Abstract
The tumour suppressor gene RASSF1A is known to be frequently silenced by promoter hypermethylation in neuroblastoma tumours. Here we explored the possible prognostic significance of aberrant promoter hypermethylation of RASSF1A in serum DNA samples of patients with neuroblastoma as a surrogate marker for circulating tumour cells. We analysed the methylation status of the RASSF1A gene in matched tumour and pretreatment serum DNA obtained from 68 neuroblastoma patients. Hypermethylation of RASSF1A in tumour samples was found in 64 patients (94%). In contrast, serum methylation of RASSF1A was observed in 17 patients (25%). Serum methylation of RASSF1A was found to be statistically associated with age ⩾12 months at diagnosis (P=0.002), stage 4 (P<0.001) and MYCN amplification (P<0.001). The influence of serum RASSF1A methylation on prognosis was found to be comparable with that of the currently most reliable marker, MYCN amplification on univariate analysis (hazard ratio, 9.2; 95% confidence interval (CI), 2.8–30.1; P<0.001). In multivariate analysis of survival, methylation of RASSF1A in serum had a hazard ratio of 2.4 (95% CI, 0.6–9.2), although this association did not reach statistical significance (P=0.194). These findings show that the methylation status of RASSF1A in the serum of patients with neuroblastoma has the potential to become a prognostic predictor of outcome.
Similar content being viewed by others
Main
Neuroblastoma is the most common extracranial solid tumour in children and is characterised by a wide range of clinical behaviours, from spontaneous regression to rapid progression with a fatal outcome (Maris et al, 2007). The clinical outcome is associated with disease stage, age at diagnosis, MYCN amplification and histological classification. Although numerous genetic abnormalities, including MYCN amplification, are associated with tumour progression and poor outcome, the molecular mechanisms responsible for the pathogenesis of aggressive neuroblastoma remain unclear. Identifying such molecular changes may contribute to improved clinical management and outcome prediction of newly diagnosed neuroblastomas.
In recent years, changes in the status of DNA methylation, known as epigenetic alterations, have turned out to be one of the most common molecular alterations in human neoplasia including neuroblastoma (Misawa et al, 2005; Sugino et al, 2007). Several potential tumour-suppressor genes have been described as frequently silenced by hypermethylation in neuroblastomas. Methylation of promoter CpG islands is known to inhibit transcriptional initiation and cause permanent silencing of downstream genes. Loss of heterozygosity of chromosome 3p21.3 is one of the most frequent alterations in solid tumours. Located within this 3p21.3 locus, the RAS-association domain family 1, isoform A gene (RASSF1A) encodes a RAS effector that has been identified as a tumour suppressor of many different cancer types (Dammann et al, 2000). RASSF1A falls into the category of genes frequently inactivated by methylation rather than mutational events. This gene is silenced and inactivated by promoter region hypermethylation in many adult and childhood cancers, including neuroblastoma (Astuti et al, 2001; Harada et al, 2002; Wong et al, 2004; Yang et al, 2004; Banelli et al, 2005; Lazcoz et al, 2006; Michalowski et al, 2008). RASSF1A has been shown to play important roles in cell cycle regulation, apoptosis and microtubule stability as a tumour suppressor gene (Agathanggelou et al, 2005).
It is well known that DNA fragments are frequently and abundantly found in the serum of cancer patients, with significantly higher levels in patients with metastasis (Hesson et al, 2007). A number of studies have evaluated the potential of circulating tumour-related methylated DNA in serum for the molecular diagnosis and prognosis of various types of cancer (Müller et al, 2003; Ibanez de Caceres et al, 2004; Mori et al, 2005). Methylation-specific PCR assay is a sensitive and specific assay for tumour-related DNA methylation in serum. Several studies have investigated the prospect of using DNA methylation as a surrogate marker for circulating tumour cells in serum samples from breast cancer or melanoma patients (Fiegl et al, 2005; Koyanagi et al, 2006). However, no studies of neuroblastoma have assayed serum samples for aberrant DNA methylation. Therefore, this study investigated whether it is possible to detect RASSF1A epigenetic alterations in the serum of neuroblastoma patients, and aberrant RASSF1A methylation in patient pretherapeutic serum is of prognostic significance in neuroblastoma using a series of matched neuroblastoma tumour and serum DNA.
