell lung cancer, however, the existence of an association between VEGF-C expression and LVD remains contradictory (Lu et al, 2005; Renyi-Vamos et al, 2005; Takanami, 2006).
Other markers
The main disadvantage of the histological surrogate markers of lymphangiogenesis is the inherent interobserver variability. A more objective approach is the quantification of circulating levels of lymphangiogenic growth factors, such as VEGF-C and VEGF-D, and of circulating lymphatic endothelial progenitor cells.
Circulating levels of lymphangiogenic growth factors
From a practical point of view, the detection of circulating levels of VEGF-C and VEGF-D protein/antigen in preoperative blood samples might be a useful indicator of advanced disease.
In some cancers, circulating lymphangiogenic factors are increased compared to healthy individuals or patients with benign tumours, for example, VEGF-C in lung non-small-cell carcinoma (Tamura and Ohta, 2003). However, in ovarian carcinoma, breast carcinoma, cervix adenocarcinoma and head and neck carcinoma this seems not to be the case (Table 3). Furthermore, in colorectal cancer, VEGF-C is increased in cancer patients but not VEGF-D (George et al, 2001; Duff et al, 2005). In lung non-small-cell carcinoma, cervical squamous cell carcinoma and colorectal cancer, a higher preoperative circulating VEGF-C level strongly correlated with LN metastasis and also lymphatic vessel invasion (the latter only in lung non-small-cell carcinoma). Concerning VEGF-D, plasma levels are increased in patients with angiosarcoma compared to healthy controls, and in one study on prostate carcinoma, a correlation between VEGF-D levels and LN metastasis was found (Kaushal et al, 2005).
The above results should be seen in context, since there are only a few studies on circulating VEGF-C and VEGF-D levels compared to the expression of their mRNA or protein levels in cancer.
Lymphatic endothelial progenitor cells (LEPCs)
Bone marrow-derived circulating endothelial precursor cells contribute to newly blood vessel formation both under physiological and pathological conditions. The measurement of circulating endothelial cells in peripheral blood of patients with cancer has been integrated in clinical studies exploring the efficacy of antiangiogenic therapies. Evidence for the existence of LEPCs has only recently been found. Salven et al (2003) identified a subset of CD34+ cells that coexpress the stem/precursor cell marker CD133 and VEGFR-3. These cells are functionally nonadherent endothelial precursor cells that can differentiate into mature adherent VEGFR-3+ endothelial cells in the presence of vascular growth factors. In a corneal lymphangiogenesis model of irradiated mice reconstituted with donor BM cells, both CD34+/VEGFR-2+ cells and CD34+/VEGFR-3+ cells were found to be incorporated into the newly formed lymphatic vessels (Religa et al, 2005). A second population of candidate LECPs has now been identified. A subpopulation of human circulating CD14+ monocytes was shown to also express VEGFR-3 on its surface and could be stimulated in vitro to express VEGF-C as well as the LEC marker podoplanin (Schoppmann et al, 2002; Kerjaschki et al, 2006). It was speculated that these cells participate in inflammation-associated de novo lymphangiogenesis in nephrectomy specimens of rejected kidney transplants (Kerjaschki et al, 2006). Maruyama et al (2005) have provided direct evidence of the incorporation of transdifferentiated monocytes-macrophages into growing lymphatic vessels. In a mouse corneal transplantation model, macrophages could transdifferentiate into LECs by forming cell aggregates and vesicles that integrate into an existing lymphatic vessel. Moreover, in vitro experiments demonstrated that CD11b+ macrophages were capable of forming tube-like structures that expressed markers of lymphatic endothelium such as LYVE-1 and podoplanin. These data indicate a novel role for macrophages in lymphangiogenesis. Gene expression profiling studies are necessary for characterisation of LECPs in peripheral blood and will improve our understanding of lymphatic endothelial function in cancer.
Recommended methodology
So far, studies on the importance of lymphangiogenesis for tumour growth have yielded inconsistent conclusions and this is mostly due to differences in the applied methodology and the lack of standardisation. In Table 4, a proposition for the standardisation of the immunohistochemical method for lymphangiogenesis assessment is given.
Methods of lymphangiogenesis quantification in solid tumours rely upon the use of markers that allow an accurate discrimination between lymphatic vessels and blood vessels in histological tissue sections. At present the most reliable marker is likely to be podoplanin, which is recognised by the monoclonal D2–40 antibody with a high specificity and sensitivity. Although LYVE-1 has been proven valuable for distinguishing between lymphatic vessels and blood vessels in histological tissue sections, it has been reported that LYVE-1 expression in tumour lymphatic vessels can be downmodulated, for example, in breast cancer (Stessels et al, 2004; Van der Auwera et al, 2004). None of the proposed markers fulfils the criteria of an ideal lymphatic vessel marker, which should be exclusively found on all types of LECs in all pathological conditions. Therefore, the use of multiple immunohistochemical stains on serial sections of random subgroups of cases is recommended to confirm the actual staining of lymphatic vessels. The best combination of markers of the lymphatic endothelium could vary on the tissue type. As more insights on the molecular pathways of lymphatic differentiation emerge, novel potential markers of the lymphatic endothelium might be identified.
The quantification of LVD has been proven valuable for the risk assessment of regional LN involvement in patients with cancer. By using the Chalkley point overlap morphometric technique the observer-dependent step of measuring LVD can be abolished since the Chalkley count is a relative area estimate rather than a true vessel count. However, the method that most likely reflects the ongoing tumour lymphangiogenesis would be the analysis of proliferating LECs, which can be assessed by a double immunostain with podoplanin to stain lymphatic vessels, together with Ki-67 to stain proliferating cells.
As it seems that the patterns of lymphangiogenesis vary among malignancies lymphangiogenesis should be evaluated both intratumourous and at the tumour periphery.
Summary and future directions
For every major type of cancer LN involvement is strongly associated with poor survival and usually is one of the major factors associated with poor prognosis. Whether this is the mechanism for poor prognosis or a marker for aggressive underlying molecular pathway is difficult to determine clinically. The pathway of metastasis via lymphatic vessels, regional LNs and then into the systemic circulation is an accepted pathway of metastasis, although in recent years the emphasis has switched to the importance of angiogenesis and direct systemic spread. Nevertheless, it is not possible to quantify the relative contribution to spread currently between these different routes and the very strong association of LN involvement with outcome is a key factor in the staging of all cancers. Understanding such an important prognostic factor, the mechanisms regulating it and how it might be related to prognosis are important issues regardless of any possible therapeutic approach.
