Abstract
The pathogenic mechanisms of Alzheimer’s disease (AD) remain largely unknown and clinical trials have not demonstrated significant benefit. Biochemical characterization of AD and its prodromal phase may provide new diagnostic and therapeutic insights. We used targeted metabolomics platform to profile cerebrospinal fluid (CSF) from AD (n=40), mild cognitive impairment (MCI, n=36) and control (n=38) subjects; univariate and multivariate analyses to define between-group differences; and partial least square-discriminant analysis models to classify diagnostic groups using CSF metabolomic profiles. A partial correlation network was built to link metabolic markers, protein markers and disease severity. AD subjects had elevated methionine (MET), 5-hydroxyindoleacetic acid (5-HIAA), vanillylmandelic acid, xanthosine and glutathione versus controls. MCI subjects had elevated 5-HIAA, MET, hypoxanthine and other metabolites versus controls. Metabolite ratios revealed changes within tryptophan, MET and purine pathways. Initial pathway analyses identified steps in several pathways that appear altered in AD and MCI. A partial correlation network showed total tau most directly related to norepinephrine and purine pathways; amyloid-β (Ab42) was related directly to an unidentified metabolite and indirectly to 5-HIAA and MET. These findings indicate that MCI and AD are associated with an overlapping pattern of perturbations in tryptophan, tyrosine, MET and purine pathways, and suggest that profound biochemical alterations are linked to abnormal Ab42 and tau metabolism. Metabolomics provides powerful tools to map interlinked biochemical pathway perturbations and study AD as a disease of network failure.
Similar content being viewed by others
Introduction
Although the causes for late-onset Alzheimer’s disease (AD) are unknown, there are clearly profound biochemical alterations in multiple pathways in the AD brain including changes in amyloid precursor protein metabolism, tau phosphorylation, oxidative stress, energetics and mitochondrial dysfunction, inflammation, membrane lipid dysregulation and neurotransmitter pathway disruption.1, 2 Many of these biochemical changes are functionally interrelated, highlighting the need for a systems approach to model the pathogenesis of AD at a network level.
Until recently, the lack of validated ‘mega’ metabolic platforms has limited the ability to study metabolic networks in relation to known pathologic markers. Such studies could eventually help provide a deeper understanding of disease mechanisms that goes beyond current limited AD hypotheses and targets, and may potentially yield novel candidate biomarkers for diagnosis or risk prediction.
Over the past decade, major advances in analytical chemistry have resulted in a new field, that is, metabolomics, the study of the repertoire of small molecules present in cells, tissues, organs and biological fluids and their mutual interactions.3, 4 Many diseases disrupt metabolism and result in changes that are long-lasting and can be captured as metabolic signatures.4 As metabolic processes are at the core of physiology, metabolomics is ideally positioned to characterize an integrated view of metabolic failures in AD and metabolic failures that can lead to formation of plaques and tangles in the brain. Metabolomic signatures, utilizing different metabolomic platforms, have been reported for several central nervous system disorders, including AD.5, 6, 7, 8, 9 One such platform, the liquid chromatography electrochemical array platform, detects a subset of the metabolome consisting of compounds susceptible to oxidation reduction and is therefore one of the most sensitive platforms for studying key central nervous system pathways, such as the tryptophan, tyrosine and purine pathways. This targeted platform enabled us to define signatures for several central nervous system diseases and drugs used for the treatment of these diseases.7, 10
In this study, we used liquid chromatography electrochemical array to establish metabolomic signatures in cerebrospinal fluid (CSF) from two well-characterized cohorts of AD and mild cognitive impairment (MCI) participants compared with matched cognitively intact normal control (CN) participants. We modeled changes in metabolic pathways and developed multivariate models to classify diagnostic groups using their baseline CSF metabolomic profiles. A partial correlation network was built to link metabolic markers, protein markers and disease severity.
