Abstract
Introduction The clinical diagnosis of dry-eye is confirmed by a suitable test of tear production and the technique commonly used today to diagnose dry eye is the Schirmer’s test (ST). Although the ST is easy to perform it gives variable results, poor reproducibility and low sensitivity for detecting dry eyes. Another test, the tear break up time (TBUT) is used to assess the stability of tears which if abnormal may also cause symptomatic dry-eye. We present the results of both these tests and a new test, which shows greater sensitivity than the ST in detecting aqueous tear deficiency. The fluorescein meniscus time (FMT) is a new test developed in conjunction with one of the authors (CL) and the Department of Ophthalmology at the University Hospital of Wales. The FMT is a measure of the rate at which a fluorescent tear meniscus is formed using 2% sodium fluorescein, a stopwatch and suitable illumination with a slit lamp.
Method An open controlled study in 62 patients and 51 controls was conducted to compare the ability of ST, FMT and TBUT to detect dry-eye in a group of patients diagnosed with rheumatoid arthritis and symptomatic dry eyes for a minimum period of 6 months. A separate control group of 15 subjects was tested on three separate occasions to assess the reproducibility of the FMT test.
Results All three tests showed a statistically significant difference between the patient and control populations; Mann–Whitney P < 0.001. There was a correlation between the right and left eye for all three tests in the control group (ST r2 = 0.77, FMT r2 = 0.98, TBUT r2 = 0.94). This correlation was markedly reduced for FMT and TBUT in the patient population and was in keeping with the symptoms reported as being worse on one side in a proportion of the patients (FMT r2 = 0.52, TBUT r2 = 0.54, ST r2 = 0.75). A correlation with age was also observed for all the three tests in the control group (ST r2 = 0.74, FMT r2= 0.92, TBUT r2 = 0.51), but not in the patient population (ST r2 = 0.06, FMT r2 = 0.18, TBUT r2 = 0.03). A significant correlation was observed between the ST and FMT in both the control (ST vs FMT r2 = 0.65) and patient population (ST vs FMT r2 = 0.44). There was no value greater than 200 seconds for FMT recorded in the control group. Using this value to define an abnormal FMT, 85% of the patients (72% of the eyes tested) had an abnormal result. This was in contrast to 35% of patients (26% of the eyes tested) with abnormal results detected by ST.
Using ANOVA and Student’s paired t-test, there were no significant differences between the three sets of values recorded serially over 3 months to assess the reproducibility of the FMT. The average standard error of the mean was 2.72% and the average co-efficient of variation 4.07%.
Conclusion Our study suggests that the FMT is a more sensitive test with good reproducibility compared to the Schirmer’s test. The FMT correlates with the ST and suggests that both tests measure aqueous tear deficiency. The FMT therefore is a better alternative to ST currently being used to test aqueous tear deficiency.
Similar content being viewed by others
Introduction
The clinical diagnosis of dry eye is usually confirmed by a test of measurement of tear production. The technique commonly used today is Schirmer’s test (ST) developed by the German ophthalmologist, Otto WA Schirmer in 1903.1 Although ST is easy to perform, it gives variable results, poor reproducibility and low sensitivity for detecting dry eyes.2,3,4 Attempts to preserve glandular function are now being made with the use of topical immunosuppressants, and initial results from these studies have been encouraging. With such treatments becoming available a more sensitive and easily performed test would be advantageous to detect and monitor the effect of treatment and the progression of the disease.
Abnormalities of mucin and lipid components in tears may alter the quality of the tear film and result in symptomatic dry-eye even if the quantity of aqueous tear production is normal.5 The TBUT is used to assess the stability of the tear film.6
Colorimetry, using 1% fluorescein and 1% Rose Bengal and the principle of tear dilution, has been used as an alternative method to measure aqueous tear production. The colour intensity of the tear meniscus, 5 min after the introduction of the above combination of dyes, has been shown to correlate with the level of tear production.7
The proposed new FMT test measures the rate of tear meniscus formation. After the introduction of 2% sodium fluorescein drops, tears, which are continually being produced, dilute the fluorescein to form a fluorescent meniscus along the lower eye-lid, beginning at the outer canthus. The rate of production of this meniscus reflects the rate of tear production.
