Abstract
This study assessed the prognostic value of several markers involved in gliomagenesis, and compared it with that of other clinical and imaging markers already used. Four-hundred and sixteen adult patients with newly diagnosed glioma were included over a 3-year period and tumour suppressor genes, oncogenes, MGMT and hTERT expressions, losses of heterozygosity, as well as relevant clinical and imaging information were recorded. This prospective study was based on all adult gliomas. Analyses were performed on patient groups selected according to World Health Organization histoprognostic criteria and on the entire cohort. The endpoint was overall survival, estimated by the Kaplan–Meier method. Univariate analysis was followed by multivariate analysis according to a Cox model. p14ARF, p16INK4A and PTEN expressions, and 10p 10q23, 10q26 and 13q LOH for the entire cohort, hTERT expression for high-grade tumours, EGFR for glioblastomas, 10q26 LOH for grade III tumours and anaplastic oligodendrogliomas were found to be correlated with overall survival on univariate analysis and age and grade on multivariate analysis only. This study confirms the prognostic value of several markers. However, the scattering of the values explained by tumour heterogeneity prevents their use in individual decision-making.
Similar content being viewed by others
Main
The estimated incidence of adult gliomas in Europe and the United States is 4–5 per 100 000 inhabitants. The most malignant form is glioblastoma multiforme (GBM), the commonest primary brain tumour in adults with an estimated incidence of 2–3 per 100 000 inhabitants and that has a very poor prognosis with a median survival of about 40–48 weeks despite surgery, radiotherapy and chemotherapy (Laws et al, 2003; Stark et al, 2005). Chemotherapy provides a sometimes questionable and, at best, limited benefit (Stewart, 2002; Stark et al, 2005; Stupp et al, 2005). However, the development of new treatment protocols over recent years (Board and Jayson, 2005) and the emergence of new therapeutic concepts (Board and Jayson, 2005; Galanis et al, 2005; Haas-Kogan et al, 2005; Mellinghoff et al, 2005; Hall and Vallera, 2006; Sathornsumetee et al, 2007) have accentuated the need to characterize potential candidates for treatments as precisely as possible. Although the diagnostic standard is the World Health Organization (WHO) histoprognostic classification, which can be used to define homogeneous patient groups in terms of prognosis (Kleihues and Webster, 2000), some patients do not present the expected outcome. In parallel, recent progress in molecular biology has allowed determination of numerous markers in routine clinical practice, but raises the question of their capacity to improve patient management (Boudreau et al, 2005). The purpose of the present study was to answer this question with respect to certain markers that have already been shown to play a role in gliomagenesis. Published studies on this subject are retrospective and usually based on patients selected according to a particular histoprognostic group or treatment modalities. To the best of our knowledge, this is the first large-scale prospective study based on all adult gliomas.
Patients and methods
Study design and inclusion criteria Two centres participated in the study: the Poitiers and Angers university hospitals, in France. Tissues from these glial tumours were collected during surgery after obtaining signed informed consent from all patients, approval from the Poitou-Charentes ethics committee and in accordance with the precepts established by the Helsinki Declaration. All adult patients in whom a diagnosis of glioma was suspected were prospectively and consecutively preincluded and were definitively included after confirmation of the diagnosis based on WHO histopathologic criteria. These glial tumors encompass: (i) diffusely infiltrating astrocytomas (i.e., diffuse astrocytomas, anaplastic astrocytomas and glioblastoma multiforme), (ii) oligodendroglial tumours (i.e., oligodendroglioma and anaplastic oligodendroglioma) and (iii) mixed gliomas (i.e., oligoastrocytoma and anaplastic oligoastrocytoma) (Kleihues and Webster, 2000). These patients had no particular past medical history, especially no history of brain surgery, brain radiation therapy or chemotherapy. Distribution of the patients according to the WHO classification is presented in Table 1. Tumour diagnosis and grading were established according to the WHO criteria (Kleihues and Webster, 2000) and were systematically revised in each centre by two expert neuropathologists. Four-hundred and sixteen patients were included from 1 September 2002 to 31 December 2005, and patients not satisfying the inclusion criteria after quality control were excluded from the analysis. Median follow-up is 14 months for all patients, and 29 months for patients who were alive. This series also included three tumour-free patients, operated for refractory epilepsy, obtained from Neurobiotec® (Lyon, France) after ethics committee approval. The main demographic data are presented in Table 1. The primary endpoint was overall survival (OS).