Materials and methods
Study design and participants
This case–control study examined participants enrolled in a prospective longitudinal study. The participants were recruited at the Penn Memory Center, University of Pennsylvania (Philadelphia, PA, USA) and the Maria de los Santos Health Center (Philadelphia, PA, USA), following written informed consent under approval of the University of Pennsylvania ethics committee and Duke University Medical Center institutional review board. Cases were classified as AD or MCI based on standard diagnostic criteria.11, 12 From this cohort, we identified a subset of 114 participants (40 AD, 36 MCI and 38 CN) who had banked CSF samples and other traditional biomarker data. Cases from each diagnostic category were matched as closely as possible for age and gender. Neuropsychological testing was conducted including the Clinical Dementia Rating, Dementia Rating Scale-Second Edition, Mini-Mental State Exam (MMSE) and/or tests of frontal executive function, memory, language, praxis, visuospatial construction, motor performance, mood and function. Details for CSF samples collection and for standardized Lumixex assay for amyloid-β (Ab42), total tau (t-tau) and phosphorylated tau (p-tau) at the threonine 181 are described elsewhere.13 There were no significant differences between AD, MCI and CN groups with regard to age and gender; however, as expected, baseline cognitive status and apolipoprotein E (ApoE) ɛ4 genotype prevalence were significantly different (Table 1).
Metabolomic profiling
Samples were analyzed using a liquid chromatography electrochemical array platform that was extensively used and validated in our prior studies into neurodegenerative and psychiatric disorders.7, 10 Levels of 71 metabolites, including 24 known compounds, were measured (see Table 2 for known compounds and their abbreviations).
Data analysis
Data analysis included univariate and multivariate statistical techniques. The Fisher’s exact test was used to examine the association of the following clinical covariates with disease status: gender, with APOE ɛ4, cholinesterase inhibitors and memantine; Kruskal–Wallis tests were used to test between-diagnostic-group differences in age, years of education and MMSE scores; two-sample t-test was used to compare age of onset between diagnostic groups. The raw metabolomics data were first viewed by quantile–quantile normal and χ2 plots, and by variable-pair scatterplots, to assess normality and nonlinear relationships. As most analytes were not approximately normally distributed, nonparametric Kruskal–Wallis tests were used for pairwise comparison between AD or MCI and CN. Significant metabolites were mapped to several key biochemical pathways. We examined differences among diagnostic groups in product/substrate ratios within the pathways; the ratios of compounds could potentially indicate the relative effectiveness of enzymes involved in the pathways. Correlations between metabolites and protein markers were obtained by calculating their Pearson’s correlation coefficients. The significance of correlation was tested using Student’s t-distribution. For all above systematic univariate tests, multiple comparison was corrected by estimating the positive false discovery rate using Storey’s q-value. The partial correlation network was built among metabolites, protein markers and MMSE using the sparse partial correlation estimation approach.14 An edge between two network variables implies conditional dependency between corresponding variable pairs conditional on the rest of the variables. The false discovery rate was controlled at 0.05 using the approach suggested by Meinshausen and Bühlmann.15 Metabolomic profiles were used to construct partial least square-discriminant analysis (PLS-DA) models for categorical separation of AD or MCI and CN. The variable importance in projection parameter was used to identify metabolites that make the most contribution in discriminating diagnostic groups in the PLS-DA models, and threefold cross-validation of the PLS-DA models was performed to evaluate model predictive performance. Participant data from different groups were randomly divided into training (∼2/3 of all participants in a given group) and test (remaining participants in a given group) sets. Following construction of PLS-DA models using training sets, the models were used to predict class membership of the test-set participants. This procedure was repeated three times with different participants in the training and test sets and a new PLS-DA model constructed each time.
Results
Metabolic differences between AD, MCI and CN groups
Metabolites and key pathways altered in AD
Several metabolites were significantly different in AD patients versus controls (Table 3 and Figure 1). Methionine (MET), involved in one-carbon metabolism and methylation processes; 5-Hydroxyindoleacetic acid (5-HIAA), a major metabolite of serotonin (5-HT); Vanillylmandelic acid (VMA), an end product of catecholamine metabolism; and Xanthosine (XANTH), a purine pathway metabolite, were significantly increased in AD. The 5-HIAA/5-Hydroxytryptophan (5-HTP) ratio was significantly increased in AD, whereas GSH (glutathione)/MET ratio was decreased. There were significant differences in the levels of several compounds of unknown chemical structure between AD and CN (Table 3).