Understanding the mechanisms by which lymphangiogenesis occurs or tumour cells migrate to lymphatic vessels, or indeed understanding how new lymphatic vessels are generated from other cell types such as macrophages or circulating progenitor cells is all highly relevant to potential mechanisms of growth of metastases. VEGF-A-overexpressing primary tumours have been shown to induce sentinel LN lymphangiogenesis before metastasising (Hirakawa et al, 2005) and also in human cancer lymphangiogenesis appears to occur in secondary sites, for example, in LN metastases of breast cancer (Van den Eynden et al, 2006). This might suggest that primary tumours begin preparing their future metastatic site by inducing the growth of new lymphatic vessels.
Lymphangiogenesis is a complex process that is regulated by multiple factors that are produced by various cell types. Some of the originally angiogenic signalling molecules, such as VEGF-A and FGF-2, have been implicated in the control of lymphatic vessel growth as well, indicating a close link between angiogenesis and lymphangiogenesis. Novel insights into the interrelationship between both processes will lead to a better understanding of the mechanisms of growth of metastases and will have important implications for cancer therapy. Many potent antiangiogenic compounds that can be used in anticancer therapy have been identified and are currently being investigated in clinical trials. It is not clear whether these antiangiogenic agents also affect lymphangiogenesis and hence, biopsy studies should also stain for effects on lymphatic vessels to dissect their possible role in response to therapy.
The search for specific lymphangiogenesis inhibitors has led to the identification of a number of potential antilymphangiogenic compounds that have been shown to suppress metastasis of tumours to regional LNs in experimental animal models. These include antibodies that either block the activity of the ligands VEGF-C and VEGF-D directly by binding to the ligand or by preventing the interaction with VEGFR-3 and soluble dimeric fusion proteins containing the extracellular ligand binding site of VEGFR-3 (Banerji et al, 1999; Thiele and Sleeman, 2006). However, many questions concerning their potential therapeutic role in the management of human cancer are raised. Although the point could be made that when patients first present they already have lymphatic metastasis or not, and these will be treated surgically or with other means, it would be highly desirable to prevent metastasis in patients who are at increased risk of second primaries. A clear example is breast cancer with second cancers either in the treated breast or the opposite breast and reducing the incidence of new primaries, but also reducing the instance of secondary deposits from the new primaries is a key therapeutic aim.
Understanding the mechanisms of lymphangiogenesis could be helpful in the adjuvant situation of managing common cancers with treatment aimed at both stopping proliferation and recurrence of primary tumours and their regional metastases.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Achen MG, Jeltsch M, Kukk E, Makinen T, Vitali A, Wilks AF, Alitalo K, Stacker SA (1998) Vascular endothelial growth factor D (VEGF-D) is a ligand for the tyrosine kinases VEGF receptor 2á(Flk1) and VEGF receptorá3á(Flt4). PNAS 95: 548–553
Agarwal B, Saxena R, Morimiya A, Mehrotra S, Badve S (2005) Lymphangiogenesis does not occur in breast cancer. Am J Surg Pathol 29: 1449–1455
Alitalo K, Mohla S, Ruoslahti E (2004) Lymphangiogenesis and cancer: meeting report. Cancer Res 64: 9225–9229
Alitalo K, Tammela T, Petrova TV (2005) Lymphangiogenesis in development and human disease. Nature 438: 946–953
Amo Y, Masuzawa M, Hamada Y, Katsuoka K (2004) Serum concentrations of vascular endothelial growth factor-D in angiosarcoma patients. Br J Dermatol 150: 160–161
Arigami T, Natsugoe S, Uenosono Y, Arima H, Mataki Y, Ehi K, Yanagida S, Ishigami S, Hokita S, Aikou T (2005) Lymphatic invasion using D2–40 monoclonal antibody and its relationship to lymph node micrometastasis in pN0 gastric cancer. Br J Cancer 93: 688–693
Audet N, Beasley NJ, MacMillan C, Jackson DG, Gullane PJ, Kamel-Reid S (2005) Lymphatic vessel density, nodal metastases, and prognosis in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 131: 1065–1070
Banerji S, Ni J, Wang SX, Clasper S, Su J, Tammi R, Jones M, Jackson DG (1999) LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J Cell Biol 144: 789–801
Beasley NJP, Prevo R, Banerji S, Leek RD, Moore J, van Trappen P, Cox G, Harris AL, Jackson DG (2002) Intratumoral lymphangiogenesis and lymph node metastasis in head and neck cancer. Cancer Res 62: 1315–1320
Birner P, Schindl M, Obermair A, Breitenecker G, Kowalski H, Oberhuber G (2001) Lymphatic microvessel density as a novel prognostic factor in early-stage invasive cervical cancer. Int J Cancer 95: 29–33
Bjorndahl M, Cao R, Nissen LJ, Clasper S, Johnson LA, Xue Y, Zhou Z, Jackson D, Jon Hansen A, Cao Y (2005a) Insulin-like growth factors 1 and 2 induce lymphangiogenesis in vivo. PNAS 102: 15593–15598
Bjorndahl MA, Cao R, Burton JB, Brakenhielm E, Religa P, Galter D, Wu L, Cao Y (2005b) Vascular endothelial growth factor-A promotes peritumoral lymphangiogenesis and lymphatic metastasis. Cancer Res 65: 9261–9268