Methods
The following molecular markers were included in this study: (i) expression of oncogenes EGFR, PDGF and VEGF, (ii) expression of tumour suppressor genes p14ARF, p16INK4A and PTEN, (iii) expression of O6-methylguanine DNA methyltransferase (MGMT) and (iv) expression of the catalytic subunit (hTERT) of telomerase. In addition, cytogenetic parameters, including loss of heterozygosity (LOH), were also collected: 1p, 2p23, 9p, 10p, 10q23, 10q26, 11q, 13q, 17q, 19q, 22q. Clinical data were recorded: age, treatment received, comprising various combinations of surgery, radiotherapy and chemotherapy, including temozolomide (TMZ), OS, histoprognostic types and grades according to WHO grading criteria. Finally, preoperative CT and MRI imaging data systematically performed without and with injection of contrast agent and were recorded. Gene expression was determined by quantitative RT-PCR using the Taqman® gene expression assays kit for each gene, and the device ABIPrism 7000 (Applera®) was used. The method used has been previously described (Wager et al, 2006). Three modalities of gene expression were defined according to the following cutoff values: decreased: more than one and a half times lower than the control value, normal: from one and a half times lower to one and a half times higher than the control value and increased: more than one and a half times higher than control value. LOH was determined by the microsatellite method. Microsatellite markers and cytogenetic bands and the corresponding genes, when they are known, are shown as additional data. The end point was the correlation between the parameters available on inclusion and OS. Two types of parameters were selected: those already known to be independent prognostic factors and those tested by studying the levels of expression and LOH. This study is not a therapeutic trial. Individual therapeutic options and treatments were proposed and decided independently of inclusion in the study. Of note, TMZ was used since the start of the study (2002). Details of patient treatment appear on Table 2.
Statistical analysis
Data were collected from the date of inclusion. Differences between groups in presenting characteristics were tested using the Mann–Whitney U-test. OS was analysed by calculating the time interval between date of inclusion and date of death from any cause, or date of the last follow-up for surviving patients, and then estimated by the Kaplan–Meier method. The following clinical and biological features were analysed as potential prognostic factors for survival: age, grade (‘high’ vs ‘low’), treatment (surgery+radiotherapy+TMZ, vs surgery+radiotherapy±other chemotherapy, vs others), loss of heterozygosities, relative expression of p14ARF, p16INK4A, PTEN, EGFR, PDGF, VEGF, MGMT and expression of hTERT. Tested transcripts were categorized in three groups according to the fold change as compared with control, cutoff being set at 1.5 above for overexpression level or 1.5 below the normal expression value for underexpression level. Age and hTERT expression were categorized according to the upper and lower quartiles of their respective values. All variables were assessed in univariate analysis using the two-tailed log rank or Wilcoxon test as appropriate. To summarise prognostic information, variables found to be associated at the 20% level with the outcome were entered into a Cox regression model on the basis of likelihood ratio test and potential interactions were tested. A step-down procedure allowed to retain those variables adding to each other prognostic information. Levels of significance were represented by P-values derived from two-sided tests. A P-value <0.05 or less was considered to indicate statistical significance. SAS v 8 (Statistical Analysis System, Cary, NC, USA) software package was used.
Results
Expression values are presented in Table 3.
Univariate analysis
Relation of expressions with OS
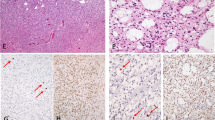
The prognostic importance (Figure 1 and Table 4A) of clinical features at baseline, treatment, relative gene expression of p14ARF, p16INK4A, PTEN, EGFR, PDGF and VEGF and the expression of hTERT in univariate analysis is summarized in Table 4A.
Of clinical relevance, three factors were considered: age, grade (‘high’ vs ‘low’) and contrast enhancement (P<10−4). When tested individually, p14ARF, p16INK4A and PTEN provided prognostic information (P<0.05), overexpression being associated to a better survival (Figure 1). Among other factors, the relative expression of VEGF, the expression of hTERT were considered as potential prognostic factors, underexpression or low expression, respectively, showing a slight advantage, as well as EGFR with a very slight advantage when overexpression. Treatment was also considered and categorized as follows: surgery+radiotherapy+TMZ, vs surgery+radiotherapy±other chemotherapy vs others.
