Abstract
Background:
Studies evaluating vitamin D status in relation to pancreatic cancer risk have yielded inconsistent results.
Methods:
We prospectively followed 118 597 participants in the Nurses' Health Study and Health Professionals Follow-up Study from 1986 to 2006. We calculated a 25-hydroxyvitamin D (25(OH)D) score from known predictors of vitamin D status for each individual and then examined the predicted 25(OH)D levels in relation to pancreatic cancer risk. Relative risks (RRs) and 95% confidence intervals (95% CIs) were estimated using Cox proportional hazards models adjusted for age, sex, race, height, smoking, and diabetes. We then further adjusted for body mass index (BMI) and physical activity in a sensitivity analysis.
Results:
During 20 years of follow-up, we identified 575 incident pancreatic cancer cases. Higher 25(OH)D score was associated with a significant reduction in pancreatic cancer risk; compared with the lowest quintile, participants in the highest quintile of 25(OH)D score had an adjusted RR of 0.65 (95% CI=0.50–0.86; Ptrend=0.001). Results were similar when we further adjusted for BMI and physical activity.
Conclusions:
Higher 25(OH)D score was associated with a lower risk of pancreatic cancer in these two prospective cohort studies.
Similar content being viewed by others
Main
The role of vitamin D in carcinogenesis has attracted increasing attention in recent years. Certain observational studies have reported a protective association between sufficient vitamin D status and lower risk of colon, breast, prostate, and ovarian cancers (Garland et al, 2006). Experimental studies showed that vitamin D has anticancer properties, including inducing differentiation, initiating apoptosis, and inhibiting proliferation, angiogenesis, and metastasis (Giovannucci, 2005). Pancreatic cancer cells express vitamin D receptors (VDRs) (Colston et al, 1997) and high levels of 25(OH)D3-1α-hydroxylase, an enzyme that converts 25(OH)D to the active metabolite, 1,25-dihydroxyvitamin D (1,25(OH)2D) (Schwartz et al, 2004). In addition, 1,25 vitamin D analogs inhibit pancreatic cancer cell line growth in vitro (Colston et al, 1997; Schwartz et al, 2004) and pancreatic tumour growth in vivo (Colston et al, 1997). Therefore, vitamin D may have a role in the development of pancreatic cancer.
However, studies evaluating vitamin D status in relation to pancreatic cancer risk have yielded inconsistent results. To evaluate the impact of vitamin D status in a larger population, we developed a model to predict long-term plasma 25(OH)D levels. This 25(OH)D score takes into account the combined influence of many of the major determinants of vitamin D status. In previous analyses, the score was correlated with plasma 25(OH)D levels and was inversely associated with total cancer mortality and pancreatic cancer incidence in men (follow-up up to 2000; number of pancreatic cancer cases=170) (Giovannucci et al, 2006). In this study, we assessed the relation between predicted long-term vitamin D status and pancreatic cancer risk in both men and women and with additional follow-up (up to 2006), and further examined the potential effect modifications by other factors, using data collected from the Nurses' Health Study (NHS) and the Health Professionals Follow-up Study (HPFS).
Materials and methods
In 1976, the NHS cohort was established when 121 700 US female registered nurses aged 30–55 years answered a baseline questionnaire on risk factors for cancer and cardiovascular disease. Every 2 years, participants receive follow-up questionnaires to update information on potential risk factors and new cancer and disease diagnoses. Dietary information was first collected in 1980 through a food frequency questionnaire, and is updated in alternate follow-up cycles; leisure-time physical activity was assessed in the 1986 questionnaire. Blood samples were provided by 32 826 participants aged 43–70 years from 1989 to 1990.
In 1986, the HPFS cohort was established when 51 529 male dentists, optometrists, osteopaths, podiatrists, pharmacists, and veterinarians aged 40–75 years responded to a baseline questionnaire on risk factors for cancer, cardiovascular disease, and diabetes. A follow-up questionnaire is sent to participants every 2 years requesting an update on nondietary exposures and medical history, with dietary history updated every 4 years. Blood samples were provided by 18 018 participants from 1993 to 1995.