The objective of this study is to compare the ST, FMT and TBUT in detection of dry-eye in a group of patients with rheumatoid arthritis and symptomatic dry eyes with a set of age-matched controls.
Methods
Comparative study
Patient population
Patients (n = 62) with symptomatic dry eyes for a minimum period of 6 months and diagnosed with rheumatoid arthritis were recruited from the Rheumatology clinic at the University Hospital of Wales between June 1997 and June 1999. The symptoms were validated using a standard questionnaire.8 The exclusion criteria were a history of conjunctival, scleral or corneal diseases, diabetes mellitus, thyroid disorders, patients taking antidepressant or diuretic medication and present or past use of contact lenses.
Control group
The control group (n = 51) was recruited from staff at the University Hospital of Wales and patients attending the Optometry clinic for the assessment and management of refractive error. The controls had no symptoms of dry eyes and did not suffer with any other medical or rheumatological disorders. The exclusion criteria for the control group were the same as that for the patient population.
Reproducibility study
A separate group of 15 female subjects with no previous ophthalmic history and taking no medication was used to test the reproducibility of FMT. The exclusion criteria for this group were the same as that for the comparative study patient and control population. The test was performed monthly over 3 months. An average of three measurements was recorded for each eye during each visit.
Ocular assessments
Schirmer’s test (ST)
The test was performed using a standardised kit containing a strip of filter paper 5 mm × 30 mm and placed on to the lower lid margin in a temporal position. The patient looks up and blinks normally for 5 min before the strip is removed and the length of wetted paper measured. A value of < 5 mm was taken as abnormal.1
Fluorescein meniscus time (FMT)
A drop of 2% sodium fluorescein is placed in the lateral canthus of the eye. The natural flow of tears towards the lacrimal duct draws the dye along the lower eye-lid in a medial direction as it is diluted with the tears produced by the lacrimal gland. Using a slit lamp and a cobalt-blue light filter and a stop watch, the time taken for the fluorescent meniscus to fill the lateral half of the lower eyelid was measured in seconds. An average of three measurements was recorded.
Tear break up time test (TBUT)
The stability of the tear film over the conjunctiva and cornea was assessed using a Burton’s lamp with a cobalt blue filter and sodium fluorescein. A drop of 2% sodium fluorescein was applied to the eye, and the patient is asked to blink five times so that a film is formed over the cornea and bulbar conjunctiva. The patient is then asked to refrain from blinking during which time black spots or lines begin to appear indicating dry spots. The interval between the last blink and the first randomly distributed dry spot was taken as the tear break-up time. An average of three measurements was recorded. A value of < 10 seconds is taken as abnormal.6
Procedure
All patients and controls were screened for evidence of any disease affecting the cornea and sclera or anterior blepharitis by an ophthalmologist. The tests were carried out in sequence, FMT followed by TBUT followed by Schirmer’s test. This sequence was chosen to minimise any error caused due to reflex tearing. A set of three readings of FMT and TBUT were taken from each eye in both groups and the average recorded. The Schirmer’s test was then performed in each eye and the results recorded.
Tests for statistical analysis
Correlation was calculated using Pearson’s correlation test. The significance of the results between the patient and control group was calculated using the non-parametric Mann–Whitney U test. The variation of FMT over 3 months was analysed using ANOVA and Student’s paired t-test. The reproducibility of FMT was analysed using standard error of mean and the coefficient of variation (SPSS).
Results
Patient demographics
The mean age of the patient group was 63.8 yrs (range 13–88) and that of the control group was 58.2 yrs (range 40–86). All the patients were rheumatoid factor positive and had erosive disease of mean duration 13.6 yrs (range 4–36 yrs). Using rank analysis there was no significant difference between the two groups for age; Mann–Whitney U P = 0.196. The proportion of females in the patient group was slightly higher than those in the control group (88% vs 72%).