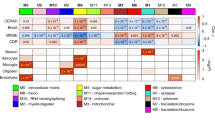
Changes in the methionine (a), tryptophan (b), purine (c) and tyrosine (d) pathways in Alzheimer’s disease (AD). Red metabolites: significantly increased in AD; dark metabolites: not measured. Red and green pathways: significantly up- and downregulated in AD, respectively, implicated by ratios. For expansions of the metabolite abbreviations, see Table 2.
Metabolites and key pathways affected in MCI
Metabolites that increased in MCI included 5-HIAA, MET, hypoxanthine (HX), indole-3-acetic acid (I-3-AA), uric acid (URIC) and kynurenine (KYN) whereas tryptophan (TRP) was decreased (Table 3 and Figure 2). Similar to AD, the 5-HIAA/5-HTP ratio was increased and GSH/MET ratio was decreased in MCI; additionally, the ratios of URIC/XAN (Xanthine), KYN/TRP, I-3-AA/TRP and XAN/XANTH were increased and of 5-HTP/TRP and XAN/HX were decreased. Similar to AD, several compounds of unknown chemical structure were different between MCI and controls (Table 3). Many significant unknown metabolites increased in MCI were those noted in AD.
Changes in the methionine (a), tryptophan (b), purine (c) and tyrosine (d) pathways in mild cognitive impairment (MCI). Red metabolites: significantly increased in MCI; dark metabolites: not measured. Red and green pathways: significantly up- and downregulated in MCI, respectively, implicated by ratios. For expansions of the metabolite abbreviations, see Table 2.
MCI versus AD comparison 5-HTP was lower in MCI compared with AD. Several unknown metabolites differed between MCI and AD (Supplementary Table I).
Metabolite intercorrelations
To gain insights into possible structure/functions of unknown metabolites changed in AD and MCI, we analyzed their possible associations with the known metabolites (Supplementary Table 2). Levels of several unknown metabolites that significantly changed in AD and MCI versus controls correlated with levels of known compounds significantly changed in AD and MCI, suggesting that they could be either structurally or functionally related to the metabolites from one-carbon metabolism and from tyrosine, TRP, and purine pathways.
PLS-DA models for categorical separation of AD, MCI and CN
We evaluated the value of metabolic profiles in separating disease participants and controls. PLS-DA models were constructed for each pair of disease status (AD vs CN and MCI vs CN); the performance of models was evaluated by cross-validation using correct classification rate together with sensitivity and specificity. The correct classification rate for AD versus CN was 83.1% (sensitivity: 76.5% and specificity: 89.2%). The correct classification rate for MCI versus CN was also 83.1% (sensitivity: 73.5% and specificity: 91.9%). Figure 3 shows the classification results using a two-component PLS-DA model, with corresponding variable importance in projection scores provided in Supplementary Table 3.
PLS-DA models for separation between AD, MCI and CN. (a) Separation between AD and CN; (b) separation between MCI and CN. Examples of PLS-DA models cross-validation: (c) AD versus CN and (d) MCI versus CN. A, Alzheimer’s disease; AD, Alzheimer’s disease; C, normal cognition; CN, normal cognition; M, mild cognitive impairment; MCI, mild cognitive impairment; PLS-DA, partial least square-discriminant analysis.
Correlation between metabolites, proteins and MMSE scores
A pair-wise correlation analysis revealed significant associations between metabolites and each of Ab42, t-tau and p-tau (Table 4). We found correlations between MET, VMA and Ab42; between XAN, 4-hydroxyphenyllactic acid (4-HPLA), 5-HIAA, VMA, GSH, (2-hydroxyphenylacetic acid) and t-tau; and between XAN, VMA, 4-HPLA, HVA, GSH, XANTH and p-tau. For correlations within each group, see Table 5. A partial correlation network was built among protein AD biomarkers, MMSE, all known metabolites and seven unknown metabolites found in previous studies to be related to disease status (Figure 4). Two variables are connected within the network if their mutual correlation cannot be fully mediated by the other variables. The false discovery rate was controlled at 0.05. T-tau is directly related to VMA, XAN and 9–29.925, Ab42 is related to 15–65.533, and MMSE is related to 15–65.533 and 12–94.5. Interestingly, the unknown metabolite 15–65.533 is related to MET and 5-HIAA, the two metabolites altered in AD CSF.