The overall follow-up rate was over 90% in both cohorts. For the present analysis, we excluded individuals with a history of cancer up to 1986, leaving a cohort of 118 597 participants eligible (45 226 men and 73 371 women). This study was approved by the human subjects committee at Brigham and Women's Hospital and the Harvard School of Public Health. All participants provided informed consent for questionnaire and blood data to be used in research studies.
In both cohorts, when a participant (or next of kin for decedents) reported a diagnosis of pancreatic cancer on a follow-up questionnaire, we asked permission to obtain the participant's medical records. We also searched the National Death Index to identify deaths among non-respondents. If the primary cause of death on the death certificate was a previously unreported pancreatic cancer case, we contacted a family member to obtain permission to retrieve medical records. Study physicians at the NHS and HPFS who were masked to the exposure data reviewed medical records and assigned cancer diagnoses and causes of death. In this study, 90% of the pancreatic cancer cases were confirmed by medical record review.
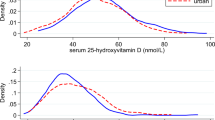
Derivation of the 25(OH)D prediction score has been described previously (Giovannucci et al, 2006). Briefly, we used a sample of 1095 men in the HPFS who had available plasma 25(OH)D measurements and who were free of diagnosed cancer at the time of blood draw. With the measured plasma 25(OH)D concentration as the dependent variable, linear regression was performed using race, geographic region, vitamin D intake, body mass index (BMI), and leisure-time physical activity as independent predictors of plasma 25(OH)D. Then, on the basis of the predictors' regression coefficients from the sample, a 25(OH)D score was calculated for each cohort member. To validate this model, we calculated the 25(OH)D score for an independent sample of 542 men in the HPFS who also had available measurements of circulating 25(OH)D (Giovannucci et al, 2006). The actual plasma concentration rose across increasing deciles of 25(OH)D score (Ptrend <0.001), and the difference in the mean actual 25(OH)D concentration between extreme deciles was 10 ng ml−1, similar to the difference of 11 ng ml−1, which we calculated from the initial dataset (1 ng ml−1=2.496 nmol l−1). In addition, in a separate analysis of 47 800 men, 25(OH)D score had a significantly inverse association with colorectal cancer, which is compatible with plasma-based studies (Giovannucci et al, 2006). We then applied this method to women and calculated 25(OH)D score for all the participants in our study cohort using baseline race and geographic region, and values of leisure-time physical activity, BMI, and vitamin D intake reported in the 1986 questionnaire (when leisure-time physical activity was first assessed).
We collected information on height, race, and geographic regions from the 1986 HPFS questionnaire and the 1976 NHS questionnaire, the only questionnaires in which these variables were assessed. BMI (kg m−2) was calculated using height (reported in 1986 for HPFS and in 1976 for NHS) and weight was reported in the 1986 questionnaires for both cohorts. Information on cigarette smoking, physical activity, history of diabetes, multivitamin use, and dietary factors was also obtained from the 1986 questionnaires for both cohorts.
