Abstract
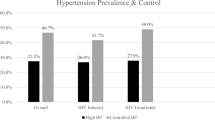
The objective of this study was to determine the prevalence, treatment, and control of hypertension, and the determinants of undertreatment in the Dutch population. The study design was cross-sectional. A population-based survey on cardiovascular disease risk factors in the Netherlands from 1996 to 2002 was the setting of the study. A total of 10 820 men and women, aged 30–59 years, were included in the study. The main outcome measures of the study were: Prevalence of hypertension, treatment, and control of hypertension and determinants of undertreatment of hypertension. Hypertension was defined as: systolic blood pressure (SBP) ⩾140 mmHg and/or diastolic blood pressure (DBP) ⩾90 mmHg, and/or the use of antihypertensive medication. Treated and controlled hypertension was defined as SBP <140 mmHg and DBP <90 mmHg. Multivariate logistic regression was used to assess the determinants of undertreatment. The prevalence of hypertension in men was 21.4% and in women 14.9%, and 17.9% of the hypertensive men and 38.5% of the hypertensive women were receiving antihypertensive medication. Of the untreated hypertensives, 21.9% of the men and 13.6% of the women were eligible for treatment with antihypertensive medication according to Dutch guidelines. Female gender and the use of cholesterol-lowering medication were associated with an increased chance of being treated. Subjects who were physically active, on a low salt diet, and current smokers had an increased chance of being untreated. Taking cholesterol-lowering medication and no asthma or allergy were factors associated with better control of blood pressure. In conclusion, a considerable proportion of hypertensives were untreated and uncontrolled. Therefore, the detection and control of hypertension in the Netherlands needs to improve. Several groups of hypertensives were identified that need additional care and attention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Brown MJ, Haydock S . Pathoaetiology, epidemiology and diagnosis of hypertension. Drugs 2000; 59 (Suppl 2): 1–12.
Svardsudd K, Tibblin G . Mortality and morbidity during 13.5 years’ follow-up in relation to blood pressure. The study of men born in 1913. Acta Med Scand 1979; 205: 483–492.
Fiebach NH et al. A prospective study of high blood pressure and cardiovascular disease in women. Am J Epidemiol 1989; 130: 646–654.
MacMahon S et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990; 335: 765–774.
van der Giezen AM et al. Systolic blood pressure and cardiovascular mortality among 13 740 Dutch women. Prev Med 1990; 19: 456–465.
Kannel WB . Cardioprotection and antihypertensive therapy: the key importance of addressing the associated coronary risk factors (the Framingham experience). Am J Cardiol 1996; 77: 6B–11B.
Collins R, MacMahon S . Blood pressure, antihyper-tensive drug treatment and the risks of stroke and of coronary heart disease. Br Med Bull 1994; 50: 272–298.
Gueyffier F, Froment A, Gouton M . New meta-analysis of treatment trials of hypertension: improving the estimate of therapeutic benefit. J Hum Hypertens 1996; 10: 1–8.
Neal B, MacMahon S, Chapman N . Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. Lancet 2000; 356: 1955–1964.
Klungel OH et al. Undertreatment of hypertension in a population-based study in The Netherlands. J Hypertens 1998; 16: 1371–1378.
World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens 1999; 17: 151–183.
Verschuren WMM et al. Cardiovascular disease risk factors in The Netherlands. Neth J Cardiol 1993; 4: 205–210.
Jacobsen BK, Thelle DS . Risk factors for coronary heart disease and level of education. The Tromso Heart Study. Am J Epidemiol 1988; 127: 923–932.
Kraus JF, Borhani NO, Franti CE . Socioeconomic status, ethnicity, and risk of coronary heart disease. Am J Epidemiol 1980; 111: 407–414.
CBO-consensus. Hoge bloeddruk. Herziening richtlijnen 2000 (in Dutch).
Klungel OH et al. Estimating the prevalence of hypertension corrected for the effect of within-person variability in blood pressure. J Clin Epidemiol 2000; 53: 1158–1163.
Primatesta P, Brookes M, Poulter NR . Improved hypertension management and control: results from the health survey for England 1998. Hypertension 2001; 38: 827–832.
de Gaudemaris R et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension 2002; 39: 1119–1125.
Gasse C et al. Assessing hypertension management in the community: trends of prevalence, detection, treatment, and control of hypertension in the MONICA Project, Augsburg 1984–1995. J Hum Hypertens 2001; 15: 27–36.
Wolf-Maier K et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. Jama 2003; 289: 2363–2369.