A partial correlation network among clinical AD biomarkers and MMSE (red) and known (green) and important unknown (blue) CSF metabolites in all the participants. AD, Alzheimer’s disease; CSF, cerebrospinal fluid; MMSE, Mini-Mental State Exam. For expansions of the metabolite abbreviations, see Table 2.
Discussion
We used a metabolomics approach to identify potential metabolic pathways implicated in the mechanisms of AD and MCI. Different perturbations in one-carbon metabolism, tyrosine, TRP and purine pathways were identified in CSF from AD and MCI patients. These findings complement and expand upon prior reports of alterations in neurotransmitter, purine and cysteine metabolism in AD and MCI, and provide some new insights. We have confirmed that all key metabolites that contribute to separation of groups are not confounded by gender differences.
Earlier studies indicated that blood levels of homocysteine and cysteine were increased in AD patients; it was also shown that increased homocysteine is associated with an increased risk of cognitive impairment and dementia,16 and alterations in the homocysteine metabolism are related to increased accumulation of p-tau and could contribute to the neurofibrillary pathology in normal aging and AD.17 Recently, a significant increase of cysteine in the CSF of AD patients has been reported.8 MET, the key metabolite of one-carbon metabolism, which provides the methyl groups for numerous methyl transferase reactions via S-adenosylmethionine, is the precursor for homocysteine and cysteine, the rate-limiting amino acid in glutathione synthesis. Synthesis of glutathione involves formation of γ-glutamylcysteine from glutamate and cysteine (catalyzed by γ-glutamylcysteine synthetase), followed by the addition of glycine to γ-glutamylcysteine (catalyzed by glutathione synthetase). The role of glutathione depletion in AD and in dementia has been documented.18
In this study, we found for the first time that in both AD and MCI participants, the levels of MET—the precursor of homocysteine—are increased whereas the MET/GSH ratio is decreased. These findings suggest that the glutathione depletion in AD could result from perturbations within this pathway, probably occurring at the level of synthesis of glutathione from cysteine. Supporting this hypothesis are reports that upregulation of glutathione by γ-glutamylcysteine in primary neuronal cultures protects against Ab42-mediated oxidative stress and neurotoxicity,19 and that GSH delivery systems prevent amyloid-induced oxidative stress and cholinergic dysfunction in AD models in vitro.20
AD is associated with dysfunction of catecholaminergic and serotoninergic neurotransmitter systems. Post-mortem studies in AD have found the loss of noradrenergic (NE) neurons in locus coeruleus with corresponding decreases of NE levels in the cortical and subcortical projection areas, and have demonstrated that severity of AD correlated with the degree of NE neuron loss in locus coeruleus.21 Our previous metabolomic study found significant decreases in NE levels in ventricular CSF from autopsy-confirmed AD participants.7 NE was not measured in this study because of its very low levels in lumbar CSF; however, VMA levels (end product of the NE pathway) were found to be significantly increased in AD, as noted in previous ventricular CSF studies.7 The observed increases in VMA levels could be a result of medication, as approximately 15% of the AD participants were treated with the N-Methyl-D-aspartate antagonist, memantine, which was shown to increase the release and metabolism of NE.22 However, we found no differences in VMA levels between AD participants who received memantine and those who did not (data not shown). NE is metabolized by catechol-O-methytransferase (COMT) and monoamine oxidase (MAO) with VMA as the end product. Therefore, it is possible that upregulation of COMT and/or MAO in AD patients could result in the observed increases of VMA in AD. Indeed, activation of MAO in the AD brain was recently demonstrated.23 COMT, in addition to the metabolism of monoamines, is the principal enzyme in the metabolism of estrogens that have recently been implicated in the AD pathogenesis through the ApoE-dependent mechanism.24, 25 The COMT GG genotype and APOE ɛ4 allele have been found to have a synergistic effect upon the risk of AD, and COMT genetic variations could be associated with psychoses in AD.26 Therefore, the elevated levels of VMA in AD found in this study suggest upregulated COMT that, in turn, could result in the increased metabolism of estrogens. In this respect, it is interesting that levels of VMA were the highest among the ɛ4/ɛ4 participants as compared with ɛ3/ɛ4 and non-ApoE participants (data not shown). Further studies with larger cohorts of well-defined ApoE AD participants are necessary to elucidate the potential role of COMT in the mechanisms of AD.
