Abstract
OBJECTIVE: To evaluate the effect of primary care coordination on utilization rates and satisfaction with care among public hospital patients.
DESIGN: Prospective randomized gatekeeper intervention, with 1-year follow-up.
SETTING: The Adult General Medical Clinic at San Francisco General Hospital, a university-affiliated public hospital.
PATIENTS: We studied 2,293 established patients of 28 primary care physicians.
INTERVENTION: Patients were randomized based on their primary care physician’s main clinic day. The 1,121 patients in the intervention group (Ambulatory Patient-Physician Relationship Organized to Achieve Coordinated Healthcare [APPROACH] group) required primary care physician approval to receive specialty and emergency department (ED) services; 1,172 patients in the control group did not.
MEASUREMENTS AND MAIN RESULTS: Changes in outpatient, ED, and inpatient utilization were measured for APPROACH and control groups over the 1-year observation period, and the differences in the changes between groups were calculated to estimate the effect of the intervention. Acceptability of the gatekeeping model was determined via patient satisfaction surveys.
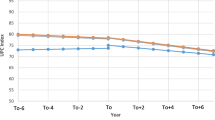
RESULTS: Over the 1-year observation period, APPROACH patients decreased their specialty use by 0.57 visits per year more than control patients did (P=.04; 95% confidence interval [CI] −1.05 to −0.01). While APPROACH patients increased their primary care use by 0.27 visits per year more than control patients, this difference was not statistically significant (P=.14; 95% CI, −0.11 to 0.66). Changes in lowacuity ED care were similar between the two groups (0.06 visits per year more in APPROACH group than control group, P=.42; 95% CI, −0.09 to 0.22). APPROACH patients decreased yearly hospitalizations by 0.14 visits per year more than control patients (P=.02; 95% CI, −0.26 to −0.03). Changes in patient satisfaction with care, perceived access to specialists, and use of out-of-network services between the 2 groups were similar.
CONCLUSIONS: A primary care model of health delivery in a public hospital that utilized a gatekeeping strategy decreased outpatient specialty and hospitalization rates and was acceptable to patients.
Similar content being viewed by others
References
Kreier R. HMOs without gatekeepers. Am Med News. 1996;39(29):1.
Freudenheim M. Medical insurers revise cost-control efforts. New York Times. December 3, 1999:A1.
Grembowski D, Cook K, Patrick D, Roussel A. Managed care and physician referral. Med Care Res Rev. 1998;55:3–31.
Kerr E, Mittman B, Hays R, Siu A, Leake B, Brook R. Managed care and capitation in California: how do physicians at financial risk control their own utilization? Ann Intern Med. 1995;123:500–4.
Felt-Lisk S. How HMOs structure primary care delivery. Managed Care Q. 1996;4:96–105.
Rosenbaum S. A look inside Medicaid managed care. Health Aff. 1997;16:266–71.
Rowland D, Hanson K. Medicaid: moving to managed care. Health Aff. 1996;15:150–2.
Hurley R, Freund D, Gage B. Gatekeeper effects on patterns of physician use. J Fam Pract. 1991;32:167–73.
National Public Health and Hospital Institute. Survey of Managed Care Programs for the Indigent. Washington, DC: National Public Health and Hospital Institute; 1996.
Sisk J, Gorman S, Reisinger A, Glied S, DuMouchel W, Hynes M. Evaluation of Medicaid managed care. JAMA. 1996;276:50–5.
Long S, Settle R. An evaluation of Utah’s primary care case management program for Medicaid recipients. Med Care. 1988;26:1021–32.
Schoenman J, Evans W, Schur C. Primary care case management for Medicaid recipients: evaluation of the Maryland Access to Care program. Inquiry. 1997;34:155–70.
Martin D, Diehr P, Price K, Richardson W. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989;79:1628–32.
Manning W, Leibowitz A, Goldberg G, Rogers W, Newhouse J. A controlled trial of the effect of a prepaid group practice on use of services. N Engl J Med. 1984;310:1505–10.
Rice T. Physician payment policies: impacts and implications. Annu Rev Public Health. 1997:549–65.
Hillman A, Pauly M, Kerstein J. How do financial incentives affect physicians’ clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989;321:86–92.
Stearns S, Wolfe B, Kindig D. Physician response to fee-for-service and capitation payment. Inquiry. 1992;29:416–25.
Hellinger F. The impact of financial incentives on physician behavior in managed care plans: a review of the evidence. Med Care Res Rev. 1996;53:294–314.
SAS/STAT Software: Changes and Enhancements through Release 6.12. Cary, NC: Sas Institute Inc.; 1997:571–701.
Efron B, Tibshirani RJ. An Introduction to the Bootstrap. London, UK: Chapman and Hall; 1993:178–88, 214–8, 398–403.
The Medicaid Access Study Group: access of Medicaid recipients to outpatient care. N Engl J Med. 1994:1426–30.
Weinberger M, Oddone E, Henderson W, et al. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334:1441–7.
Bodenheimer T, Lo B, Casalino L. Primary care physicians should be coordinators, not gatekeepers. JAMA. 1999;281:2045–8.
Blumenthal D, Mort E, Edwards J. The efficacy of primary care for vulnerable population groups. Health Serv Res. 1995;30:253–73.
Conrad D, Maynard C, Cheadle A, et al. Primary care physician compensation methods in medical groups. JAMA. 1998;279:853–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schillinger, D., Bibbins-Domingo, K., Vranizan, K. et al. Effects of primary care coordination on public hospital patients. J GEN INTERN MED 15, 329–336 (2000). https://doi.org/10.1046/j.1525-1497.2000.07010.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2000.07010.x