Bono P, Wasenius VM, Heikkila P, Lundin J, Jackson DG, Joensuu H (2004) High LYVE-1-positive lymphatic vessel numbers are associated with poor outcome in breast cancer. Clin Cancer Res 10: 7144–7149
Breiteneder-Geleff S, Matsui K, Soleiman A, Meraner P, Poczewski H, Kalt R, Schaffner G, Kerjaschki D (1997) Podoplanin, novel 43-kd membrane protein of glomerular epithelial cells, is down-regulated in puromycin nephrosis. Am J Pathol 151: 1141–1152
Breiteneder-Geleff S, Soleiman A, Kowalski H, Horvat R, Amann G, Kriehuber E, Diem K, Weninger W, Tschachler E, Alitalo K, Kerjaschki D (1999) Angiosarcomas express mixed endothelial phenotypes of blood and lymphatic capillaries: podoplanin as a specific marker for lymphatic endothelium. Am J Pathol 154: 385–394
Cao R, Bjorndahl MA, Gallego MI, Chen S, Religa P, Hansen AJ, Cao Y (2006) Hepatocyte growth factor is a novel lymphangiogenic factor with an indirect mechanism of action. Blood 107: 3531–3536
Cao R, Bjorndahl MA, Religa P, Clasper S, Garvin S, Galter D, Meister B, Ikomi F, Tritsaris K, Dissing S, Ohhashi T, Jackson DG, Cao Y (2004) PDGF-BB induces intratumoral lymphangiogenesis and promotes lymphatic metastasis. Cancer Cell 6: 333–345
Cao Y (2005a) Direct role of PDGF-BB in lymphangiogenesis and lymphatic metastasis. Cell Cycle 4: 228–230
Cao Y (2005b) Opinion: emerging mechanisms of tumour lymphangiogenesis and lymphatic metastasis. Nat Rev Cancer 5: 735–743
Cassella M, Skobe M (2002) Lymphatic vessel activation in cancer. Ann NY Acad Sci 979: 120–130
Chang LK, Garcia-Cardena G, Farnebo F, Fannon M, Chen EJ, Butterfield C, Moses MA, Mulligan RC, Folkman J, Kaipainen A (2004) Dose-dependent response of FGF-2 for lymphangiogenesis. Proc Natl Acad Sci U S A 101: 11658–11663
Chen F, Takenaka K, Ogawa E, Yanagihara K, Otake Y, Wada H, Tanaka F (2004) Flt-4-positive endothelial cell density and its clinical significance in non-small cell lung cancer. Clin Cancer Res 10: 8548–8553
Choi WW, Lewis MM, Lawson D, Yin-Goen Q, Birdsong GG, Cotsonis GA, Cohen C, Young AN (2005) Angiogenic and lymphangiogenic microvessel density in breast carcinoma: correlation with clinicopathologic parameters and VEGF-family gene expression. Mod Pathol 18: 143–152
Colpaert CG, Vermeulen PB, Fox SB, Harris AL, Dirix LY, van Marck EA (2003a) The presence of a fibrotic focus in invasive breast carcinoma correlates with the expression of carbonic anhydrase IX and is a marker of hypoxia and poor prognosis. Breast Cancer Res Treat 81: 137–147
Colpaert CG, Vermeulen PB, Van Beest P, Soubry A, Goovaerts G, Dirix LY, Harris AL, van Marck EA (2003b) Cutaneous breast cancer deposits show distinct growth patterns with different degrees of angiogenesis, hypoxia and fibrin deposition. Histopathology 42: 530–540
Cursiefen C, Chen L, Borges LP, Jackson D, Cao J, Radziejewski C, D’Amore PA, Dana MR, Wiegand SJ, Streilein JW (2004) VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest 113: 1040–1050
Dadras SS, Paul T, Bertoncini J, Brown LF, Muzikansky A, Jackson DG, Ellwanger U, Garbe C, Mihm MC, Detmar M (2003) Tumor lymphangiogenesis: a novel prognostic indicator for cutaneous melanoma metastasis and survival. Am J Pathol 162: 1951–1960
Di Nucci A, Marchetti C, Serafini S, Piovella F (1996) P-selectin and von Willebrand factor in bovine mesenteric lymphatics: an immunofluorescent study. Lymphology 29: 25–28
Dicken BJ, Graham K, Hamilton SM, Andrews S, Lai R, Listgarten J, Jhangri GS, Saunders LD, Damaraju S, Cass C (2006) Lymphovascular invasion is associated with poor survival in gastric cancer: an application of gene-expression and tissue array techniques. Ann Surg 243: 64–73
Duff SE, Li C, Renehan A, O’Dwyer ST, Kumar S (2003) Immunodetection and molecular forms of plasma vascular endothelial growth factor-C. Int J Oncol 22: 339–343
Duff SE, Saunders M, McCredie V, Kumar S, O’Dwyer ST, Jayson GC (2005) Pre-operative plasma levels of vascular endothelial growth factor A, C and D in patients with colorectal cancer. Clin Oncol (R Coll Radiol) 17: 367–371
Ebata N, Nodasaka Y, Sawa Y, Yamaoka Y, Makino S, Totsuka Y, Yoshida S (2001) Desmoplakin as a specific marker of lymphatic vessels. Microvasc Res 61: 40–48
Evangelou E, Kyzas PA, Trikalinos TA (2005) Comparison of the diagnostic accuracy of lymphatic endothelium markers: Bayesian approach. Mod Pathol 18: 1490–1497
Fiedler U, Christian S, Koidl S, Kerjaschki D, Emmett MS, Bates DO, Christofori G, Augustin HG (2006) The Sialomucin CD34 is a marker of lymphatic endothelial cells in human tumors. Am J Pathol 168: 1045–1053
Franchi A, Gallo O, Massi D, Baroni G, Santucci M (2004) Tumor lymphangiogenesis in head and neck squamous cell carcinoma: a morphometric study with clinical correlations. Cancer 101: 973–978
Gale NW, Thurston G, Hackett SF, Renard R, Wang Q, McClain J, Martin C, Witte C, Witte MH, Jackson D, Suri C, Campochiaro PA, Wiegand SJ, Yancopoulos GD (2002) Angiopoietin-2 is required for postnatal angiogenesis and lymphatic patterning, and only the latter role is rescued by Angiopoietin-1. Dev Cell 3: 411–423
Garrafa E, Alessandri G, Benetti A, Turetta D, Corradi A, Cantoni AM, Cervi E, Bonardelli S, Parati E, Giulini SM, Ensoli B, Caruso A (2006) Isolation and characterization of lymphatic microvascular endothelial cells from human tonsils. J Cell Physiol 207: 107–113
George ML, Tutton MG, Janssen F, Arnaout A, Abulafi AM, Eccles SA, Swift RI (2001) VEGF-A, VEGF-C, and VEGF-D in colorectal cancer progression. Neoplasia 3: 420–427
Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thurlimann B, Senn HJ, Panel members (2005) Meeting Highlights: INTERNATIONAL Expert Consensus on the Primary Therapy of Early Breast Cancer 2005. Ann Oncol 16: 1569–1583
Gombos Z, Xu X, Chu CS, Zhang PJ, Acs G (2005) Peritumoral lymphatic vessel density and vascular endothelial growth factor C expression in early-stage squamous cell carcinoma of the uterine cervix. Clin Cancer Res 11: 8364–8371
Gunn MD, Tangemann K, Tam C, Cyster JG, Rosen SD, Williams LT (1998) A chemokine expressed in lymphoid high endothelial venules promotes the adhesion and chemotaxis of naive Tálymphocytes. PNAS 95: 258–263
Hachisuka T, Narikiyo M, Yamada Y, Ishikawa H, Ueno M, Uchida H, Yoriki R, Ohigashi Y, Miki K, Tamaki H, Mizuno T, Nakajima Y (2005) High lymphatic vessel density correlates with overexpression of VEGF-C in gastric cancer. Oncol Rep 13: 733–737
Hall FT, Freeman JL, Asa SL, Jackson DG, Beasley NJ (2003) Intratumoral lymphatics and lymph node metastases in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129: 716–719
He Y, Rajantie I, Pajusola K, Jeltsch M, Holopainen T, Yla-Herttuala S, Harding T, Jooss K, Takahashi T, Alitalo K (2005) Vascular endothelial cell growth factor receptor 3-mediated activation of lymphatic endothelium is crucial for tumor cell entry and spread via lymphatic vessels. Cancer Res 65: 4739–4746
Hirakawa S, Hong YK, Harvey N, Schacht V, Matsuda K, Libermann T, Detmar M (2003) Identification of vascular lineage-specific genes by transcriptional profiling of isolated blood vascular and lymphatic endothelial cells. Am J Pathol 162: 575–586
Hirakawa S, Kodama S, Kunstfeld R, Kajiya K, Brown LF, Detmar M (2005) VEGF-A induces tumor and sentinel lymph node lymphangiogenesis and promotes lymphatic metastasis. J Exp Med 201: 1089–1099
Hoar FJ, Lip GY, Belgore F, Stonelake PS (2004) Circulating levels of VEGF-A, VEGF-D and soluble VEGF-A receptor (sFIt-1) in human breast cancer. Int J Biol Markers 19: 229–235
Hong YK, Lange-Asschenfeldt B, Velasco P, Hirakawa S, Kunstfeld R, Brown LF, Bohlen P, Senger DR, Detmar M (2004) VEGF-A promotes tissue repair-associated lymphatic vessel formation via VEGFR-2 and the alpha1beta1 and alpha2beta1 integrins. FASEB J 18: 1111–1113
Huang JH, Li Y, Liu L, Yang HC, Hai J, Tang LL, Hu TH (2006) Lymphangiogenes and location of tumor lymphatic vessels induced by VEGF-C in primary breast cancer. Zhong Nan Da Xue Xue Bao Yi Xue Ban 31: 36–39, 51
Hub E, Rot A (1998) Binding of RANTES, MCP-1, MCP-3, and MIP-1alpha to cells in human skin. Am J Pathol 152: 749–757
Hyung WJ, Lee JH, Choi SH, Min JS, Noh SH (2002) Prognostic impact of lymphatic and/or blood vessel invasion in patients with node-negative advanced gastric cancer. Ann Surg Oncol 9: 562–567
Jia YT, Li ZX, He YT, Liang W, Yang HC, Ma HJ (2004) Expression of vascular endothelial growth factor-C and the relationship between lymphangiogenesis and lymphatic metastasis in colorectal cancer. World J Gastroenterol 10: 3261–3263
Jiang WG, Davies G, Martin TA, Parr C, Watkins G, Mansel RE, Mason MD (2005) The potential lymphangiogenic effects of hepatocyte growth factor/scatter factor in vitro and in vivo. Int J Mol Med 16: 723–728
Jitsuiki Y, Hasebe T, Tsuda H, Imoto S, Tsubono Y, Sasaki S, Mukai K (1999) Optimizing microvessel counts according to tumor zone in invasive ductal carcinoma of the breast. Mod Pathol 12: 492–498
Juttner S, Wissmann C, Jons T, Vieth M, Hertel J, Gretschel S, Schlag PM, Kemmner W, Hocker M (2006) Vascular endothelial growth factor-D and its receptor VEGFR-3: two novel independent prognostic markers in gastric adenocarcinoma. J Clin Oncol 24: 228–240
Kahn HJ, Bailey D, Marks A (2002a) Monoclonal antibody D2–40, a new marker of lymphatic endothelium, reacts with Kaposi's sarcoma and a subset of angiosarcomas. Mod Pathol 15: 434–440
Kahn HJ, Marks A (2002b) A new monoclonal antibody, D2–40, for detection of lymphatic invasion in primary tumors. Lab Invest 82: 1255–1257
Kaipainen A, Korhonen J, Mustonen T, van Hinsbergh VWM, Fang G, Dumont D, Breitman M, Alitalo K (1995) Expression of the Fms-like tyrosine kinase 4 gene becomes restricted to lymphatic endothelium during development. PNAS 92: 3566–3570
Kajiya K, Hirakawa S, Ma B, Drinnenberg I, Detmar M (2005) Hepatocyte growth factor promotes lymphatic vessel formation and function. EMBO J 24: 2885–2895
Karkkainen MJ, Ferrell RE, Lawrence EC, Kimak MA, Levinson KL, McTigue MA, Alitalo K, Finegold DN (2000) Missense mutations interfere with VEGFR-3 signalling in primary lymphoedema. Nat Genet 25: 153–159
Karkkainen MJ, Haiko P, Sainio K, Partanen J, Taipale J, Petrova TV, Jeltsch M, Jackson DG, Talikka M, Rauvala H, Betsholtz C, Alitalo K (2004) Vascular endothelial growth factor C is required for sprouting of the first lymphatic vessels from embryonic veins. Nat Immunol 5: 74–80
Karpanen T, Egeblad M, Karkkainen MJ, Kubo H, Yla-Herttuala S, Jaattela M, Alitalo K (2001) Vascular endothelial growth factor C promotes tumor lymphangiogenesis and intralymphatic tumor growth. Cancer Res 61: 1786–1790
Kato T, Prevo R, Steers G, Roberts H, Leek RD, Kimura T, Kameoka S, Nishikawa T, Kobayashi M, Jackson DG, Harris AL, Gatter KC, Pezzella F (2005) A quantitative analysis of lymphatic vessels in human breast cancer, based on LYVE-1 immunoreactivity. Br J Cancer 93: 1168–1174