De Henauw S et al. Trends in the prevalence, detection, treatment and control of arterial hypertension in the Belgian adult population. J Hypertens 1998; 16: 277–284.
Di Bari M et al. Undertreatment of hypertension in community-dwelling older adults: a drug-utilization study in Dicomano, Italy. J Hypertens 1999; 17: 1633–1640.
Shah S, Cook DG . Inequalities in the treatment and control of hypertension: age, social isolation and lifestyle are more important than economic circumstances. J Hypertens 2001; 19: 1333–1340.
NHG-Standaard Hypertensie. Huisarts Wet 1997; 40: 598–617 (in Dutch).
Chobanian AV et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Jama 2003; 289: 2560–2571.
Luscher TF et al. Compliance in hypertension: facts and concepts. J Hypertens Suppl 1985; 3: S3–S9.
Balazovjech I, Hnilica Jr P . Compliance with antihypertensive treatment in consultation rooms for hypertensive patients. J Hum Hypertens 1993; 7: 581–583.
Haynes RB et al. Improvement of medication compliance in uncontrolled hypertension. Lancet 1976; 1: 1265–1268.
Peterson GM, McLean S, Millingen KS . Determinants of patient compliance with anticonvulsant therapy. Epilepsia 1982; 23: 607–613.
Morisky DE et al. Evaluation of family health education to build social support for long-term control of high blood pressure. Health Educ Q 1985; 12: 35–50.
Eisen SA et al. The effect of medication compliance on the control of hypertension. J Gen Intern Med 1987; 2: 298–305.
Stockwell DH et al. The determinants of hypertension awareness, treatment, and control in an insured population. Am J Public Health 1994; 84: 1768–1774.
Wilber JA, Barrow JG . Hypertension—a community problem. Am J Med 1972; 52: 653–663.
Klein LE . Compliance and blood pressure control. Hypertension 1988; 11 (3 Part 2): II61–II64.
Trilling JS, Froom J . The urgent need to improve hypertension care. Arch Fam Med 2000; 9: 794–801.
Miller NH, Hill M, Kottke T, Ockene IS . The multilevel compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation 1997; 95: 1085–1090.
Klungel OH et al. Cardiovascular diseases and risk factors in a population-based study in The Netherlands: agreement between questionnaire information and medical records. Neth J Med 1999; 55: 177–183.
Klungel OH et al. Agreement between self-reported antihypertensive drug use and pharmacy records in a population-based study in The Netherlands. Pharm World Sci 1999; 21: 217–220.
Acknowledgements
The management team for the MORGEN-project consisted of Dr HB Bueno de Mesquita, Dr HA Smit, Dr WMM Verschuren, and Professor Dr JC Seidell. Logistic support was provided by A Jansen and J Steenbrink MSc, and data management was performed by A Blokstra MSc, AWD van Kessel MSc, and PE Steinberger MSc. Project leader for the Doetinchem Cohort Study is Dr WMM Verschuren, with logistic support by J Steenbrink MSc and P Vissink, secretarial assistance by EP van der Wolf, and data management by A Blokstra MSc, AWD van Kessel MSc, and PE Steinberger MSc. We thank the epidemiologists and field workers of the Municipal Health Services in Amsterdam, Doetinchem, and Maastricht for their contribution to the data collection for this study. This study is supported by the Netherlands Heart Foundation, Grant number: 2001.064. This study was financially supported by the Ministry of Health, Welfare and Sport of the Netherlands and the National Institute for Public Health and the Environment. Potential conflicts of interest: none.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schelleman, H., Klungel, O., Kromhout, D. et al. Prevalence and determinants of undertreatment of hypertension in the Netherlands. J Hum Hypertens 18, 317–324 (2004). https://doi.org/10.1038/sj.jhh.1001672
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001672
Keywords
This article is cited by
-
Genetic Variants of the Renin Angiotensin System: Effects on Atherosclerosis in Experimental Models and Humans
Current Atherosclerosis Reports (2010)
-
Hypertension risk in idiopathic hyperCKemia
Journal of Neurology (2008)
-
Ethnic differences in the effect of environmental stressors on blood pressure and hypertension in the Netherlands
BMC Public Health (2007)
-
Interactions between five candidate genes and antihypertensive drug therapy on blood pressure
The Pharmacogenomics Journal (2006)
-
Factors associated with hypertension awareness, treatment and control among ethnic groups in Amsterdam, The Netherlands: The SUNSET study
Journal of Human Hypertension (2006)