Statistical analyses
We computed person-time from the return date of the 1986 questionnaire to the date of pancreatic cancer diagnosis, death from any cause, or the end of follow-up (30 June 2006 in the NHS, and 31 January 2006 in the HPFS), whichever came first. Relative risks (RRs) and 95% confidence intervals (CIs) were estimated by Cox proportional hazards models with age (in years) as the primary time scale. The proportional hazards assumption was verified by modelling interaction terms of age and our main exposures as well as other fixed covariates. We first analysed the HPFS and the NHS separately; and if similar RRs were obtained, we would then perform a pooled analysis with adjustment for cohort. 25-Hydroxyvitamin D score was analysed in quintiles based on predicted levels, with the lowest quintile as the reference group. Quintiles were based on the distribution observed in the entire study population. In multivariate models, we adjusted for sex, race (Caucasian, African American, other), height (inches in quintiles), cigarette smoking (never, past, current <15 cigarettes per day, current 15–35 cigarettes per day, current >35 cigarettes per day), and diabetes (yes/no). We considered the possibility that the 25(OH)D score might be acting as a surrogate for other risk factors of pancreatic cancer, such as BMI or physical activity, which were both in the prediction equation. We therefore further adjusted for BMI (kg m−2 in quintiles) and physical activity (MET-h per week in quintiles) in the multivariate model. An indicator variable for missing values of each covariate was created. Linear trends were tested by the Wald test of a score variable that contained median values of 25(OH)D quintiles.
We performed subgroup analyses to examine whether the association of 25(OH)D score with pancreatic cancer varies across strata of sex (also across strata of study, as HPFS consisted of only men and NHS of only women), age at baseline (<60 or ⩾60 years), follow-up duration (<10 or ⩾10 years), geographic region (northern or southern), smoking (never or ever), BMI (<25 or ⩾25 kg m−2), physical activity (below or above median, 8.7 MET-h per week), dietary vitamin D intake (below or above median, 288 IU per day), calcium intake (below or above median, 888 mg per day), multivitamin use (no or yes), and use of supplemental vitamin D (no or yes). We also examined whether retinol intake (below or above median, 2669 IU per day) modified the association between 25(OH)D score and pancreatic cancer because retinol can compete with vitamin D for binding to the retinoid X receptor (Giovannucci, 2005). Tests for interaction were performed by the Wald test using cross-product term of predicted 25(OH)D quintile trend with the stratification variables.
In sensitivity analyses, we excluded the first 2 years of follow-up for all participants to rule out an effect of subclinical pancreatic cancer on 25(OH)D levels. We also did a subgroup analysis including only Caucasians. For analyses among men or women, we repeated our analyses using sex-specific quintiles, which yielded consistent results with those based on quintiles generated from the entire population. Excluding cases with missing medical records (10% of all cases) had no impact on the estimates. All analyses used SAS software, version 9.1 (SAS Institute, Cary, NC, USA).
Results
With 2 226 169 person-years accrued over 20 years of follow-up, a total of 575 pancreatic cancer cases were identified (273 men and 302 women). The median predicted 25(OH)D level was 29.2 ng ml−1 in men and 27.6 ng ml−1 in women. Participants with higher 25(OH)D score were more likely to be Caucasian, live in southern states, have a lower BMI, report higher physical activity, have higher vitamin D intake, and were less likely to be current smokers or have a history of diabetes (Table 1).
We pooled the HPFS and the NHS together because their designs were similar and no significant differences in the risk estimates were found when the two studies were analysed separately (Table 3, the stratified analysis by sex). Higher 25(OH)D score was associated with a significant reduction in risk (Table 2). Compared with individuals with 25(OH)D scores in the lowest quintile, those in the highest quintile had an adjusted RR of 0.65 (95% CI=0.50–0.86; Ptrend=0.001) for pancreatic cancer. This result remained largely unchanged after further adjusting for BMI and physical activity or after excluding the first 2 years of follow-up (Table 2). Restricting to Caucasians had little impact on the estimates (data not shown).
Associations with 25(OH)D score were examined across strata of other factors (Table 3). No statistically significant interactions were found; higher predicted 25(OH)D remained inversely related to risk across most subgroups. We noted that there was a trend towards a greater impact of higher 25(OH)D scores on risk among participants of older age, southern region, nonsmokers, low physical activity, low dietary vitamin D intake, low retinol intake, no multivitamin use, and no supplemental vitamin D use (Table 3).