Kaushal V, Mukunyadzi P, Dennis RA, Siegel ER, Johnson DE, Kohli M (2005) Stage-specific characterization of the vascular endothelial growth factor axis in prostate cancer: expression of lymphangiogenic markers is associated with advanced-stage disease. Clin Cancer Res 11: 584–593
Kerjaschki D, Huttary N, Raab I, Regele H, Bojarski-Nagy K, Bartel G, Krober SM, Greinix H, Rosenmaier A, Karlhofer F, Wick N, Mazal PR (2006) Lymphatic endothelial progenitor cells contribute to de novo lymphangiogenesis in human renal transplants. Nat Med 12: 230–234
Kooby DA, Suriawinata A, Klimstra DS, Brennan MF, Karpeh MS (2003) Biologic predictors of survival in node-negative gastric cancer. Ann Surg 237: 828–835
Koukourakis MI, Giatromanolaki A, Sivridis E, Simopoulos C, Gatter KC, Harris AL, Jackson DG (2005) LYVE-1 immunohistochemical assessment of lymphangiogenesis in endometrial and lung cancer. J Clin Pathol 58: 202–206
Kubo H, Cao R, Brakenhielm E, Makinen T, Cao Y, Alitalo K (2002) Blockade of vascular endothelial growth factor receptor-3 signaling inhibits fibroblast growth factor-2-induced lymphangiogenesis in mouse cornea. PNAS 99: 8868–8873
Kukk E, Lymboussaki A, Taira S, Kaipainen A, Jeltsch M, Joukov V, Alitalo K (1996) VEGF-C receptor binding and pattern of expression with VEGFR-3 suggests a role in lymphatic vascular development. Development 122: 3829–3837
Kuroyama S, Kobayashi N, Ohbu M, Ohtani Y, Okayasu I, Kakita A (2005) Enzyme histochemical analysis of lymphatic vessels in colon carcinoma: occurrence of lymphangiogenesis within the tumor. Hepatogastroenterology 52: 1057–1061
Kyzas PA, Geleff S, Batistatou A, Agnantis NJ, Stefanou D (2005) Evidence for lymphangiogenesis and its prognostic implications in head and neck squamous cell carcinoma. J Pathol 206: 170–177
Leak LV (1976) The structure of lymphatic capillaries in lymph formation. Fed Proc 35: 1863–1871
Leak LV, Burke JF (1968) Ultrastructural studies on the lymphatic anchoring filaments. J Cell Biol 36: 129–149
Lee AH, Pinder SE, Macmillan RD, Mitchell M, Ellis IO, Elston CW, Blamey RW (2006) Prognostic value of lymphovascular invasion in women with lymph node negative invasive breast carcinoma. Eur J Cancer 42: 357–362
Li YS, Kaneko M, Amatya VJ, Takeshima Y, Arihiro K, Inai K (2006) Expression of vascular endothelial growth factor-C and its receptor in invasive micropapillary carcinoma of the breast. Pathol Int 56: 256–261
Liang P, Hong JW, Ubukata H, Liu HR, Watanabe Y, Katano M, Motohashi G, Kasuga T, Nakada I, Tabuchi T (2006) Increased density and diameter of lymphatic microvessels correlate with lymph node metastasis in early stage invasive colorectal carcinoma. Virchows Arch 448 (5): 570–575
Lotan Y, Gupta A, Shariat SF, Palapattu GS, Vazina A, Karakiewicz PI, Bastian PJ, Rogers CG, Amiel G, Perotte P, Schoenberg MP, Lerner SP, Sagalowsky AI (2005) Lymphovascular invasion is independently associated with overall survival, cause-specific survival, and local and distant recurrence in Patients with negative lymph nodes at radical cystectomy. J Clin Oncol 23: 6533–6539
Lu ZQ, Li HG, Xie DR, Zhang HZ, Shen XM, Zeng YJ, Zeng H (2005) Expression and clinical significance of vascular endothelial growth factor C and vascular endothelial growth factor receptor 3 in non-small cell lung carcinoma. Ai Zheng 24: 1132–1135
Mäkinen T, Veikkola T, Mustjoki S, Karpanen T, Catimel B, Nice EC, Wise L, Mercer A, Kowalski H, Kerjaschki D, Stacker SA, Achen MG, Alitalo K (2001) Isolated lymphatic endothelial cells transduce growth, survival and migratory signals via the VEGF-C/D receptor VEGFR-3. EMBO J 20: 4762–4773
Marchetti C (1996) Weibel-Palade bodies and lymphatic endothelium: observations in the lymphatic vessels of normal and inflamed human dental pulps. Vasa 25: 337–340
Maruyama K, Ii M, Cursiefen C, Jackson DG, Keino H, Tomita M, Van Rooijen N, Takenaka H, D’Amore PA, Stein-Streilein J, Losordo DW, Streilein JW (2005) Inflammation-induced lymphangiogenesis in the cornea arises from CD11b-positive macrophages. J Clin Invest 115: 2363–2372
Massi D, Puig S, Franchi A, Malvehy J, Vidal-Sicart S, Gonzalez-Cao M, Baroni G, Ketabchi S, Palou J, Santucci M (2006) Tumour lymphangiogenesis is a possible predictor of sentinel lymph node status in cutaneous melanoma: a case–control study. J Clin Pathol 59: 166–173
Mathur SP, Mathur RS, Gray EA, Lane D, Underwood PG, Kohler M, Creasman WT (2005) Serum vascular endothelial growth factor C (VEGF-C) as a specific biomarker for advanced cervical cancer: Relationship to insulin-like growth factor II (IGF-II), IGF binding protein 3 (IGF-BP3) and VEGF-B. Gynecol Oncol 98: 467–483
Maula SM, Luukkaa M, Grenman R, Jackson D, Jalkanen S, Ristamaki R (2003) Intratumoral lymphatics are essential for the metastatic spread and prognosis in squamous cell carcinomas of the head and neck region. Cancer Res 63: 1920–1926
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2005) REporting recommendations for tumor MARKer prognostic studies (REMARK). Nat Clin Pract Urol 2: 416–422
Mitsuhashi A, Suzuka K, Yamazawa K, Matsui H, Seki K, Sekiya S (2005) Serum vascular endothelial growth factor (VEGF) and VEGF-C levels as tumor markers in patients with cervical carcinoma. Cancer 103: 724–730
Miyata Y, Kanda S, Ohba K, Nomata K, Hayashida Y, Eguchi J, Hayashi T, Kanetake H (2006) Lymphangiogenesis and angiogenesis in bladder cancer: prognostic implications and regulation by vascular endothelial growth factors-A, -C, and -D. Clin Cancer Res 12: 800–806