No correlation was observed between MGMT expression and survival, either for the entire cohort or for each WHO histopathologic group but a correlation was observed between MGMT expression and grade classified as ‘high-grade’ (higher expression) vs ‘low-grade’ (P=0.0126). No correlation was observed between astrocytic or oligodendroglial tumour phenotypes and the level of MGMT expression.
Relation of LOH with OS
For the entire cohort, 10p15 (carrying KLF6), 10q23 (PTEN), 10q26 (DMBT1) and 13q (Rb1) LOH were correlated with OS. 10q26 was correlated with OS of high-grade tumours and also with grade III oligodendrogliomas OS. No correlation was observed between OS of patients with low-grade tumours and the various laboratory parameters studied (Figures 2 and 3 and Table 4A).
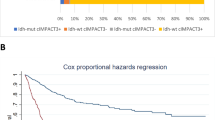
Multivariate analysis
When the eight factors that were identified in univariate analysis (P<0.20), treatment, grade and interaction between grade and treatment were entered into a Cox model, only three variables were selected with a P-value less than 0.05, namely age (P<10−4), grade (P=0.0017) and VEGF (P=0.0071) (Table 4B). The relative expression of VEGF was not retained after stepwise regression procedure. Factors that were considered adding to each other prognostic information were age and grade, which remained highly significant. The final model is presented in Table 4B.
MGMT was of no prognostic value by univariate analysis. However, when this factor was added into the Cox model based on previously published therapeutic approaches considerations, the results remained strictly similar.
Discussion
The correlations with OS observed in this study confirm data already reported for smaller retrospective series. These results will be discussed globally after a few comments on each of the main markers considered.
Expressions
A very strong analogy was observed for the results concerning p14ARF and p16INK4A, which is coherent with their localization corresponding to the ‘INK4A locus’. Hypermethylation of p14ARF has been associated with progression of astrocytomas (Watanabe et al, 2007) and has been described as a factor of poor prognosis of grade II diffuse gliomas (Watanabe et al, 2003), although its prognostic value in oligodendroglioma is more controversial (Korshunov and Golanov, 2001; Kamiya and Nakazato, 2002). p16INK4A deletion is a factor of poor prognosis of these tumours (Jeon et al, 2007). Globally, these data are coherent with concomitant inactivation of these genes during the late stage of gliomagenesis. Loss or inactivation of PTEN has been described in solid tumours of various organs, and it is mutant in about 30% of GBM, but not in low-grade gliomas and very rarely in anaplastic gliomas (Duerr et al, 1998; Zhou et al, 1999). EGFR is the main oncogene identified in brain tumours, but its prognostic value is controversial (Chakravarti et al, 2001; Muracciole et al, 2002; Miracco et al, 2003; Shinojima et al, 2003; Heimberger et al 2005a, 2005b; Kleinschmidt-DeMasters et al, 2005; Lopes-Gines et al, 2005; Quan et al, 2005; Rich et al, 2005), although a fairly strong correlation with OS was observed in the present study. PDGF is often overexpressed in gliomas, with an elevation correlated with tumour grade (Shih and Holland, 2006) and was considered to be predictive of poor prognosis in a study on grade II tumours (Varela et al, 2004). The interest in PDGF is largely due to the growing importance, over recent years, of tyrosine kinases as useful targets in the treatment of cancer (Board and Jayson, 2005). The expression of certain VEGF receptors appears to be correlated with glioma grade (Plate et al, 1992), conferring a diagnostic and prognostic value and also making VEGF a candidate for targeted therapies (Grau et al, 2006). The hTERT gene codes for the catalytic subunit of telomerase and the potential diagnostic value of hTERT expression was recently highlighted (Chakravarti et al, 2001; Tchirkov et al, 2003; La Torre et al, 2005; Boldrini et al, 2006; Maes et al, 2007; Shervington et al, 2007).
Methylation of the MGMT promoter, a frequent phenomenon, makes gliomas more sensitive to alkylating agents by reducing gene expression (Esteller et al, 2000). Several teams have reported this increased chemosensitivity for various types of gliomas (Balana et al, 2003; Paz et al, 2004; Hegi et al, 2005; Watanabe et al, 2005; Herrlinger et al, 2006; Chinot et al, 2007) and MGMT status, either methylation or level of expression, has become a predictive marker of chemosensitivity. However, although determination of this marker is recommended in the context of clinical trials involving alkylating agents, it cannot be recommended in routine clinical practice (Stupp and Hegi, 2007). It must be kept in mind that most previously reported correlative studies examined MGMT promoter methylation, whereas in the present study, the authors chose to examine MGMT gene expression and that comparison of data obtained from these different approaches are not appropriate. MGMT appeared to be more markedly overexpressed in low-grade tumours but MGMT expression was not correlated with a specific phenotype, and its level of expression has no specific prognostic value. Patients with low MGMT expression treated with alkylating agents presented a better OS than patients not treated by alkylating agents, but it must be remembered that this was not a clinical trial with randomised treatment.