Materials and methods
Patients and sample collection
Clinical data were collected retrospectively by reviewing the medical database at the Hospital of Kyoto Prefectural University of Medicine for the period between 1985 and 2004. After approval by the Institutional Review Board, 68 neuroblastoma patients were identified on the basis of histological examination of tumour specimens that met the following criteria: the patient had an available tumour specimen; a serum specimen was available; and the patient either died or had >1 year of follow-up time. The clinical data included information regarding tumour stage, age at diagnosis, sex, MYCN gene status and outcome. Staging was evaluated according to the criteria of the International Neuroblastoma Staging System (Maris et al, 2007). Patients of any age who had stage 1 or 2 disease and those younger than 12 months with stage 3 or 4S disease were given either surgery or surgery with chemotherapy (Matsumura and Michon, 2000). Patients aged 12 months or older with stage 3 and any patients with stage 4 disease were treated according to the protocol by the Japanese Neuroblastoma Study Group (Sawaguchi et al, 1990; Tsuchida and Kaneko, 2000; Kaneko et al, 2002; Suita et al, 2007). The patients with stage 4 disease underwent high-dose chemotherapy with autologous stem-cell rescue after the initial chemotherapy. Instead of pre-specified sample size determination, power analysis was conducted after collecting clinical data to guarantee statistical power and to evaluate whether RASSF1A methylation is a prognostic marker for survival. In a realistic scenario, a study of 68 patients had power of 96% to detect a single marker with hazard ratio larger than 5.
Tumour samples at the time of diagnosis and before the administration of chemotherapy were frozen immediately and stored at −80°C until DNA extraction. In addition, match-paired serum samples were assessed. Peripheral blood was obtained before any therapy or surgery. To avoid contamination of serum DNA by the DNA from WBCs, serum was prepared exclusively from the liquid fraction of clotted blood after centrifugation at 1000 × g for 10 min and stored it at −20°C until DNA extraction. For the extraction of free DNA, we used 200 μl of stored serum, which supplemented with 1 μg salmon testes DNA (Sigma, St Louis, MO, USA) as a carrier DNA. DNA was extracted from tumour samples using a QIAmp DNA Mini Kit and from serum samples using a QIAmp DNA Blood Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions.
Analysis of DNA methylation
Treatment of tumour DNA and serum DNA with sodium bisulphite was performed with an EZ DNA methylation kit (Zymo Research, Orange, CA, USA) following the protocol of the manufacturer. Methylation-specific PCR was performed with primers specific for either methylated or unmethylated DNA spanning the region within the RASSF1A gene (Figure 1). The primers used were methylation-specific RAM-1 (5′-GTGTTAACGCGTTGCGTATC-3′) and RAM-2 (5′-AACCCCGCGAACTAAAAACGA-3′) and unmethylation-specific RAU-1 (5′-TTTGGTTGGAGTGTGTTAATG-3′) and RAU-2 (5′-CAAACCCCACAAACTAAAAACAA-3′), as described earlier (Lo et al, 2001). PCR conditions consisted of an initial incubation for 10 min at 95°C followed by 35 cycles for tumour samples or 40 cycles for serum samples of denaturation at 95°C for 45 s, annealing at 60°C for 45 s and extension at 72°C for 60 s, followed by a final extension step of 72°C for 10 min. Lymphocyte DNA and in vitro methylated (using SssI CpG methylase; New England Biolabs, Beverly, MA, USA) lymphocyte DNA were used as unmethylated and methylated controls, respectively. The PCR products obtained were analysed by electrophoresis in 2% agarose gels and stained with ethidium bromide. Samples were scored as methylation positive when methylated alleles were visualised as bands in the methylated DNA lane and as methylation negative when bands were seen only in the unmethylated DNA lane. The analysis of the samples in this study was performed by an analyst blinded to the clinical and biological information.