Morisada T, Oike Y, Yamada Y, Urano T, Akao M, Kubota Y, Maekawa H, Kimura Y, Ohmura M, Miyamoto T, Nozawa S, Koh GY, Alitalo K, Suda T (2005) Angiopoietin-1 promotes LYVE-1-positive lymphatic vessel formation. Blood 105: 4649–4656
Mou JH, Yan XC, Li ZP, Wang D, Duan GJ, Xiang DB, Xiao HL, Zhang QH (2005) Characteristic and clinicopathologic significance of lymphangiogenesis in colorectal cancer. Zhonghua Bing Li Xue Za Zhi 34: 348–352
Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, Barrera JL, Mohar A, Verastegui E, Zlotnik A (2001) Involvement of chemokine receptors in breast cancer metastasis. Nature 410: 50–56
Nakamura Y, Yasuoka H, Tsujimoto M, Imabun S, Nakahara M, Nakao K, Nakamura M, Mori I, Kakudo K (2005) Lymph vessel density correlates with nodal status, VEGF-C expression, and prognosis in breast cancer. Breast Cancer Res Treat 91: 125–132
Nakamura Y, Yasuoka H, Tsujimoto M, Kurozumi K, Nakahara M, Nakao K, Kakudo K (2006) Importance of lymph vessels in gastric cancer: a prognostic indicator in general and a predictor for lymph node metastasis in early stage cancer. J Clin Pathol 59: 77–82
Nakamura Y, Yasuoka H, Tsujimoto M, Yang Q, Imabun S, Nakahara M, Nakao K, Nakamura M, Mori I, Kakudo K (2003) Flt-4-positive vessel density correlates with vascular endothelial growth factor-D expression, nodal status, and prognosis in breast cancer. Clin Cancer Res 9: 5313–5317
Nathanson SD, Anaya P, Avery M, Hetzel FW, Sarantou T, Havstad S (1997) Sentinel lymph node metastasis in experimental melanoma: relationships among primary tumor size, lymphatic vessel diameter and 99mTc-labeled human serum albumin clearance. Ann Surg Oncol 4: 161–168
Niakosari F, Kahn HJ, Marks A, From L (2005) Detection of lymphatic invasion in primary melanoma with monoclonal antibody D2–40: a new selective immunohistochemical marker of lymphatic endothelium. Arch Dermatol 141: 440–444
Nibbs RJB, Kriehuber E, Ponath PD, Parent D, Qin S, Campbell JDM, Henderson A, Kerjaschki D, Maurer D, Graham GJ, Rot A (2001) The {beta}-chemokine receptor D6 is expressed by lymphatic endothelium and a subset of vascular tumors. Am J Pathol 158: 867–877
Oh SJ, Jeltsch MM, Birkenhager R, McCarthy JE, Weich HA, Christ B, Alitalo K, Wilting J (1997) VEGF and VEGF-C: specific induction of angiogenesis and lymphangiogenesis in the differentiated avian chorioallantoic membrane. Dev Biol 188: 96–109
Ohno M, Nakamura T, Kunimoto Y, Nishimura K, Chung-Kang C, Kuroda Y (2003) Lymphagenesis correlates with expression of vascular endothelial growth factor-C in colorectal cancer. Oncol Rep 10: 939–943
Omachi T, Kawai Y, Mizuno R, Nomiyama T, Miyagawa S, Ohhashi T, Nakayama J (2006) Immunohistochemical demonstration of proliferating lymphatic vessels in colorectal carcinoma and its clinicopathological significance. Cancer Lett (in press)
Onogawa S, Kitadai Y, Amioka T, Kodama M, Cho S, Kuroda T, Ochiumi T, Kimura S, Kuwai T, Tanaka S, Chayama K (2005) Expression of vascular endothelial growth factor (VEGF)-C and VEGF-D in early gastric carcinoma: correlation with clinicopathological parameters. Cancer Lett 226: 85–90
Partanen TA, Alitalo K, Miettinen M (1999) Lack of lymphatic vascular specificity of vascular endothelial growth factor receptor 3 in 185 vascular tumors. Cancer 86: 2406–2412
Pepper MS, Skobe M (2003b) Lymphatic endothelium: morphological, molecular and functional properties. J Cell Biol 163: 209–213
Pepper MS, Tille JC, Nisato R, Skobe M (2003a) Lymphangiogenesis and tumor metastasis. Cell Tissue Res 314: 167–177
Petrova TV, Makinen T, Makela TP, Saarela J, Virtanen I, Ferrell RE, Finegold DN, Kerjaschki D, Yla-Herttuala S, Alitalo K (2002) Lymphatic endothelial reprogramming of vascular endothelial cells by the Prox-1 homeobox transcription factor. EMBO J 21: 4593–4599
Podgrabinska S, Braun P, Velasco P, Kloos B, Pepper MS, Jackson DG, Skobe M (2002) Molecular characterization of lymphatic endothelial cells. PNAS 99: 16069–16074
Prevo R, Banerji S, Ferguson DJP, Clasper S, Jackson DG (2001) Mouse LYVE-1 is an endocytic receptor for hyaluronan in lymphatic endothelium. J Biol Chem 276: 19420–19430
Religa P, Cao R, Bjorndahl M, Zhou Z, Zhu Z, Cao Y (2005) Presence of bone marrow-derived circulating progenitor endothelial cells in the newly formed lymphatic vessels. Blood 106: 4184–4190
Renyi-Vamos F, Tovari J, Fillinger J, Timar J, Paku S, Kenessey I, Ostoros G, Agocs L, Soltesz I, Dome B (2005) Lymphangiogenesis correlates with lymph node metastasis, prognosis, and angiogenic phenotype in human non-small cell lung cancer. Clin Cancer Res 11: 7344–7353
Roma AA, Magi-Galluzzi C, Kral MA, Jin TT, Klein EA, Zhou M (2006) Peritumoral lymphatic invasion is associated with regional lymph node metastases in prostate adenocarcinoma. Mod Pathol 19: 392–398
Rubbia-Brandt L, Terris B, Giostra E, Dousset B, Morel P, Pepper MS (2004) Lymphatic vessel density and vascular endothelial growth factor-C expression correlate with malignant behavior in human pancreatic endocrine tumors. Clin Cancer Res 10: 6919–6928
Sacchi G, Weber E, Agliano M, Cavina N, Comparini L (1999) Lymphatic vessels of the human heart: precollectors and collecting vessels. A morpho-structural study. J Submicrosc Cytol Pathol 31: 515–525