LOH
Tumour progression reflects genetic instability that can be expressed by several alternative pathways in the same tumour phenotype, resulting in a correlation between the degree of anaplasia of a tumour and the percentage of LOH detected in tumour cells, although a constant profile of loss or gain related to a particular tumour phenotype has not been demonstrated. This phenomenon has been described in meningiomas, but, to the best of our knowledge, has not been previously described on a very large prospective series of adult gliomas. As for meningiomas, no constant expression profile, based on single LOH or combinations of LOH, was found to be correlated with a particular tumour phenotype. However, some LOH appear to be correlated with OS: 10q26, which carries DMBT1 (deleted in malignant brain tumours), is a possible tumour suppressor gene in glial tumours (Mollenhauer et al, 1997). It is generally accepted that passage from an anaplastic phenotype to a GBM phenotype is associated with 10q LOH (Fujisawa et al, 1999; Daido et al, 2004), although the role specifically played by DMBT1 in this progression is controversial (Sasaki et al, 2002). Taken all together, these results suggest firstly that an increased frequency of this LOH is associated with increasing grade. Secondly, its very strong correlation with survival in the grade III oligodendrogliomas group suggests a participation of DMBT1 at the anaplastic stage of gliomagenesis. LOH10p is more frequent in high-grade than in low-grade tumours and is also more frequent in tumours with a large oligodendroglial component. The present study demonstrated a link between 10p LOH and poorer survival in the overall cohort but not in the various histoprognostic groups. As 13q LOH was first observed in low-grade gliomas, it was initially thought to be involved at an early stage of gliomagenesis (Lee et al, 1995). However, it was subsequently associated with anaplastic astrocytomas and GBM (Wooten et al, 1999) and appeared to be mutually exclusive with 19q LOH (Nakamura et al, 2000).
General discussion
All of the correlations observed with OS in this study cohort, probably as a result of the large number of patients, which compensates for the scattering of data, therefore, confirm the results reported in the literature. The correlation between each marker studied and OS can, therefore, be confirmed or excluded for the overall cohort. The results of studies such as this one, can, therefore, confirm the involvement of these markers in gliomagenesis and constitute a valuable tool. However, these results have certain limitations, as these correlations with OS are observed more rarely and become less robust when based on smaller sample sizes and the very broad scattering of the results for these markers prevent any extrapolation of the conclusions drawn from this study cohort to individual patients. These conclusions, therefore, have no practical impact as an aid to individual decision-making. As this scattering is due to tumour heterogeneity, neither studies based on larger series nor studies conducted over longer periods would be able to eliminate this obstacle. Moreover, the relationship between markers and OS was observed at relatively late stages of these gliomas, and no positive correlation was observed for low-grade tumours. Finally, these relationships would only provide a diagnostic contribution when the correlation observed is higher than that of already identified markers. However, the markers correlated with OS in this study were much less robust than other previously identified prognostic indicators, such as age and treatment modalities. These markers, therefore, do not provide crucial contribution in clinical practice at the present time.
Conclusions
Application of relevant data provided by molecular biology to the treatment of cancers is a major challenge in medical oncology. In this context, it is a widely held belief that, in the years to come, these data will allow treatment tailored to each individual patient's tumour. However, the results of the present study, which, to our knowledge, is the largest prospective study ever performed to evaluate the prognostic value of biological markers in adult gliomas, tend to suggest that these markers will be of limited value for individual treatment decisions, particularly for the most heterogeneous, that is, high-grade, tumours. If tumour markers were to have a role in treatment decisions in adult gliomas, it would probably be limited to less heterogeneous, that is, low-grade, tumours, as illustrated by the study of certain p73 isoforms. The absence of correlation between LOH and OS of low-grade tumours observed in this study could be due to lower genetic instability, whereas the absence of correlation with gene expressions could be due to the fact that the genes studied here are involved in later stages of gliomagenesis.