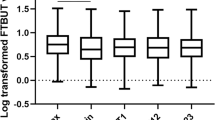
Range of results
The ranges of the results for FMT, ST and TBUT in the control group were 20–200 seconds, 9–20 mm and 10–60 seconds, respectively. The ranges of the results for FMT, ST and TBUT in the patient population were 90–360 seconds, 0–40 mm and 1–13 seconds, respectively (Figure 1).
Correlation with age
A strong correlation with age was noted for all the three tests in the control group. However this correlation was not observed in the patient population (Table 1 and Figure 2).
Comparison of patient and control group: the distribution of the data is as shown in Figure 1. The data were non-parametric in nature therefore rank analysis was used to determine the difference between the two groups. The results of the ST in the patient group showed complete overlap with that in the control. However a better separation between patients and controls was noted with FMT and TBUT. All three tests showed statistically significant differences between the patient and control population; (absolute values: control vs patient population, P < 0.001 for ST, FMT and TBUT).
Comparison of right and left eye
The right and left eyes were tested separately for all the three tests in both the patient and control groups. There was a strong correlation between the right and left eye for all three tests in the control group. This correlation was markedly reduced for FMT and TBUT in the patient population and was in keeping with the symptoms reported as being worse on one side in 17% of the patients. Therefore, each eye was considered separately for further analysis (Table 2 and Figure 3).
Correlation between FMT, Schirmer’s & TBUT
A significant correlation was observed between the ST and FMT in both the control and patient population. There was a poor correlation between TBUT and ST and between TBUT and FMT in the patient and control group (Table 3). There was no value greater than 200 seconds for FMT recorded in the control group. Using this value to define an abnormal FMT, 85% of the patients (72% of the eyes tested) had an abnormal result. This is in contrast to 35% of patients (26% of the eyes tested) with abnormal results detected by ST (Table 4).
Reproducibility of FMT
As seen in the control population of the comparative study, the FMT showed a correlation between the right and left eye (r2 = 0.98) and with age (r2 = 0.87). There were no statistically significant differences between the three sets of values recorded serially over 3 months— P >0.05. The average standard error of the mean for the 15 cases was 2.72%. The average co-efficient of variation was 4.07%.
Discussion
Our study reflects the results of many others showing a poor sensitivity for ST in detecting dry eyes.2,3,4,9 This is due to several factors such as the positioning of the filter paper in the eye, confounding effects of reflex tearing due to the irritation caused by the paper and the influence of evaporation, temperature and humidity.4,10
The correlation co-efficient (r2) of FMT and TBUT in the right and the left eye in the asymptomatic control group was close to 1 compared to that of ST. This correlation between right and left eye was markedly reduced in the patient population for FMT and TBUT and was in keeping with symptoms reported as being worse on one side in 17% of the patients. The Schirmer’s test was unable to detect this difference.
Because FMT measurements increase with increasing age (Figure 2), an age-related normal range would be best suited to define normal limits. However due to the limitation of this study we chose the highest recorded value for FMT in the control population to define normal limits. This cut-off value for ‘normal’ FMT was <200 seconds. The age-related correlation for ST and FMT seen in the control group was not observed in the patient population. Therefore we observed that the pathological process has a more pronounced effect on tear production than the age-related change within the patients (Figure 2). Because of this effect of the disease on tear production and because the numbers studied were small, we have used 100% confidence limits to define abnormal FMT. Though all patients gave a history of symptoms of dry eye for at least a period of 6 months, ST was able to detect an abnormality in only 35%, while the FMT was able to do so in 85%. By using 100% confidence intervals to define normal limits of FMT, the test is made 100% specific, however we may have compromised the sensitivity of the test. No patient with an abnormal ST had a normal FMT, however a large number of patients with normal ST had an abnormal FMT. Hence the FMT would be a more sensitive method for assessing tear production compared to ST (Figure 4).