Saeki H, Moore AM, Brown MJ, Hwang ST (1999) Cutting edge: secondary lymphoid-tissue chemokine (SLC) and CC chemokine receptor 7 (CCR7) participate in the emigration pathway of mature dendritic cells from the skin to regional lymph nodes. J Immunol 162: 2472–2475
Salven P, Mustjoki S, Alitalo R, Alitalo K, Rafii S (2003) VEGFR-3 and CD133 identify a population of CD34+ lymphatic/vascular endothelial precursor cells. Blood 101: 168–172
Schacht V, Dadras SS, Johnson LA, Jackson DG, Hong YK, Detmar M (2005) Up-regulation of the lymphatic marker podoplanin, a mucin-type transmembrane glycoprotein, in human squamous cell carcinomas and germ cell tumors. Am J Pathol 166: 913–921
Schmelz M, Franke WW (1993) Complexus adhaerentes, a new group of desmoplakin-containing junctions in endothelial cells: the syndesmos connecting retothelial cells of lymph nodes. Eur J Cell Biol 61: 274–289
Schoppmann SF, Bayer G, Aumayr K, Taucher S, Geleff S, Rudas M, Kubista E, Hausmaninger H, Samonigg H, Gnant M, Jakesz R, Horvat R (2004) Prognostic value of lymphangiogenesis and lymphovascular invasion in invasive breast cancer. Ann Surg 240: 306–312
Schoppmann SF, Birner P, Stockl J, Kalt R, Ullrich R, Caucig C, Kriehuber E, Nagy K, Alitalo K, Kerjaschki D (2002) Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am J Pathol 161: 947–956
Shayan R, Achen MG, Stacker SA (2006) Lymphatic vessels in cancer metastasis: bridging the gaps. Carcinogenesis 27: 1729–1738
Shida A, Fujioka S, Ishibashi Y, Kobayashi K, Nimura H, Mitsumori N, Suzuki Y, Kawakami M, Urashima M, Yanaga K (2005) Prognostic significance of vascular endothelial growth factor D in gastric carcinoma. World J Surg 29: 1600–1607
Shields JD, Borsetti M, Rigby H, Harper SJ, Mortimer PS, Levick JR, Orlando A, Bates DO (2004) Lymphatic density and metastatic spread in human malignant melanoma. Br J Cancer 90: 693–700
Shin JW, Min M, Larrieu-Lahargue F, Canron X, Kunstfeld R, Nguyen L, Henderson JE, Bikfalvi A, Detmar M, Hong YK (2005) Prox1 promotes lineage-specific expression of FGF receptor-3 in lymphatic endothelium: a role for FGF signaling in lymphangiogenesis. Mol Biol Cell E05–E04
Sipos B, Klapper W, Kruse ML, Kalthoff H, Kerjaschki D, Kloppel G (2004) Expression of lymphangiogenic factors and evidence of intratumoral lymphangiogenesis in pancreatic endocrine tumors. Am J Pathol 165: 1187–1197
Skobe M, Hawighorst T, Jackson DG, Prevo R, Janes L, Velasco P, Riccardi L, Alitalo K, Claffey K, Detmar M (2001) Induction of tumor lymphangiogenesis by VEGF-C promotes breast cancer metastasis. Nat Med 7: 192–198
Sleeman JP, Krishnan J, Kirkin V, Baumann P (2001) Markers for the lymphatic endothelium: in search of the Holy Grail? Microsc Res Tech 55: 61–69
Stacker SA, Achen MG, Jussila L, Baldwin ME, Alitalo K (2002) Lymphangiogenesis and cancer metastasis. Nat Rev Cancer 2: 573–583
Stacker SA, Caesar C, Baldwin ME, Thornton GE, Williams RA, Prevo R, Jackson DG, Nishikawa S, Kubo H, Achen MG (2001) VEGF-D promotes the metastatic spread of tumor cells via the lymphatics. Nat Med 7: 186–191
Stessels F, Van den Eynden G, Van der Auwera I, Salgado R, Van den Heuvel E, Harris AL, Jackson DG, Colpaert CG, Van Marck E, Dirix LY, Vermeulen PB (2004) Breast adenocarcinoma liver metastases, in contrast to colorectal cancer liver metastases, display a non-angiogenic growth pattern that preserves the stroma and lacks hypoxia. Br J Cancer 90: 1429–1436
Straume O, Jackson DG, Akslen LA (2003) Independent prognostic impact of lymphatic vessel density and presence of low-grade lymphangiogenesis in cutaneous melanoma. Clin Cancer Res 9: 250–256
Strauss L, Volland D, Kunkel M, Reichert TE (2005) Dual role of VEGF family members in the pathogenesis of head and neck cancer (HNSCC): possible link between angiogenesis and immune tolerance. Med Sci Monit 11: BR280–BR292
Swartz MA, Skobe M (2001) Lymphatic function, lymphangiogenesis, and cancer metastasis. Microsc Res Tech 55: 92–99
Takanami I (2006) Lymphatic microvessel density using D2–40 is associated with nodal metastasis in non-small cell lung cancer. Oncol Rep 15: 437–442
Tamura M, Oda M, Matsumoto I, Tsunezuka Y, Kawakami K, Ohta Y, Watanabe G (2004a) The combination assay with circulating vascular endothelial growth factor (VEGF)-C, matrix metalloproteinase-9, and VEGF for diagnosing lymph node metastasis in patients with non-small cell lung cancer. Ann Surg Oncol 11: 928–933
Tamura M, Oda M, Tsunezuka Y, Matsumoto I, Kawakami K, Ohta Y, Watanabe G (2004b) Chest CT and serum vascular endothelial growth factor-C level to diagnose lymph node metastasis in patients with primary non-small cell Lung Cancer. Chest 126: 342–346
Tamura M, Ohta Y (2003) Serum vascular endothelial growth factor-C level in patients with primary nonsmall cell lung carcinoma: a possible diagnostic tool for lymph node metastasis. Cancer 98: 1217–1222
Thiele W, Sleeman JP (2006) Tumor-induced lymphangiogenesis: a target for cancer therapy? J Biotechnol
Trojan L, Michel MS, Rensch F, Jackson DG, Alken P, Grobholz R (2004) Lymph and blood vessel architecture in benign and malignant prostatic tissue: lack of lymphangiogenesis in prostate carcinoma assessed with novel lymphatic marker lymphatic vessel endothelial hyaluronan receptor (LYVE-1). J Urol 172: 103–107
Valtola R, Salven P, Heikkila P, Taipale J, Joensuu H, Rehn M, Pihlajaniemi T, Weich H, deWaal R, Alitalo K (1999) VEGFR-3 and its ligand VEGF-C are associated with angiogenesis in breast cancer. Am J Pathol 154: 1381–1390