MGMT has a special place in this context, as, although it has a poor specific prognostic value, it can be used to predict the chemosensitivity of these tumours. Although it is recommended to include MGMT in clinical trials of chemotherapy, it cannot be recommended as part of everyday clinical practice. For all of these reasons, it would, therefore, be unrealistic to expect any contribution of these markers to treatment decisions for adult patients with glioma.
When this study was initiated, tumour stem cell and pluripotent stem cell biology was only in the early stages. A growing body of literature has demonstrated the importance of these stem cells to propose an explanatory model for gliomagenesis that could possibly open the way to major therapeutic progress, as these cells constitute the genuine target of treatments. Preclinical animal models reproducing all phases of gliomas could also be used to develop a similar approach to that conducted in this study, based on whole tumours and not stem cells, which can now be specifically isolated and studied. Progress in tumour stem cell (TSC) biology has led to identification of cells possessing the specific characteristics of true glioma stem cells, specific markers (e.g. CD133), capacity for self-renewal and capacity for differentiation into the various cell lines of brain tissue (neuronal, glial) (Gilbertson and Rich, 2007). These results have led to the development of a gliomagenesis model directly resulting in GBM, which postulates the malignant transformation of these cells at the time of ‘insults’, which selectively affect the genes involved in the initial steps of carcinogenesis. Access to these tumour stem cells has now been defined by tumour culture protocols, which will allow molecular studies on much more homogeneous populations. This type of approach applied to individual tumors should result in much more effective use of markers currently identified in heterogeneous cohorts. At the same time, this type of approach would also allow a more accurate definition of the limits of treatments (e.g. resistance of TSC to radiotherapy and acquisition of resistance to chemotherapy) (Rich, 2007).
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Balana C, Ramirez J-L, Taron M, Roussos Y, Ariza A, Ballester R, Sarries C, Mendez P, Sanchez J-J, Rosell R (2003) O6-methyl-guanine-DNA methyltransferase methylation in serum and tumor DNA predicts reponse to 1,3-bis(2-chloroethyl)-1-nitrosourea but not to temozolomide plus cisplatin in glioblastoma multiforme. Clin Cancer Res 9 (4): 1461–1468
Board R, Jayson GC (2005) Platelet-derived growth factor receptor (PDGFR): a target for anticancer therapeutics. Drug Resist Updat 8: 75–83
Boldrini L, Pistolesi S, Gisfredi S, Ursino S, Ali G, Pieracci N, Basolo F, Parenti G, Fontanini G (2006) Telomerase activity and hTERT mRNA expression in glial tumors. Int J Oncol 28 (6): 1555–1560
Boudreau CR, Yang I, Liau LM (2005) Gliomas: advances in molecular analysis and characterization. Surg Neurol 64: 286–294
Chakravarti A, Delaney MA, Noll E, Black PM, Loeffler JS, Muzikansky A, Dyson NJ (2001) Prognostic and pathologic significance of quantitative protein expression profiling in human gliomas. Clin Cancer Res 7: 2387–2395
Chinot OL, Barrié M, Fuentes S, Eudes N, Lancelot S, Metellus P, Muracciole X, Braguer D, Ouafik L, Martin PM, Dufour H, Figarella-Branger D (2007) Correlation between O6- methylguanine-DNA methyltransferase and survival in inoperable newly diagnosed glioblastoma patients treated with neoadjuvant temozolomide. J Clin Oncol 25 (12): 1459–1460
Daido S, Takao S, Tamiya T, Ono Y, Terada K, Ito S, Ouchida M, Date I, Ohmoto T, Shimizu K (2004) Loss of heterozygosity on chromosome 10q associated with malignancy and prognosis in astrocytic tumors, and discovery of novel loss regions. Oncol Rep 12 (4): 789–795