Discussion
In our study, higher 25(OH)D score was associated with a significantly lower risk of pancreatic cancer. This inverse association was consistent across gender and strata of other covariates. There are several mechanisms through which vitamin D may affect pancreatic cancer risk. Pancreatic cancer cells express VDRs (Colston et al, 1997) and 25(OH)D3-1a-hydroxylase (Schwartz et al, 2004), which metabolises 25(OH)D to the active 1,25(OH)2D vitamin D form. Binding of VDRs by 1,25(OH)2D leads to increased differentiation and apoptosis as well as reduced proliferation, invasiveness, angiogenesis, and metastasis (Giovannucci, 2005); and experimental studies have shown that 1,25(OH)2D analogs inhibit growth of pancreatic cancer cells in vitro and in vivo (Colston et al, 1997; Schwartz et al, 2004). In addition, pancreatic islet cells express VDRs and 25(OH)D3-1a-hydroxylase, and in vitro and in vivo evidence supports that vitamin D deficiency impairs endocrine pancreatic function (Pittas et al, 2007). Observational studies have shown that vitamin D status is inversely associated with development of type 2 diabetes or metabolic syndrome (Mattila et al, 2007; Pittas et al, 2007; Forouhi et al, 2008). As diabetes, hyperglycaemia, and insulin resistance have been linked to pancreatic cancer development, vitamin D may act to decrease pancreatic cancer risk by improving glucose metabolism and reducing insulin resistance.
Epidemiological studies have used four approaches to examine the association of pancreatic cancer with vitamin D status, and their results have been inconsistent. Sunlight exposure, a major source of vitamin D in humans, was inversely correlated with pancreatic cancer in ecological studies conducted in North America, Europe, and Japan (Mizoue, 2004; Boscoe and Schymura, 2006; Grant, 2007). Higher dietary vitamin D intake as well as higher total vitamin D intake (from foods and supplements) was related to lower risk in the NHS and the HPFS (Skinner et al, 2006) but not in a cohort of male Finnish smokers enrolled in the Alpha-Tocopherol, Beta-Carotene (ATBC) Cancer Prevention Study (Stolzenberg-Solomon et al, 2002). Directly measured circulating 25(OH)D, which reflects vitamin D status from both sun and dietary sources, was positively associated with pancreatic cancer risk in male Finnish smokers (fifth vs first quintile, RR=2.92, 95% CI=1.56–5.48) (Stolzenberg-Solomon et al, 2006) but not in a cohort of the Prostate, Lung, Colorectal, and Ovarian (PLCO) Screening Trial (fifth vs first quintile, RR=1.45, 95% CI=0.66–3.15) (Stolzenberg-Solomon et al, 2009). In contrast, the vitamin D prediction score, which also accounts for sun exposure (by using residential state and physical activity as surrogates) and vitamin D intake, was inversely associated with pancreatic cancer risk in the present two US prospective cohort studies (NHS and HPFS) (Giovannucci et al (2006) and this study).
However, participants in the ATBC study might not be comparable with those in the American studies, as they were all current smokers and lived at higher latitude. In this study, we observed a stronger inverse association with vitamin D among nonsmokers and among those living in southern states. The PLCO study also found a significant interaction by geographic region (Pinteraction=0.015): they reported a positive association of risk with plasma vitamin D concentrations among those living in northern latitudes, but no association was observed among those living in southern latitudes (Stolzenberg-Solomon et al, 2009). Another difference in the ATBC study population concerns dietary pattern: a major dietary source of vitamin D in the Finns does not tend to be from fortified dairy products or breakfast cereal as American populations but from vitamin D-rich fish that may contain some pancreatic carcinogen such as organochlorine compounds (Stolzenberg-Solomon et al, 2006). In addition, both the ATBC study and the PLCO study were based on one measurement of 25(OH)D in blood, which most likely reflects recent exposure to sources of vitamin D rather than long-term average vitamin D level; whereas the 25(OH)D prediction score would track well over time because factors that influence the score, such as race and residential region, are immutable or relatively stable. As evidence of this supposition, in a previous study, the correlation between two direct plasma measurements 4 years apart was 0.70, whereas the correlation between the two 25(OH)D scores was 0.83 (Giovannucci et al, 2006).