The main metabolite of 5-HT metabolism, 5-HIAA, was increased in both AD and MCI participants. Potential mechanisms could involve upregulation of MAO activity in AD,23 or antidepressant therapy in these patients. No correlation was found between use of medications and levels of 5-HIAA (data not shown). We also observed an increased 5-HIAA/5-HTP ratio in AD and MCI groups, and an increased KYN/TRP ratio in MCI participants. These findings, combined with previous reports, provide further evidence for the involvement of TRP and KYN branch of its metabolism in mechanisms of neurodegeneration and in depression.27
We found increased XAN levels in AD and an increased ratio of URIC/XAN in MCI, which is in accordance with our previous studies in AD.7 Several studies have implicated mitochondrial dysfunction, oxidative stress and related perturbations in purine metabolism in the mechanisms of neurodegenerative disorders, including AD. Additionally, there is growing evidence for the involvement of purinergic transmission in the mechanisms of AD and in Ab42 processing. Post-mortem brain tissue from patients with a confirmed diagnosis of AD showed a loss of A1 adenosine receptors in the hippocampus, and an increased density of A1 and A2 receptors in the frontal cortex.28 In post-mortem neocortical and hippocampal tissue from patients with AD, a colocalization of A1 receptors with Ab42 in senile plaques was reported, and in human neuroblastoma cells, activation of A1 receptors was linked to increased formation of soluble Ab42; it was also found that purinergic receptors are involved in α-secretase-dependent processing of the Ab42.29, 30 In addition, novel purine-based γ-secretase modulators were introduced as selective agents toward Ab42.31
A partial correlation network has revealed new insights about links between protein markers of AD and metabolites. The correlation of t-tau to VMA and XAN suggests that the NE pathway and purine pathway might be implicated in t-tau pathology and that the MET pathway one-carbon metabolism and methylation might link to Ab42 pathology through the unknown compound 15–65.533. A new perspective emerging from recent research is that AD is a network disorder that affects a large number of neuronal cell types, is organized into functionally connected networks across many brain regions and is not simply a disease of discrete lesions limited to specialized brain regions associated with cognition and learning. Within this concept, AD is believed to be a response to a shift from normal to pathological networks, and hence the emerging recognition that we must understand the disease at a systems level. Metabolomics provides powerful tools to enable this systems approach.
In this study we used a targeted metabolomics approach to map biochemical pathways that could be implicated in the mechanisms of AD pathogenesis. CSF samples were analyzed as it is generally believed that CSF more closely reflects metabolic processes in the brain because of the free exchange of several molecules between the brain and CSF. Obviously, blood samples easily available in clinical setting would be more suitable for developing biomarkers for monitoring/predicting progression of the disease. However, the extent to which metabolic changes in blood reflect changes in CSF remains to be investigated and we will establish relationships between changes in central and peripheral compartments in future studies; most likely, for different classes of metabolites the relationships between central and peripheral compartments would be different. In this study, matching plasma and CSF samples from same subjects were not available; currently, we are collecting such samples for our next study. Integration of data obtained using different metabolomics and lipidomics platforms (both targeted and nontargeted) for central and peripheral samples with genetic, imaging and proteomic data for all AD subjects is our ultimate goal and focus of our current investigations. For MCI subjects involved in this study, no sufficient clinical data to enable us to define metabolic signatures of progression from MCI to AD were available. Currently, we are in the process of getting this information and are recruiting more MCI subjects to address this topic in subsequent studies.