Duerr EM, Rollbrocker B, Hayashi Y, Peters N, Meyer-Puttlitz B, Louis DN, Schramm J, Wiestler OD, Parsons R, Eng C, vonDeimling A (1998) PTEN mutations in gliomas and glioneuronal tumors. Oncogene 16 (17): 2259–2264
Esteller M, Garcia-Foncilla J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, Baylin SB, Herman JG (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343: 1350–1354
Fujisawa H, Kurrer M, Reis RM, Yonekawa Y, Kleihues P, Ohgaki H (1999) Acquisition of the glioblastoma phenotype during astrocytoma progression is associated with loss of heterozygosity on 10q25-qter. Am J Pathol 155 (2): 387–394
Galanis E, Buckner JC, Maurer MJ, Kreisberg JI, Ballman K, Boni J, Peralba JM, Jenkins RB, Dakhil SR, Morton RF, Jaeckle KA, Sheithauer BW, Dancey J, Idalgo M, Walsh DJ (2005) Phase II trail of Temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group study. J Clinl Oncol 23 (23): 5294–5304
Gilbertson RJ, Rich JN (2007) Making a tumour's bed: glioblastoma stem cells and the vascular niche. Nat Rev Cancer 7 (10): 733–736
Grau SJ, Trillsch F, Herms J, Thon N, Nelson PJ, Tonn JC, Goldbrunner R (2006) Expression of VEGFR 3 in glioma endothelium correlates with tumor grade. J Neurooncol 82 (2): 141–150
Haas-Kogan DA, Prados MD, Tihan T, Berhard DA, Jelluma N, Arvold ND, Baumber R, Lamborn KR, Kapadia A, Malec M, Berger MS, Stokoe D (2005) Epidermal growth factor receptor, protein kinase B/Akt, and glioma response to erlotinib. J Natl Cancer Inst 97 (12): 880–887
Hall WA, Vallera DA (2006) Efficacy of antiangiogenic targeted toxins against glioblastoma multiforme. Neurosurg Focus 20 (4): E23
Hegi ME, Diserens AC, Gorlia T, Hamou MF, DeTribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JEC, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 350 (10): 997–1003
Heimberger AB, Hlatky R, Suki D, Yang D, Weinberg J, Gilbert M, Sawaya R, Aldape K (2005a) Prognostic effect of epidermal growth factor receptor and EGFRvIII in glioblastoma multiforme patients. Clin Cancer Res 11 (4): 42–46
Heimberger AB, Suki D, Yang D, Shi W, Aldape K (2005b) The natural history of EGFR and EGFRvIII in glioblastoma patients. J Transl Med 3: 38
Herrlinger U, Rieger J, Koch D, Loeser S, Blaschke B, Kortmann RD, Steinbach JP, Hundsberger T, Wick W, Meyermann R, Tan TC, Sommer C, Bamberg M, Reifenberger G, Weller M (2006) Phase II trail of lomustine plus temozolomide chemotherapy in addition to radiotherapy in newly diagnosed glioblastoma: UKT-03. J Clin Oncol 24 (27): 4412–4417
Jeon YK, Park K, Park CK, Paek SH, Jung HW, Park SH (2007) Chromosome 1p and 19q status and p53 and p16 expression patterns as prognostic indicators of oligodendroglial tumors: a clinicopathological study using fluorescence in situ hybridisation. Neuropathology 27: 10–20
Kamiya M, Nakazato Y (2002) The expression of cell cycle regulatory proteins in oligodendroglial tumors. Clin Neuropathol 21 (2): 52–65
Kleihues P, Webster KC (2000) World Health Oranization Classification of Tumours: ‘Tumours of the Nervous System. Pathology and Genetics’. IARC Press: Lyon
Kleinschmidt-DeMasters BK, lillehei KO, Varella-Garcia M (2005) Glioblastoma in the older old. Arch Pathol Lab Med 129 (5): 624–631
Korshunov A, Golanov A (2001) Immunohistochemical analysis of p18INK4C and p14ARF protein expression in 117 oligodendrogliomas. Arch Pathol Lab Med 126 (1): 42–48
La Torre D, De Divitiis O, Conti A, Angileri FF, Cardali S, Aguennouz M, Aragona M, Panetta S, Avella D, Vita G, La Torre F, Tomasello F (2005) Expression of telomeric repeat binding factor-1 in astroglial brain tumors. Neurosurg 56 (4): 802–810
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, Lillehei KO, Bernstein M, Brem H, Sloan A, Berger MS, Chang S, Glioma Outcomes Investigators (2003) Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg 99 (3): 467–473