Premature break-up of the tear film is a feature of any form of dry eye. A reference value of <10 seconds for TBUT is used in the diagnosis of dry eyes.11 The TBUT has been shown to be dependent on the reduction of surface tension by mucins and other surface-active agents but not so much on the quantity of aqueous content in tears.12,13 Using the above value 97% of the patients had an abnormal TBUT (Figure 5). Though this test seems to be most sensitive, it is a clinical measurement of the stability of the tear film rather than of aqueous tear production, and is more appropriately used in conjunction with measurements of aqueous tear deficiency, in the evaluation of symptoms of dry eye. Rose Bengal staining is another commonly used test to evaluate symptomatic dry eye.14 This test quantifies the epithelial damage caused by the lack of tears and is not a true measure of tear production at the time of the test.15 Because of this, the Schirmer test was chosen for comparison with the FMT. Rose Bengal also causes pain on instillation and this pain may outlast by hours or days the duration of topical anaesthesia commonly used.16 This makes the test extremely unpopular among patients. The currently established criterion for the diagnosis of dry eye uses both tests, ie tests for surface damage and tear secretion to evaluate symptoms.17,18
Attempts to limit the destruction of the lacrimal gland and preserve its function are being made with the use of topical androgens and cyclosporin A, and initial studies have given encouraging results.19,20,21 Such a treatment would help both the pathological process and symptoms of dry eye. If new and more effective treatments become available, a test, such as FMT, that is sensitive and easily performed would be needed to detect and monitor the effect of treatment and the progression of the disease.
A number of methods to assess tear secretion accurately have been proposed and this involves a detailed study of the tear meniscus, which accounts for 75–90% of the tear volume.22,23,24 Although more reliable, these tests need more sophisticated equipment and skill to do and would usually be performed in a specialist ophthalmology/research clinic. The Schirmer’s test has been known to be insensitive, but the ease with which the test is performed adds to the popularity of this test. The FMT is similarly easily performed using a slit lamp, stop watch and 2% sodium fluorescein. Although both tests are subjective, our study shows that the FMT is a more sensitive test compared to the Schirmer’s test commonly used today.
The FMT also has good reproducibility with a low standard error of mean (2.72%) and co-efficient of variation (4.07%) in a trained observer. This is in contrast to the Schirmer’s test with a coefficient of variation greater than 10% as reported in previous studies.2 Our study suggests that the FMT is a sensitive test that could replace the Schirmer’s test currently being used to test aqueous deficiency in dry eye.
References
Schirmer O . Studien zur Phisiologie und Pathologie der Tranenabsonderung und Tranenabfuhr. Graefes Arch Klin Exp Ophthalmol 1903; 56: 197–291
Clinch TE, Benedetto DA, Felberg NT, Laibson PR . Schirmer’s test: a closer look. Arch Ophthalmol 1983; 101: 1383–1386
Asbell PA, Chiang B, Li K . Phenol-red thread test compared to Schirmer test in normal subjects. Ophthalmology (Suppl) 1987; 94: 128
Gupta A, Heigle TJ, Pflugfelder SC . Nasolacrimal stimulation of aqueous tear production. (Abstract 3936). Invest Ophthalmol Vis Sci (ARVO Suppl) 1996; 37: S851
Lemp MA, Hamill JR . Factors affecting tear filim breakup in normal eyes. Arch Ophthalmol 1973; 89: 103–105
Norn MS . Desiccation of the precorneal film. I. Corneal wetting time. Acta Ophthalmol 1969; 47: 865–880
Norn MS . Tear secretion in the normal eyes. Estimated by a new method: the lacrimal streak dilution test. Acta Ophthalmol 1965; 43: 567–573