Retinol has been hypothesised to counteract the cancer prevention effects of vitamin D, possibly acting through competition with vitamin D for the retinoid X receptor (Giovannucci, 2005). In this study, we observed that the inverse association between vitamin D status and pancreatic cancer was more pronounced among those with lower intake of retinol; we also observed a stronger inverse association among those who did not use multivitamins or supplemental vitamin D. We have previously reported an increased pancreatic cancer risk associated with multivitamin use (Skinner et al, 2004), so it is possible that some factor in multivitamin supplements other than vitamin D, potentially retinol, antagonises the protective effect of vitamin D or increases risk independently.
One concern of our approach is that the 25(OH)D score may act as a surrogate for other potential risk factors, such as BMI or physical activity. A higher BMI and less physical activity have previously been associated with increased pancreatic cancer risk in our cohorts (Michaud et al, 2001). However, our results for predicted 25(OH)D did not change when adjusted for BMI or physical activity, which suggests that total vitamin status, rather than simply low BMI or physical activity, is driving the significant inverse association. We are also aware that the prediction score has been developed in men; however, given the prospective design, any misclassification of the 25(OH)D score among women tended to be non-differential, and therefore would only bias the results towards the null. In addition, when we stratified the analyses by gender, similar RRs were obtained for men and women, with no significant interactions. To rule out the possibility that vitamin D status might be changed by preclinical pancreatic cancer at baseline, we excluded the first 2 years of follow-up for all participants in sensitivity analyses. The results were unchanged. Residual confounding by smoking was not likely because a stronger association was observed among never smokers. Residual confounding by other measured factors might be of minor importance in this study, as our age/sex-adjusted models and multivariate models yielded very similar results.
The strengths of our study include its prospective design, use of a validated prediction score taking into account both diet and sun exposure, comprehensive information on many potential confounders, a large sample size that allowed us to stratify the data by potential effect modifiers, and 20 years of follow-up with a high follow-up rate. Because the participants were health professionals, the accuracy of self-reported data is likely to be high; moreover, any misclassification of vitamin D status is likely to be random and would therefore have attenuated rather than exaggerated a true association.
In conclusion, our data suggest that higher 25(OH)D levels may significantly decrease the risk of pancreatic cancer. Given the growing epidemic of vitamin D insufficiency in the US population (Ginde et al, 2009), more epidemiological research is needed, particularly prospective studies with repeated measures of plasma 25(OH)D. If the association between vitamin D and pancreatic cancer is causal, many with low vitamin D levels might benefit from increased vitamin D status for pancreatic cancer risk reduction.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Boscoe FP, Schymura MJ (2006) Solar ultraviolet-B exposure and cancer incidence and mortality in the United States, 1993–2002. BMC Cancer 6: 264
Colston KW, James SY, Ofori-Kuragu EA, Binderup L, Grant AG (1997) Vitamin D receptors and anti-proliferative effects of vitamin D derivatives in human pancreatic carcinoma cells in vivo and in vitro. Br J Cancer 76: 1017–1020
Forouhi NG, Luan J, Cooper A, Boucher BJ, Wareham NJ (2008) Baseline serum 25-hydroxy vitamin d is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely Prospective Study 1990–2000. Diabetes 57: 2619–2625
Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, Holick MF (2006) The role of vitamin D in cancer prevention. Am J Public Health 96: 252–261