Statistical analysis
The primary end point was overall survival defined by the period from diagnosis of the primary tumour to any cause of death. The relationship between clinicopathological variables and methylation status of the RASSF1A gene was shown initially using contingency tables and χ2 test. Survival curves for RASSF1A methylation were derived by the Kaplan–Meier method. Univariate analysis was conducted using Cox’s proportional hazard models and log-rank test. Performance of RASSF1A methylation as a prognostic marker was also analysed after adjustment for known prognostic factors by (i) subset analysis of stage 3 patients using contingency tables and Fisher’s exact test and (ii) multivariate Cox’s proportional hazard models including age, sex and tumour stage. Two-sided P-values<0.05 were considered as significant. SAS 9.13 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
Results
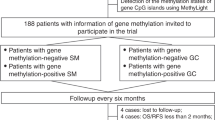
A total of 124 patients with histologically confirmed neuroblastoma or ganglioneuroblastoma were treated at the Hospital of Kyoto Prefectural University of Medicine between January 1985 and May 2004. Sixty-eight patients met the criteria of this retrospective study. The detailed patient disposition is shown in Figure 2 and the baseline characteristics of patients are presented in Table 1. Of the 68 patients, 24 were classified as stage 1, 11 as stage 2, 11 as stage 3, 18 as stage 4 and 4 as stage 4S. At the time of diagnosis, 42 patients (62%) were younger than 12 months, and 26 (38%) were older. We found no significant differences between included and excluded patients for age or stage statistically. Twelve patients (18%) had tumours with MYCN amplification, and MYCN amplification was not detected in the tumours from 56 (82%) patients by southern blot analysis or fluorescence in situ hybridisation. The median follow-up time was 72 months, with a range from 9 to 248 months.
Detection of RASSF1A promoter methylation in tumours
This study initially investigated the hypermethylation status of the RASSF1A tumour suppressor genes in 68 neuroblastoma tumours. Only four (one each at stage 1, 2, 4S and 3) tumours showed no methylation of RASSF1A (Supplementary Table). All other neuroblastoma tumours (64 of 68; 94%) showed methylated RASSF1A. Hypermethylation in tumours was observed very frequently in all of the stages of neuroblastoma examined, including stage 1, 2 and 4S tumours (Supplementary Table) and no correlation between RASSF1A methylation and known prognostic factors including stage, age and MYCN amplification was detected. No relationship between RASSF1A methylation in tumours and outcome was also observed. RASSF1A methylation was not observed in any of the three benign ganglioneuromas.
Detection of RASSF1A promoter methylation in serum
The hypermethylation status of RASSF1A in the matched serum DNA samples was then determined and compared with the pattern of hypermethylation found in the corresponding tumour DNA samples (Figure 3). RASSF1A hypermethylation was detected in 17 of 68 (25%) matched serum DNA samples (Table 1). The detailed overview is shown in Supplementary Table.
RASSF1A methylation status of tumour and serum DNA in neuroblastoma patients. M, methylated; U, unmethylated. The sizes of the PCR products for methylated and unmethylated primers are 93 and 105 bp, respectively. (A) Cases stage 1 and 2 with good prognosis tumour DNAs are methylated but absent in the serum DNAs. (B) In contrast, in stage 3 and 4 MYCN-amplified cases, methylated DNAs are detected in both tumour and serum samples.
Correlation of serum RASSF1A methylation status with clinical factors
The methylation status of RASSF1A in the pretherapeutic serum of the 68 patients was analysed for association with known prognostic factors (Table 2). Serum RASSF1A methylation showed a significant statistical association with age ⩾12 months (P=0.002). RASSF1A methylation in serum was detected more frequently in disseminated stage 4 tumours than local-regional (stage 1, 2 and 3) and 4S tumours (P<0.001). Furthermore, serum-methylated RASSF1A was significantly correlated with MYCN amplification (P<0.001). Notably, all cases with MYCN amplification showed RASSF1A methylation of serum DNA (Supplementary Table).