McMonnies CW, Ho A . Patient history in screening for dry eye conditions. J Am Optom Assoc 1987; 58: 296–301
Chiang B, Asbell PA, Franklin B . Phenol-red thread tear test and Schirmer test for tear prodoction in normal and dry eye patients. Invest Ophthalmol Vis Sci (ARVO Suppl) 1988; 29: 337
Tsubota K . The importance of the Schirmer test with nasal stimulation. Am J Ophthalmol 1991; 111: 106–108
Mengher LS, Bron AJ, Tonge SR, Gilbert DJ . A non-invasive instrument for the clinical assessment of the precorneal filim stability. Curr Eye Res 1985; 4: 1–7
Holly FJ, Lemp MA . Wettability and wetting of corneal epithelium. Exp Eye Res 1971; 11: 239–250
Tiffany JM, Pandit JC, Bron AJ . Soluble mucins and the physical properties of tears (Abstract 3901). Invest Ophthalmol Vis Sci (ARVO Suppl) 1996; 37: S845
Van Bijsterveld OP . Diagnostic tests in the sicca syndrome. Arch Ophthalmol 1969; 82: 10–14
Norn MS . Vital staining of cornea and conjuctiva. Acta Ophtalmol Scand 1962; 40: 389–401
Bron J . The Doyne lecture: reflection on the tears. Eye 1997; 11: 583–602
Vitali C, Bombardieri S, Moutsopoulos HM, Balestrieri G, Bencivelli W, Bernstein RM et al. Preliminary criteria for the classification of Sjogrens syndrome: results of a prospective cocerted action supported by the European Community. Arthritis Rheum 1993; 36: 340–347
Shimazaki J . Definition and criteria of dry eye. Report of the Dry Eye Research/Diagnostic Standards Committee. Ophthalmology (Japan) 1995; 37: 765–770
Foulks GN, Plugfelder SC, Lemp MA, Stern KL, Burk CT, Reis BL . A randomised double-masked clinical trial to assess the efficacy and safety of 1% cyclosporin A containing ophthalmic ointment vs placebo in patients with keratoconjuctivitis sicca (abstract). Invest Ophthalmol Vis Sci (ARVO Suppl) 1996; 37: S646
Mircheff AK, Warren DW, Wood RL . Hormonal support of lacrimal function, primary lacrimal deficiency, autoimmunity and peripheral tolerance in the lacrimal gland. Occular Immunol Inflamm 1996; 4: 1–28
Helms HA, Rapozoa P, Stern KL, Burk CT, Rosenthal A, Reis BL . A randomised double-masked clinical trial to assess the safety and comparative efficacy of three concentrations of a cyclosporin-containing ophthalmic ointment vs placebo in patients with keratoconjuctivitis sicca (abstract). Invest Ophthalmol Vis Sci (ARVO Suppl) 1996; 37: S646
Port MJA, Asaria TS . Assessment of human tear volume. J Br Contact Lens Assoc 1990; 13: 76–82
Holly FJ . Dry eye and the Sjogren’s syndrome. Scand J Rheumatol Suppl 1986; 61: 201–205
Bron AJ, Tiffany JM, Yokoi N, Banerjee G, Brown NAP . Meniscometry: a new method to measure tear meniscus curvature (Abstract). Invest Ophthalmol Vis Sci (ARVO Suppl) 1997; 38: 5151
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kallarackal, G., Ansari, E., Amos, N. et al. A comparative study to assess the clinical use of Fluorescein Meniscus Time (FMT) with Tear Break up Time (TBUT) and Schirmer’s tests (ST) in the diagnosis of dry eyes. Eye 16, 594–600 (2002). https://doi.org/10.1038/sj.eye.6700177
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700177
Keywords
This article is cited by
-
Rear 4-min Schirmer test, a modified indicator of Schirmer test in diagnosing dry eye
Scientific Reports (2022)
-
Reliability and efficacy of maximum fluorescein tear break-up time in diagnosing dry eye disease
Scientific Reports (2021)
-
Ocular surface disease in psoriatic patients in a developing country
International Ophthalmology (2021)
-
Ocular surface and tear film status among contact lens wearers and non-wearers who use VDT at work: comparing three different lens types
International Archives of Occupational and Environmental Health (2018)
-
Sodium Hyaluronate in the Treatment of Dry Eye Syndrome: A Systematic Review and Meta-Analysis
Scientific Reports (2017)