Ginde AA, Liu MC, Camargo Jr CA (2009) Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med 169: 626–632
Giovannucci E (2005) The epidemiology of vitamin D and cancer incidence and mortality: a review (United States). Cancer Causes Control 16: 83–95
Giovannucci E, Liu Y, Rimm EB, Hollis BW, Fuchs CS, Stampfer MJ, Willett WC (2006) Prospective study of predictors of vitamin D status and cancer incidence and mortality in men. J Natl Cancer Inst 98: 451–459
Grant WB (2007) An ecologic study of cancer mortality rates in Spain with respect to indices of solar UVB irradiance and smoking. Int J Cancer 120: 1123–1128
Mattila C, Knekt P, Mannisto S, Rissanen H, Laaksonen MA, Montonen J, Reunanen A (2007) Serum 25-hydroxyvitamin D concentration and subsequent risk of type 2 diabetes. Diabetes Care 30: 2569–2570
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Stampfer MJ, Fuchs CS (2001) Physical activity, obesity, height, and the risk of pancreatic cancer. JAMA 286: 921–929
Mizoue T (2004) Ecological study of solar radiation and cancer mortality in Japan. Health Phys 87: 532–538
Pittas AG, Lau J, Hu FB, Dawson-Hughes B (2007) The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab 92: 2017–2029
Schwartz GG, Eads D, Rao A, Cramer SD, Willingham MC, Chen TC, Jamieson DP, Wang L, Burnstein KL, Holick MF, Koumenis C (2004) Pancreatic cancer cells express 25-hydroxyvitamin D-1 alpha-hydroxylase and their proliferation is inhibited by the prohormone 25-hydroxyvitamin D3. Carcinogenesis 25: 1015–1026
Skinner HG, Michaud DS, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2006) Vitamin D intake and the risk for pancreatic cancer in two cohort studies. Cancer Epidemiol Biomarkers Prev 15: 1688–1695
Skinner HG, Michaud DS, Giovannucci EL, Rimm EB, Stampfer MJ, Willett WC, Colditz GA, Fuchs CS (2004) A prospective study of folate intake and the risk of pancreatic cancer in men and women. Am J Epidemiol 160: 248–258
Stolzenberg-Solomon RZ, Hayes RB, Horst RL, Anderson KE, Hollis BW, Silverman DT (2009) Serum vitamin D and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian screening trial. Cancer Res 69: 1439–1447
Stolzenberg-Solomon RZ, Pietinen P, Taylor PR, Virtamo J, Albanes D (2002) Prospective study of diet and pancreatic cancer in male smokers. Am J Epidemiol 155: 783–792
Stolzenberg-Solomon RZ, Vieth R, Azad A, Pietinen P, Taylor PR, Virtamo J, Albanes D (2006) A prospective nested case-control study of vitamin D status and pancreatic cancer risk in male smokers. Cancer Res 66: 10213–10219
Acknowledgements
This study was supported by grants from the National Cancer Institute, National Institutes of Health, Bethesda, MD (Grant Number CA124908) and by the Conquer Cancer Coalition of Massachusetts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bao, Y., Ng, K., Wolpin, B. et al. Predicted vitamin D status and pancreatic cancer risk in two prospective cohort studies. Br J Cancer 102, 1422–1427 (2010). https://doi.org/10.1038/sj.bjc.6605658
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605658
Keywords
This article is cited by
-
The association between circulating 25-hydroxyvitamin D and pancreatic cancer: a systematic review and meta-analysis of observational studies
European Journal of Nutrition (2024)
-
Statin use and pancreatic cancer risk in two prospective cohort studies
Journal of Gastroenterology (2018)
-
Prevalence of Vitamin D Deficiency in Children (6–18 years) Residing in Kullu and Kangra Districts of Himachal Pradesh, India
The Indian Journal of Pediatrics (2018)
-
The inverse association between serum 25-hydroxyvitamin D and mortality may be modified by vitamin A status and use of vitamin A supplements
European Journal of Nutrition (2016)
-
Recipe for cancer education: a novel integrated cooking and nutrition education curriculum for medical students and physicians in dietary preventive and supplemental treatment for pancreatic cancer
Journal of Medicine and the Person (2014)