Analysis of prognostic significance of RASSF1A methylation in serum
The association of pretherapeutic serum methylation status of RASSF1A with clinical outcome was analysed in 68 patients with known follow-ups. Univariate analyses revealed prognostic significance for age at diagnosis ⩾12 months, stage 4 and MYCN amplification (P=0.002, P<0.001 and P<0.001, respectively; Table 3) in this cohort, as expected. Patients with serum-methylated RASSF1A had significantly worse overall survival than patients with serum-unmethylated RASSF1A (P<0.001, log-rank test; Figure 4A). The 5-year survival was more than 90% in patients without serum methylation of RASSF1A, whereas lower than 50% in patients with serum methylation of RASSF1A (hazard ratio, 9.2; 95% confidence interval (95% CI), 2.8–30.1; P<0.001); Table 3). RASSF1A methylation in serum and the known prognostic factors were also correlated with relapse-free survival as well as with overall survival (P<0.001; Table 4; Figure 4B). Furthermore, a subset analysis revealed that stage 3 patients also had a trend towards poorer prognosis when RASSF1A was methylated in serum. When limited to cases in stage 3, two of the three patients with serum-methylated RASSF1A died, whereas all eight patients with serum-unmethylated RASSF1A are alive (P=0.055, Fisher's exact test). In a multivariate analysis including age, sex and tumour stage, serum RASSF1A methylation was still associated with poor outcome with a hazard ratio of 2.4 (95% CI, 0.6–9.2), although this did not reach statistical significance (P=0.194; Table 5).
Kaplan–Meier survival curves of 68 neuroblastoma patients: correlation of pretherapeutic serum RASSF1A methylation status with overall survival (A) and relapse-free survival (B). M, methylated: patients with serum methylation of RASSF1A. U, unmethylated: patients without serum methylation of RASSF1A. The 5-year overall survival was more than 90% in patients without methylation, whereas lower than 50% in patients with methylation (P<0.001).
Discussion
In patients with malignancies, aberrant methylation of serum DNA has been reported (Müller et al, 2003; Ibanez de Caceres et al, 2004; Fiegl et al, 2005; Mori et al, 2005; Koyanagi et al, 2006). We have detected cell-free tumour DNA in serum of neuroblastoma patients (Gotoh et al, 2005). Prognosis in stage 4 neuroblastoma patients with metastases is poor despite intensive chemotherapy (Maris et al, 2007). Therefore, this study aimed to explore the possible prognostic significance of aberrant promoter hypermethylation of RASSF1A, which has been found frequently in neuroblastoma tumours, using pretherapeutic serum of neuroblastoma patients as a surrogate marker for circulating tumour cells.
We first investigated the RASSF1A methylation status in 68 neuroblastoma tumour DNA samples in comparison with matched serum DNA samples. The methylation of RASSF1A was observed in this study in 94% of primary tumours. Our results show that promoter hypermethylation of RASSF1A occurs at a high frequency in primary neuroblastoma tumours and no correlation between RASSF1A methylation and known prognostic factors including stage, age and MYCN amplification, or outcome was seen. The high proportion of RASSF1A promoter methylation in tumours agrees with earlier reports in the literature, which have found RASSF1A to be hypermethylated in 52–94% of tumour DNA samples (Astuti et al, 2001; Harada et al, 2002; Wong et al, 2004; Yang et al, 2004, 2007; Banelli et al, 2005; Lazcoz et al, 2006; Michalowski et al, 2008). Several earlier studies with one exception (Yang et al, 2004) failed to find a statistical correlation between RASSF1A methylation in tumours and poor outcome (Astuti et al, 2001; Harada et al, 2002; Banelli et al, 2005; Michalowski et al, 2008). We also did not observe any relationship between RASSF1A methylation in tumours and prognosis. RASSF1A hypermethylation in tumours can be a relatively early event in neuroblastoma tumorigenesis as it is detectable in non-advanced early-stage tumours with high frequency. Although the prognostic significance of epigenetic changes of single genes in neuroblastoma tumour DNA remain controversial, a few studies have indicated that poor prognosis is associated with the CpG island methylator phenotype (Abe et al, 2005; Banelli et al, 2005; Yang et al, 2007), suggesting that aberrant methylation of multiple genes is likely to contribute to neuroblastoma pathogenesis.