The strength of our study is the careful and rigorous selection of participants and prospective nature of our cohort. However, there are limitations to our study. Although our approach was targeted, we did perform a large number of preplanned and exploratory analyses on a relatively small sample. However, within the logistics of obtaining CSF studies in a prospective cohort of AD and MCI patients, ours is one of the largest CSF metabolomics studies in at-risk and AD participants to date. We were unable to replicate some prior findings because of low levels of some metabolites in lumbar CSF compared with ventricular CSF (for example, NE). Yet, our findings complement prior findings in pointing to changes within key pathways; for example, studies have reported changes in cysteine levels in AD,32, 33 which seem related to our observation of alteration in MET and the GSH/MET ratio, although we could not measure cysteine. The same applies for observations with the VMA end product, NE. Previously, in post-mortem ventricular CSF, we measured NE and implicated it in AD pathogensis.7 Its levels were much lower in lumbar CSF (this study), and hence we could not measure it yet. Still, both studies pointed to the same pathway as being affected in AD. Differences in exogenous factors (diet, medications and comorbidities) between study samples might account for some of the variations, and are difficult to control for across studies. We have checked for possible effects of key drugs used in this patient population. We used Fisher's Exact Test to look for statistically significant associations between cognitive outcomes (AD vs MCI vs CN) and use of several medication classes. As expected, there was a statistically significant difference in the use of cholinesterase inhibitors (unadjusted P<0.0001) as well as memantine (unadjusted P=0.003), the two types of drugs commonly used to treat Alzheimer-type dementias, among the diagnostic groups. Use of antidepressants, antipsychotics, anxiolytics, corticosteroids and statins did not differ significantly between the diagnostic groups. Therefore, only the cholinesterase inhibitors and memantine were further examined for correlation with the metabolites. We did note marginal effects of these agents on a few metabolites including MET, MET/GSH ratio, and several unknown metabolites. None of these effects fully accounted for the reported metabolic differences between diagnostic groups. We have also performed analysis on metabolomics data that have been adjusted for drug effects and our reported findings remain highly significant. Our results should be viewed as hypothesis-generating comparisons rather than definitive findings. Therefore, our findings and theoretical speculations should be viewed as exploratory until replicated in larger independent studies.
In summary, our study reveals alterations in several functionally relevant metabolic networks and pathways in AD, with some overlapping changes in MCI. Further study of such findings might yield new insights about the mechanisms that underlie AD and novel targets for development as diagnostic or predictive markers.
References
O'Brien RJ, Wong PC . Amyloid precursor protein processing and Alzheimer’s disease. Annu Rev Neurosci 2011; 34: 185–204.
Di Paolo G, Kim TW . Linking lipids to Alzheimer’s disease: cholesterol and beyond. Nat Rev Neurosci 2011; 12: 284–296.
Patti GJ, Yanes O, Siuzdak G . Innovation: Metabolomics: the apogee of the omics trilogy. Nat Rev Mol Cell Biol 2012; 13: 263–269.
Kaddurah-Daouk R, Krishnan KR . Metabolomics: a global biochemical approach to the study of central nervous system diseases. Neuropsychopharmacology 2009; 34: 173–186.
Sato Y, Suzuki I, Nakamura T, Bernier F, Aoshima K, Oda Y . Identification of a new plasma biomarker of Alzheimer’s disease using metabolomics technology. J Lipid Res 2012; 53: 567–576.
Han X, Rozen S, Boyle SH, Hellegers C, Cheng H, Burke JR et al. Metabolomics in early Alzheimer’s disease: identification of altered plasma sphingolipidome using shotgun lipidomics. PLoS One 2011; 6: e21643.
Kaddurah-Daouk R, Rozen S, Matson W, Han X, Hulette CM, Burke JR et al. Metabolomic changes in autopsy-confirmed Alzheimer’s disease. Alzheimers Dement 2011; 7: 309–317.
Czech C, Berndt P, Busch K, Schmitz O, Wiemer J, Most V et al. Metabolite profiling of Alzheimer’s disease cerebrospinal fluid. PLoS One 2012; 7: 16.
Oresic M, Hyotylainen T, Herukka SK, Sysi-Aho M, Mattila I, Julkunen V et al. Metabolome in progression to Alzheimer’s disease. Transl Psychiatry 2011; 1: e57.
Kaddurah-Daouk R, Boyle S, Matson W, Sharma S, Matson S, Zhu H et al. Pretreatment metabotype as a predictor of response to sertraline or placebo in depressed outpatients: a proof of concept. Transl Psychiatry 2011; 1: e26.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM . Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984; 34: 939–944.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E . Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999; 56: 303–308.