Van den Eynden GG, Van der Auwera I, Van Laere SJ, Colpaert CG, Turley H, Harris AL, van Dam P, Dirix LY, Vermeulen PB, van Marck EA (2005) Angiogenesis and hypoxia in lymph node metastases is predicted by the angiogenesis and hypoxia in the primary tumour in patients with breast cancer. Br J Cancer 93: 1128–1136
Van den Eynden GG, Van der Auwera I, Van Laere SJ, Huygelen V, Colpaert CG, van Dam P, Dirix LY, Vermeulen PB, Van Marck EA (2006) Induction of lymphangiogenesis in and around axillary lymph node metastases of patients with breast cancer. Br J Cancer [E-pub ahead of print]
Van der Auwera I, Van den Eynden GG, Colpaert CG, Van Laere SJ, van Dam P, Van Marck EA, Dirix LY, Vermeulen PB (2005) Tumor lymphangiogenesis in inflammatory breast carcinoma: a histomorphometric study. Clin Cancer Res 11: 7637–7642
Van der Auwera I, Van Laere SJ, Van den Eynden GG, Benoy I, van Dam P, Colpaert CG, Fox SB, Turley H, Harris AL, Van Marck EA, Vermeulen PB, Dirix LY (2004) Increased angiogenesis and lymphangiogenesis in inflammatory vs noninflammatory breast cancer by real-time reverse transcriptase-PCR gene expression quantification. Clin Cancer Res 10: 7965–7971
Van Trappen PO, Steele D, Lowe DG, Baithun S, Beasley N, Thiele W, Weich H, Krishnan J, Shepherd JH, Pepper MS, Jackson DG, Sleeman JP, Jacobs IJ (2003) Expression of vascular endothelial growth factor (VEGF)-C and VEGF-D, and their receptor VEGFR-3, during different stages of cervical carcinogenesis. J Pathol 201: 544–554
Vazquez-Sequeiros E, Wang L, Burgart L, Harmsen W, Zinsmeister A, Allen M, Jondal M, Wiersema M (2002) Occult lymph node metastases as a predictor of tumor relapse in patients with node-negative esophageal carcinoma. Gastroenterology 122: 1815–1821
Veikkola T, Jussila L, Makinen T, Karpanen T, Jeltsch M, Petrova TV, Kubo H, Thurston G, McDonald DM, Achen MG, Stacker SA, Alitalo K (2001) Signalling via vascular endothelial growth factor receptor-3 is sufficient for lymphangiogenesis in transgenic mice. EMBO J 20: 1223–1231
Vermeulen PB, Gasparini G, Fox SB, Colpaert C, Marson LP, Gion M, Belien JA, de Waal RM, Van Marck E, Magnani E, Weidner N, Harris AL, Dirix LY (2002) Second international consensus on the methodology and criteria of evaluation of angiogenesis quantification in solid human tumours. Eur J Cancer 38: 1564–1579
Vermeulen PB, Gasparini G, Fox SB, Toi M, Martin L, McCulloch P, Pezzella F, Viale G, Weidner N, Harris AL, Dirix LY (1996) Quantification of angiogenesis in solid human tumours: an international consensus on the methodology and criteria of evaluation. Eur J Cancer 32A: 2474–2484
Von Marschall Z, Scholz A, Stacker SA, Achen MG, Jackson DG, Alves F, Schirner M, Haberey M, Thierauch KH, Wiedenmann B, Rosewicz S (2005) Vascular endothelial growth factor-D induces lymphangiogenesis and lymphatic metastasis in models of ductal pancreatic cancer. Int J Oncol 27: 669–679
Wang TB, Huang YH, Lan P, Song XM, Wang JP (2005) Correlation of lymphangiogenesis to progression of colorectal cancer. Ai Zheng 24: 1276–1279
Weidner N, Semple JP, Welch WR, Folkman J (1991) Tumor angiogenesis and metastasis – correlation in invasive breast carcinoma. N Engl J Med 324: 1–8
Wetterwald A, Hoffstetter W, Cecchini MG, Lanske B, Wagner C, Fleisch H, Atkinson M (1996) Characterization and cloning of the E11 antigen, a marker expressed by rat osteoblasts and osteocytes. Bone 18: 125–132
Wigle JT, Oliver G (1999) Prox1 function is required for the development of the murine lymphatic system. Cell 98: 769–778
Williams CS, Leek RD, Robson AM, Banerji S, Prevo R, Harris AL, Jackson DG (2003) Absence of lymphangiogenesis and intratumoural lymph vessels in human metastatic breast cancer. J Pathol 200: 195–206
Yasuoka H, Nakamura Y, Zuo H, Tang W, Takamura Y, Miyauchi A, Nakamura M, Mori I, Kakudo K (2005) VEGF-D expression and lymph vessels play an important role for lymph node metastasis in papillary thyroid carcinoma. Mod Pathol 18: 1127–1133
Yonemura Y, Fushida S, Bando E, Kinoshita K, Miwa K, Endo Y, Sugiyama K, Partanen T, Yamamoto H, Sasaki T (2001) Lymphangiogenesis and the vascular endothelial growth factor receptor (VEGFR)-3 in gastric cancer. Eur J Cancer 37: 918–923
Zeng Y, Opeskin K, Horvath LG, Sutherland RL, Williams ED (2005) Lymphatic vessel density and lymph node metastasis in prostate cancer. Prostate 65: 222–230
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Van der Auwera, I., Cao, Y., Tille, J. et al. First international consensus on the methodology of lymphangiogenesis quantification in solid human tumours. Br J Cancer 95, 1611–1625 (2006). https://doi.org/10.1038/sj.bjc.6603445
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603445
Keywords
This article is cited by
-
Clinicopathological Significance of Tumor Lymphatic Vessel Density in Head and Neck Squamous Cell Carcinoma
Indian Journal of Otolaryngology and Head & Neck Surgery (2018)
-
Intratumoral and peritumoral lymphatic vessel density both correlate with lymph node metastasis in breast cancer
Scientific Reports (2017)
-
Leptin promotes VEGF-C production and induces lymphangiogenesis by suppressing miR-27b in human chondrosarcoma cells
Scientific Reports (2016)
-
The role of lymphangiogenesis and angiogenesis in tumor metastasis
Cellular Oncology (2016)
-
Extracellular matrix protein 1 is correlated to carcinogenesis and lymphatic metastasis of human gastric cancer
World Journal of Surgical Oncology (2014)