Lee SH, Kim JH, Rhee CH, Kang YS, Lee JH, Hong SI, Choi KS (1995) Loss of heterozygozyty on chromosome 10, 13q(Rb), 17p, and p53 gene mutations in human brain gliomas. J Korean Med Sci 10 (6): 442–448
Lopes-Gines C, Cerda-Nicolas M, Gil-Benso R, Pellin A, Lopez-Guerrero JA, Callaghan R, Benito R, Roldan P, Piquer J, Llacer J, Barbera J (2005) Association of chromosome 7, chromosome 10 and EGFR gene amplification in glioblastoma multiforme. Clin Neuropathol 24 (5): 209–218
Maes L, Kalala J-P, Cornelissen M, deRidder L (2007) Progression of astrocytomas and meningiomas: an evaluation in vitro. Cell Prolif 40 (1): 14–23
Mellinghoff IK, Wang MY, Vivanco I, Haas-Kogan DA, Zhu S, Dia EQ, Lu KV, Yoshimoto K, Huang JH, Chute DJ, Riggs BL, Horvath S, Liau LM, Cavenee WK, Rao PN, Beroukhim R, Peck TC, Lee JC, Sellers WR, Stokoe D, Prados M, Cloughesy TF, Sawyers CL, Mischel PS (2005) Molecular determinants of the response of glioblastomas to EGFR kinase inhibitors. N Engl J Med 353 (19): 1997–1999
Miracco C, De Santi MM, Luzi P, Lalinga AV, laurini L, DeNisi MC, Angeloni G, Brogi M, Cardone C, Carducci A, Arcuri F, Tosi P, Rubino G, Pirtoli L (2003) In situ detection of telomeres by fluorescence in situ hybridization and telomerase activity in glioblastoma multiforme: correlation with p53 status, EGFR, c-myc, MIB1, and topoisomerase Iialpha protein expression. Int J Oncol 23 (6): 1529–1535
Mollenhauer J, Wiermann S, Scheurlen W, Korn B, Hayashi Y, Wilgenbus KK, Von Deimling A, Poustka A (1997) DMBT1, a new member of the SRCR superfamily, on chromosome 10q25.3–26.1 is deleted in malignant brain tumours. Nat Genet 17: 32–39
Muracciole X, Romain S, Dufour H, Palmari J, Chinot O, Ouafik L, Grisoli F, Branger DF, Martin PM (2002) PAI-1 and EGFR expression in adult glioma tumors: toward a molecular prognostic classification. Int J Radiat Oncol Biol Phys 52 (3): 592–598
Nakamura M, Yang F, Fujisawa H, Yonckawa P, Ohgaki H (2000) Loss of heterozygosity on chromosome 19 in secondary glioblastomas. J Neuropathol Exp Neurol 59 (6): 539–543
Paz MF, Yaya-Tur R, Rojas-Marcos I, Reynes G, Pollan M, Aguirre-Cruz L, Garcia-Lopez JL, Piquer J, Safont MJ, Balana C, Sanchez-Cespedes M, Garcia-Villanueva M, Arribas L, Esteller M (2004) CpG island hypermethylation of the DNA repair enzyme methyltransferase predicts response to temozolomide in primary gliomas. Clin Cancer Res 10 (15): 4933–4938
Plate KH, Breier G, Weich HA, Risau W (1992) Vascular endothelial growth factor is a potential tumor angiogenesis factor in human gliomas in vivo. Nature 359: 846–847
Quan AL, Barnett GH, Lee SY, Volgenbaum MA, Toms SA, Staugaitis SM, Prayson RA, Peereboom DM, Stevens GH, Cohen BH, Suh JH (2005) Epidermal growth factor receptor amplification does not have prognostic significance in patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys 63 (3): 695–703
Rich JN (2007) Cancer stem celles in radiation resistance. Cancer Res 67 (19): 8980–8984
Sasaki H, Betenski RA, Cairncross JG, Luis DN (2002) DMBT1 polymorphisms: relationship to malignant glioma tumorigenesis. Cancer Res 62: 1790–1796
Rich JN, Hans C, Jones B, Iversen ES, McLendon RE, Rasheed BK, Dobra A, Dressman HK, Bigner DD, Nevins JR, West M (2005) Gene expression profiling and genetic markers in glioblastoma survival. Cancer Res 65 (10): 4051–4058
Sathornsumetee S, Reardon DA, Desjardins A, Quinn JA, Vredenburgh JJ, Rich JN (2007) Molecular targeted therapy for malignant glioma. Cancer 110 (1): 13–24
Shervington A, Patel R, Lu C, Cruickshanks N, Lea R, Roberts G, Dawson T, Shervington L (2007) Telomerase subunits expression variation between biopsy samples and cell lines derived from malignant glioma. Brain Res 134: 45–52
Shih AH, Holland EC (2006) Platelet-derived growth factor (PDGF) and glial tumorigenesis. Cancer Letters 232: 139–147