Kang JH, Vanderstichele H, Trojanowski JQ, Shaw LM . Simultaneous analysis of cerebrospinal fluid biomarkers using microsphere-based xMAP multiplex technology for early detection of Alzheimer’s disease. Methods 2012; 56: 484–493.
Peng J, Wang P, Zhou N, Zhu J . Partial correlation estimation by joint sparse regression models. J Am Stat Assoc 2009; 104: 735–746.
Meinshausen N, Bühlmann P . High dimensional graphs and variable selection with the Lasso. Ann Statist 2006; 34: 1436–1462.
Vogel T, Dali-Youcef N, Kaltenbach G, Andres E . Homocysteine, vitamin B12, folate and cognitive functions: a systematic and critical review of the literature. Int J Clin Pract 2009; 63: 1061–1067.
Popp J, Lewczuk P, Linnebank M, Cvetanovska G, Smulders Y, Kölsch H et al. Homocysteine metabolism and cerebrospinal fluid markers for Alzheimer’s disease. J Alzheimers Dis 2009; 18: 819–828.
Ballatori N, Krance SM, Notenboom S, Shi S, Tieu K, Hammond CL . Glutathione dysregulation and the etiology and progression of human diseases. Biol Chem 2009; 390: 191–214.
Boyd-Kimball D, Sultana R, Abdul HM, Butterfield DA . Gamma-glutamylcysteine ethyl ester-induced up-regulation of glutathione protects neurons against Abeta(1-42)-mediated oxidative stress and neurotoxicity: implications for Alzheimer’s disease. J Neurosci Res 2002; 79: 700–706.
Zampagni M, Wright D, Cascella R, D'Adamio G, Casamenti F, Evangelisti E et al. Novel S-acyl glutathione derivatives prevent amyloid oxidative stress and cholinergic dysfunction in Alzheimer disease models. Free Radic Biol Med 2012; 52: 1362–1371.
Bondareff W, Mountjoy CQ, Roth M . Loss of neurons of origin of the adrenergic projection to cerebral cortex (nucleus locus ceruleus) in senile dementia. Neurology 1982; 32: 164–168.
Shearman E, Rossi S, Szasz B, Juranyi Z, Fallon S, Pomara N et al. Changes in cerebral neurotransmitters and metabolites induced by acute donepezil and memantine administrations: a microdialysis study. Brain Res Bull 2006; 69: 204–213.
Gulyas B, Pavlova E, Kasa P, Gulya K, Bakota L, Várszegi S et al. Activated MAO-B in the brain of Alzheimer patients, demonstrated by [11C]-L-deprenyl using whole hemisphere autoradiography. Neurochem Int 2011; 58: 60–68.
Wang PN, Liu HC, Liu TY, Chu A, Hong CJ, Lin KN et al. Estrogen-metabolizing gene COMT polymorphism synergistic APOE epsilon4 allele increases the risk of Alzheimer disease. Dement Geriatr Cogn Disord 2005; 19: 120–125.
Martinez MF, Martin XE, Alcelay LG, Flores JC, Valiente JM, Juanbeltz BI et al. The COMT Val158 Met polymorphism as an associated risk factor for Alzheimer disease and mild cognitive impairment in APOE 4 carriers. BMC Neurosci 2009; 10: 125–130.
Borroni B, Grassi M, Costanzi C, Zanetti M, Archetti S, Franzoni S et al. Haplotypes in cathechol-O-methyltransferase gene confer increased risk for psychosis in Alzheimer disease. Neurobiol Aging 2007; 28: 1231–1238.
Kincses ZT, Toldi J, Vecsei L . Kynurenines, neurodegeneration and Alzheimer’s disease. J Cell Mol Med 2010; 14: 2045–2054.
Albasanz JL, Perez S, Barrachina M, Ferrer I, Martin M . Up-regulation of adenosine receptors in the frontal cortex in Alzheimer’s disease. Brain Pathol 2008; 18: 211–219.
Delarasse C, Auger R, Gonnord P, Fontaine B, Kanellopoulos JM . The purinergic receptor P2 × 7 triggers alpha-secretase-dependent processing of the amyloid precursor protein. J Biol Chem 2011; 286: 2596–2606.