As a next step, we analysed RASSF1A methylation status in 68 paired serum DNA samples. In contrast to tumours, RASSF1A methylation was detected in neuroblastoma patient serum from only 25% (17 out of 68). To investigate the clinical significance of the serum RASSF1A methylation, associations with established prognostic factors and outcome were evaluated. RASSF1A methylation in serum was found to be statistically associated with established prognostic factors. Serum RASSF1A methylation was more frequently detected in neuroblastoma patients with age ⩾12 months at diagnosis (P=0.002), stage 4 (P<0.001) and MYCN amplification (P<0.001). Furthermore, the presence of methylation of RASSF1A in serum was associated with poorer outcome. The influence of serum RASSF1A methylation on prognosis was found to be comparable with that of the currently most reliable marker, MYCN amplification in univariate analysis. A subset analysis of stage 3 patients showed a trend associating poor survival with serum RASSF1A methylation (P=0.055), although the data were limited due to the small number of patients in the subgroup. In multivariate analysis of survival, methylation of RASSF1A in serum had a hazard ratio of 2.42, but this association did not reach statistical significance (P=0.194). Further validation studies using a larger set of patients are necessary to confirm our findings.
The presence of tumour-derived DNA within the blood stream has been identified earlier (Müller et al, 2003; Fiegl et al, 2005; Mori et al, 2005). Recently, one study showed that the detection of circulating tumour cells was correlated with tumour-related methylated DNA in patients with melanoma (Koyanagi et al, 2006), suggesting that circulating tumour cells are a potential source of circulating methylated DNA. Our study suggests that methylated RASSF1A DNA in serum is a surrogate marker for circulating neuroblastoma cells. Another recently published study showed that RASSF1A methylation was also detectable in ovarian cancer patient’s serum at a high frequency from methylated tumour cases including several stage I tumours (Ibanez de Caceres et al, 2004). In the earlier study, there was no statistical association between tumour stage and positive detection in serum. However, some other studies have shown limited detection of RASSF1A methylation in the serum of patients with other neoplasms (Murray et al, 2004; Hesson et al, 2007). These differing results may suggest that free neoplastic DNA from ovarian cancer can access the blood stream more readily than that from other neoplasms including neuroblastoma.
In conclusion, this is the first study to examine epigenetic changes in a tumour suppressor gene, RASSF1A, the promoter of which is hypermethylated at a high frequency in neuroblastoma tumours, using serum DNA in a cohort of neuroblastoma patients. This study demonstrates the utility of detecting circulating methylated RASSF1A, which can be measured in serum, as a potentially predictive marker of neuroblastoma outcome. RASSF1A methylation in serum could have useful clinical applications in neuroblastoma management, if our results are confirmed in larger studies. However, we should not forget the limitation when attempting to translate our findings into the clinical fields as highly sensitive methylation analysis could be tricky because of incomplete bisulphite conversion by inexperienced analysts.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abe M, Ohira M, Kaneda A, Yagi Y, Yamamoto S, Kitano Y, Takato T, Nakagawara A, Ushijima T (2005) CpG island methylator phenotype is a strong determinant of poor prognosis in neuroblastomas. Cancer Res 65: 828–834