Shinojima N, Tada K, Shiraishi S, Kamiryo T, Kochi M, Nakamura H, makino K, Saya H, Hirano H, Kuratsu J, Oka K, Ishimaru Y, Ushio Y (2003) Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res 63 (20): 6962–6970
Stark AM, Nabavi A, Mehdorn HM, Blömer U (2005) Glioblastoma multiforme – report of 267 cases treated at a single institution. Surg Neurol 63: 162–169
Stewart LA (2002) Chemotherapy in adult high-grade glioma: a systematic review and metaanalysis of individual patient data from 12 randomised trials. Lancet 359 (9311): 1011–1018
Stupp R, Hegi ME (2007) Methylguanine methyltransferase testing in glioblastoma: when and how? J Clin Oncol 25 (12): 1459–1460
Stupp R, Mason WP, Van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinial Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352 (10): 987–996
Tchirkov A, Rolhion C, Kemeny JL, Irthum B, Puget S, Khalil T, Chinot O, Kwiatkowski F, Perissel B, Vago P, Verrelle P (2003) Clinical implications of quantitative real-time RT-PCR analysis of hTERT gene expression in human gliomas. Br J Cancer 88 (4): 516–520
Varela M, Ranuncolo SM, Morand A, Lastiri J, De Kier Joffe EB, Puricelli LI, Pallotta MG (2004) EGF-R and PDGF-R, but not bcl-2, overexpression predict overall survival in patients with low-grade astrocytomas. J Surg Oncol 86: 34–40
Wager M, Guilhot J, Blanc JL, Ferrand S, Milin S, Bataille B, Lapierre F, Denis S, Chantereau T, Larsen CJ, Karayan-Tapon L (2006) Prognostic value of increase in transcript levels of Tp73 DeltaEx2-3 isoforms in low-grade glioma patients. Br J Cancer 95 (8): 1062–1069
Watanabe T, Katayama Y, Komine C, Yoschino A, Ogino A, Ohta T, Fukushima T (2005) O6-methylguanine-DNA methyltransferase methylation and Tp53 mutation in malignant astrocytomas and their relationships with clinical course. Int J Cancer 113 (4): 581–587
Watanabe T, Katayama Y, Yoshino A, Komine C, Yokoyama T (2003) Deregulation of the TP53/p14ARF tumor suppressor pathway in low-grade diffuse astrocytomas and its influence on clinical course. Clin Canc Res 9: 4884–4890
Watanabe T, Katayama Y, Yoshino A, Yachi K, Ohta T, Ogino A, Fukushima T (2007) Aberrant hypermethylation of p14ARF and O6-methylguanine-DNA methyltransferase genes in astroytoma progression. Brain Pathol 17 (1): 5–10
Wooten EC, Fults D, Duggirala R, Williams K, Kyritsis AP, Bondy MI, Levin VA, O’Connell P (1999) A study of loss of heterozygosity at 70 loci in anaplastic astrocytoma and glioblastoma multiforme with implications for tumor evolution. Neuro-Oncology 1 (3): 169–176
Zhou XP, Li YJ, Hoang-Xuan K, Laurent-Puig P, Mokhtari K, Longy M (1999) Mutational analysis of the PTEN gene in gliomas : molecular and pathological correlation. Int J Cancer 84: 150–154
Acknowledgements
This work was supported by grants from PHRC (Projet Hospitalier de Recherche Clinique) 2001. Supported by national grant: PHRC (Projet Hospitalier de Recherche Clinique) 2001. This work was presented in part at the annual meeting of the Societe de Neurochirurgie de Langue Française. November 2006. This work is original and has not been published or presented elsewhere.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Wager, M., Menei, P., Guilhot, J. et al. Prognostic molecular markers with no impact on decision-making: the paradox of gliomas based on a prospective study. Br J Cancer 98, 1830–1838 (2008). https://doi.org/10.1038/sj.bjc.6604378
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604378
Keywords
This article is cited by
-
The interaction between TERT promoter mutation and MGMT promoter methylation on overall survival of glioma patients: a meta-analysis
BMC Cancer (2020)
-
An Updated and Comprehensive Meta-Analysis of Association Between Seven Hot Loci Polymorphisms from Eight GWAS and Glioma Risk
Molecular Neurobiology (2016)
-
The TERT rs2736100 Polymorphism and Cancer Risk: A Meta-analysis Based on 25 Case-Control Studies
BMC Cancer (2012)