Camden JM, Schrader AM, Camden RE, González FA, Erb L, Seye CI et al. P2Y2 nucleotide receptors enhance alpha-secretase-dependent amyloid precursor protein processing. J Biol Chem 2005; 280: 18696–18702.
Rivkin A, Ahearn SP, Chichetti SM, Hamblett CL, Garcia Y, Martinez M et al. Purine derivatives as potent gamma-secretase modulators. Bioorg Med Chem Lett 2010; 20: 2279–2282.
Arlt S, Schwedhelm E, Kolsch H, Jahn H, Linnebank M, Smulders Y et al. Dimethylarginines, homocysteine metabolism, and cerebrospinal fluid markers for Alzheimer’s disease. J Alzheimers Dis 2012; 31: 751–758.
Smach MA, Jacob N, Golmard JL, Charfeddine B, Lammouchi T, Ben Othman L et al. Folate and homocysteine in the cerebrospinal fluid of patients with Alzheimer’s disease or dementia: a case control study. Eur Neurol 2011; 65: 270–278.
Acknowledgements
The corresponding author has full access to all the data in the study and the final responsibility for the decision to submit for publication. This project received funding from the following sources: NIH R01 NS054008 (to RK-D. and MD), R24 GM078233 and RC2 5RC2GM092729 ‘The Pharmacometabolomics Research Network’ (to RK-D), Alzheimer Drug Discovery Foundation, Pfizer and Pennsylvania Alzheimer’s Disease Coordinating Center (NIH P30 AG010124). Recruitment of study participants was funded through the NIH Grant AG09215 to the University of Pennsylvania. Funding sources did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript. We acknowledge the editorial support of Jon Kilner (Pittsburgh, PA, USA).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Drs Kaddurah-Daouk and Matson are inventors on patents in the metabolomics field. Dr Kaddurah-Daouk has received funding from pharmaceutical companies for metabolomic studies. Dr Arnold has received research grant support through the University of Pennsylvania from the NIH, the American Health Assistance Foundation and the Marian S Ware Alzheimer’s Program, as well as several pharmaceutical companies and advisory/speaking honoraria from Universities, pharmaceutical companies and law firms. Dr Trojanowski may accrue revenue in the future on patents submitted by the University of Pennsylvania wherein he is co-inventor and he received revenue from the sale of Avid to Eli Lily as co-inventor on imaging-related patents submitted by the University of Pennsylvania while he receives research support from the NIH, Bristol Myer Squib, AstraZeneca and several non-profits. Dr Doraiswamy has received research grants (through Duke) and advisory/speaking fees from the NIH, the Alzheimer’s Association, the Alzheimer’s Drug Discovery Foundation, the Alzheimer’s Foundation of America, and several pharmaceutical companies; and he owns stock in Sonexa and Clarimedix. Dr Motsinger-Reif has received consulting honoraria from pharmaceutical companies. The remaining co-authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kaddurah-Daouk, R., Zhu, H., Sharma, S. et al. Alterations in metabolic pathways and networks in Alzheimer’s disease. Transl Psychiatry 3, e244 (2013). https://doi.org/10.1038/tp.2013.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.18
Keywords
This article is cited by
-
Investigating metabolic dysregulation in serum of triple transgenic Alzheimer’s disease male mice: implications for pathogenesis and potential biomarkers
Amino Acids (2024)
-
Exploring the aging process of cognitively healthy adults by analyzing cerebrospinal fluid metabolomics using liquid chromatography-tandem mass spectrometry
BMC Geriatrics (2023)
-
Targeted Metabolomic Analysis of the Eye Tissue of Triple Transgenic Alzheimer’s Disease Mice at an Early Pathological Stage
Molecular Neurobiology (2023)
-
Discovery of Molecular Networks of Neuroprotection Conferred by Brahmi Extract in Aβ42-Induced Toxicity Model of Drosophila melanogaster Using a Quantitative Proteomic Approach
Molecular Neurobiology (2023)
-
Microbial-derived metabolites as a risk factor of age-related cognitive decline and dementia
Molecular Neurodegeneration (2022)