Agathanggelou A, Cooper WN, Latif F (2005) Role of the Ras-association domain family 1 tumor suppressor gene in human cancers. Cancer Res 65: 3497–3508
Astuti D, Agathanggelou A, Honorio S, Dallol A, Martinsson T, Kogner P, Cummins C, Neumann HP, Voutilainen R, Dahia P, Eng C, Maher ER, Latif F (2001) RASSF1A promoter region CpG island hypermethylation in phaeochromocytomas and neuroblastoma tumours. Oncogene 20: 7573–7577
Banelli B, Gelvi I, Di Vinci A, Scaruffi P, Casciano I, Allemanni G, Bonassi S, Tonini GP, Romani M (2005) Distinct CpG methylation profiles characterize different clinical groups of neuroblastic tumors. Oncogene 24: 5619–5628
Dammann R, Li C, Yoon JH, Chin PL, Bates S, Pfeifer GP (2000) Epigenetic inactivation of a RAS association domain family protein from the lung tumour suppressor locus 3p21.3. Nat Genet 25: 315–319
Fiegl H, Millinger S, Mueller-Holzner E, Marth C, Ensinger C, Berger A, Klocker H, Goebel G, Widschwendter M (2005) Circulating tumor-specific DNA: a marker for monitoring efficacy of adjuvant therapy in cancer patients. Cancer Res 65: 1141–1145
Gotoh T, Hosoi H, Iehara T, Kuwahara Y, Osone S, Tsuchiya K, Ohira M, Nakagawara A, Kuroda H, Sugimoto T (2005) Prediction of MYCN amplification in neuroblastoma using serum DNA and real-time quantitative polymerase chain reaction. J Clin Oncol 23: 5205–5210
Harada K, Toyooka S, Maitra A, Maruyama R, Toyooka KO, Timmons CF, Tomlinson GE, Mastrangelo D, Hay RJ, Minna JD, Gazdar AF (2002) Aberrant promoter methylation and silencing of the RASSF1A gene in pediatric tumors and cell lines. Oncogene 21: 4345–4349
Hesson LB, Cooper WN, Latif F (2007) The role of RASSF1A methylation in cancer. Dis Markers 23: 73–87
Ibanez de Caceres I, Battagli C, Esteller M, Herman JG, Dulaimi E, Edelson MI, Bergman C, Ehya H, Eisenberg BL, Cairns P (2004) Tumor cell-specific BRCA1 and RASSF1A hypermethylation in serum, plasma, and peritoneal fluid from ovarian cancer patients. Cancer Res 64: 6476–6481
Kaneko M, Tsuchida Y, Mugishima H, Ohnuma N, Yamamoto K, Kawa K, Iwafuchi M, Sawada T, Suita S (2002) Intensified chemotherapy increases the survival rates in patients with stage 4 neuroblastoma with MYCN amplification. J Pediatr Hematol Oncol 24: 613–621
Koyanagi K, Mori T, O’Day SJ, Martinez SR, Wang HJ, Hoon DS (2006) Association of circulating tumor cells with serum tumor-related methylated DNA in peripheral blood of melanoma patients. Cancer Res 66: 6111–6117
Lazcoz P, Munoz J, Nistal M, Pestana A, Encio I, Castresana JS (2006) Frequent promoter hypermethylation of RASSF1A and CASP8 in neuroblastoma. BMC Cancer 6: 254
Lo KW, Kwong J, Hui AB, Chan SY, To KF, Chan AS, Chow LS, Teo PM, Johnson PJ, Huang DP (2001) High frequency of promoter hypermethylation of RASSF1A in nasopharyngeal carcinoma. Cancer Res 61: 3877–3881
Maris JM, Hogarty MD, Bagatell R, Cohn SL (2007) Neuroblastoma. Lancet 369: 2106–2120
Matsumura T, Michon J (2000) Treatment of localized neuroblastoma. In Neuroblastoma, Brodeur GM (ed) pp 403–415. Elsevier Science B. V.: Amsterdam
Michalowski MB, de Fraipont F, Plantaz D, Michelland S, Combaret V, Favrot MC (2008) Methylation of tumor-suppressor genes in neuroblastoma: the RASSF1A gene is almost always methylated in primary tumors. Pediatr Blood Cancer 50: 29–32
Misawa A, Inoue J, Sugino Y, Hosoi H, Sugimoto T, Hosoda F, Ohki M, Imoto I, Inazawa J (2005) Methylation-associated silencing of the nuclear receptor 1I2 gene in advanced-type neuroblastomas, identified by bacterial artificial chromosome array-based methylated CpG island amplification. Cancer Res 65: 10233–10242
Mori T, O’Day SJ, Umetani N, Martinez SR, Kitago M, Koyanagi K, Kuo C, Takeshima TL, Milford R, Wang HJ, Vu VD, Nguyen SL, Hoon DS (2005) Predictive utility of circulating methylated DNA in serum of melanoma patients receiving biochemotherapy. J Clin Oncol 23: 9351–9358
Müller HM, Widschwendter A, Fiegl H, Ivarsson L, Goebel G, Perkmann E, Marth C, Widschwendter M (2003) DNA methylation in serum of breast cancer patients: an independent prognostic marker. Cancer Res 63: 7641–7645
Murray PG, Qiu GH, Fu L, Waites ER, Srivastava G, Heys D, Agathanggelou A, Latif F, Grundy RG, Mann JR, Starczynski J, Crocker J, Parkes SE, Ambinder RF, Young LS, Tao Q (2004) Frequent epigenetic inactivation of the RASSF1A tumor suppressor gene in Hodgkin’s lymphoma. Oncogene 23: 1326–1331
Sawaguchi S, Kaneko M, Uchino J, Takeda T, Iwafuchi M, Matsuyama S, Takahashi H, Nakajo T, Hoshi Y, Okabe I, Yokoyama J, Nishihira H, Sasaki S, Sakurai M, Sawada T, Nagahara N, Tsuchida Y (1990) Treatment of advanced neuroblastoma with emphasis on intensive induction chemotherapy. A report from the Study Group of Japan. Cancer 66: 1879–1887
Sugino Y, Misawa A, Inoue J, Kitagawa M, Hosoi H, Sugimoto T, Imoto I, Inazawa J (2007) Epigenetic silencing of prostaglandin E receptor 2 (PTGER2) is associated with progression of neuroblastomas. Oncogene 26: 7401–7413
Suita S, Tajiri T, Kaneko M, Hirai M, Mugishima H, Sugimoto T, Tsuchida Y (2007) Implications of MYCN amplification in patients with stage 4 neuroblastoma who undergo intensive chemotherapy. J Pediatr Surg 42: 489–493
Tsuchida Y, Kaneko M (2000) Treatment of advanced neuroblastoma: the Japanese experience. In Neuroblastoma, Brodeur GM (ed) pp 453–469. Elsevier Science B. V.: Amsterdam
Wong IH, Chan J, Wong J, Tam PK (2004) Ubiquitous aberrant RASSF1A promoter methylation in childhood neoplasia. Clin Cancer Res 10: 994–1002
Yang Q, Kiernan CM, Tian Y, Salwen HR, Chlenski A, Brumback BA, London WB, Cohn SL (2007) Methylation of CASP8, DCR2, and HIN-1 in neuroblastoma is associated with poor outcome. Clin Cancer Res 13: 3191–3197
Yang Q, Zage P, Kagan D, Tian Y, Seshadri R, Salwen HR, Liu S, Chlenski A, Cohn SL (2004) Association of epigenetic inactivation of RASSF1A with poor outcome in human neuroblastoma. Clin Cancer Res 10: 8493–8500
Acknowledgements
This study was supported by Grant-in-Aid for Young Scientists B 18790713 from the Ministry of Education, Science, Sports and Culture of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Misawa, A., Tanaka, S., Yagyu, S. et al. RASSF1A hypermethylation in pretreatment serum DNA of neuroblastoma patients: a prognostic marker. Br J Cancer 100, 399–404 (2009). https://doi.org/10.1038/sj.bjc.6604887
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604887
Keywords
This article is cited by
-
Progress toward liquid biopsies in pediatric solid tumors
Cancer and Metastasis Reviews (2019)
-
Aberrant Methylation of RASSF1A Closely Associated with HNSCC, a Meta-Analysis
Scientific Reports (2016)
-
Quantitative global and gene-specific promoter methylation in relation to biological properties of neuroblastomas
BMC Medical Genetics (2012)
-
The RASSF gene family members RASSF5, RASSF6 and RASSF7 show frequent DNA methylation in neuroblastoma
Molecular Cancer (2012)
-
Genome-wide promoter methylation analysis in neuroblastoma identifies prognostic methylation biomarkers
Genome Biology (2012)