Abstract
Is school closure effective in mitigating influenza outbreaks? For Singapore, we developed an individual-based simulation model using real-life contact data. We evaluated the impacts of temporal factors – trigger threshold and duration – on the effectiveness of school closure as a mitigation policy. We found an upper bound of the duration of school closure, where further extension beyond which will not bring additional benefits to suppressing the attack rate and peak incidence. For school closure with a relatively short duration (< 6 weeks), it is more effective to start closure after a relatively longer delay from the first day of infection; if the duration of school closure is long (>6 weeks), however, it is better to start it as early as reasonable. Our studies reveal the critical importance of timing in school closure, especially in cost-cautious situations. Our studies also demonstrate the great potential of a properly developed individual-based simulation model in evaluating various disease control policies.
Similar content being viewed by others
Introduction
In 2009, countries planned and implemented many intervention strategies to control an H1N1 influenza pandemic.1, 2, 3, 4 Although the pandemic ended with mild health impacts, it challenged people to think about control strategies for mitigating the spread of an emerging virus capable of causing high morbidity and mortality, especially when pharmaceuticals are not sufficiently available.
Schools may be critical in epidemic control and mitigation planning. High contact rates and long contact durations in schools prompt spread in school populations. School closure, a conventional non-pharmaceutical intervention,5 has been extensively evaluated and even implemented in real-life disease control. However, its effectiveness is still under debate.6, 7, 8, 9 In a recent article, Cauchemez et al 10 reviewed many aspects of school closure, concluding that uncertainties persist about the benefits of school closure as a mitigation method.
The historical data on school closures suggest contradictory conclusions. In March 2008, Hong Kong school officials closed all primary schools for 2 weeks to block a rising wave of seasonal influenza, later reporting no substantial effects.11 On the other hand, Israeli school closure data from 16 January to 28 January 2000 supported that school closure resulted in reduced respiratory infections.12 The two evaluations on school closure were conducted under different social structures, which may have affected effectiveness significantly. In addition to the differences in social structures, we believe different temporal factors, specifically the trigger threshold (when to close schools) and intervention duration (how long to keep schools closed), may have influenced results. Here we test different cases of school closure with different trigger thresholds and durations, including the uncontrolled scenario. Comparing simulation results, we explore the impact of temporal factors on the effectiveness of school closure in mitigating the spread of influenza epidemic.
We constructed an individual-based simulation model founded on real-life social contact data from Singapore, and then evaluated the effectiveness of school closure. The realistic modeling of the social-contact network allows us to reveal complex heterogeneous social structures.13, 14, 15 By representing people (or places) as ‘vertices with contacts’, computer programs can easily simulate the transmission of an infectious disease through individual interactions along the links within the contact network. Such a method, more intuitive than mathematical modeling, helps visualize the spreading dynamics of infectious diseases. It enables detailed evaluations of the effects of temporal factors.
We introduce the construction of the social contact network and define the models of disease spread and intervention policies; report extensive simulation results; followed by discussions and conclusions.
Methods
In this work, we run individual-based simulations on a realistic social contact network model constructed with real-life data from Singapore communities. The contact network represents the statistical properties of interpersonal contacts that can lead to disease transmission. By conducting extensive simulations on the network model, we investigate the effectiveness of school closure with different trigger thresholds and implementation durations.
Contact network construction
A contact network is a network representation of human-to-human contacts in a community. Each person is represented by a vertex in the network, and each contact between people is represented by an edge connecting the pair of vertices. The pathogens transmit from one person (vertex) to another (vertex) only through the connecting edges. The number of edges emanating from a vertex is the degree of the vertex. The distribution of the degrees of vertices, also called degree distribution, is a fundamental quantity in network theory, playing a critical role in estimating the outbreak size and epidemic probability of a network.13
Most social contacts take place in various community structures such as schools, workplaces, and hospitals (Figure 1). Community structures can be represented by clusters of vertices with denser connections internally than outside. The existence of clusters significantly affects the topology of a contact network and transmission of diseases on it.16
Using HPCgen model,17 we constructed a plausible contact network based on Singapore social structure. We set up 100 000 households according to Singapore household size distribution, household structure, and age distribution18 – a population of ∼480 000. According to age, household members were assigned to the schools and workplaces based on school size distribution and company size distribution in Singapore. Individuals were also assigned to visit other community structures such as shopping places and hospitals based on shopper traffic statistics and ward bed occupancy records.
Public transport in Singapore had daily ridership up to 5 000 000 passenger-trips in 2008/2009.19 We assumed that public transport is a giant community structure in which commuters are mixed to make contacts randomly. Within each community structure, we created the random connections between pairs of individuals by assuming a Poisson degree distribution15 with the mean degrees acquired from our surveys on social contacts. Each school and hospital was further divided into sub-units, that is, classes and wards. Each individual in the sub-units was assumed to have a higher probability of contact with someone from the same sub-unit than from the other sub-units. Teachers and health-care workers were also assigned to the classes and wards to describe contact with students or patients. The list of applied data and their sources are tabulated in Table 1.
To our knowledge, there has been no prior study on contact behaviors and the spread of infectious disease in Singapore. To improve estimates of the number of contacts at particular locations, we surveyed the public in Singapore in 2008, collecting 1040 pieces of survey data. The derived average numbers of contacts are summarized in Table 2. The average number of contacts in the households is excluded in the table, as we assumed every household to be fully connected.
Models of disease spreading
Spread of influenza reflects infection and host progression. Infection is the process by which an infectious person infects his/her susceptible contacts; and host progression is the development of infectivity, as the influenza illness progresses in the host (Figure 2). By making contacts with infectious individuals, a susceptible has a chance (transmission probability) to be exposed, that is infected by the influenza virus; then after a latency period, the exposed person becomes infectious but has not yet developed any flu symptoms, termed pre-symptomatic; during the incubation period since exposed, the pre-symptomatic person has a probability (symptomatic rate) to develop the clinical symptoms of influenza and become symptomatic infectious, or stay as asymptomatic infectious without any symptoms; finally at the end of the infectious period, the symptomatic or asymptomatic infectious person is removed, who recovers from influenza or dies.
Intervention policies
School closure can be of three kinds: (1) class closure, for example, a class is closed if there is a diagnosed case; (2) individual school closure, for example, a school is closed if there are diagnosed cases, and (3) all-school closure, that is, all schools are closed simultaneously if a threshold number of cases are diagnosed. All three types of school closure have occurred. Australia, the United Kingdom, the United States, and Japan have used school closure to mitigate the spread of pandemic influenza.13, 14, 15
In our modeling study, we implemented all-school closure in the simulations with varying trigger thresholds and implementation durations. We assumed: (1) all schools are closed immediately once the trigger threshold is reached; (2) all the contacts taking place in schools are removed from the contact network during the period of school closure; and (3) school closure does not cause an increase of contacts in other community structures.
Besides modeling the dynamics of the disease spread, our study focused on investigating the effectiveness of intervention polices in different scenarios. We characterized an intervention policy by two parameters:
-
1
Trigger threshold is the percentage of diagnosed (symptomatic) cases in the overall population, which is used to determine the starting time of intervention. For example, trigger=0.1 per cent means an intervention will be implemented when 0.1 per cent of population is symptomatic.
-
2
Duration refers to for how long an intervention will be in place.
Results
We first simulated the uncontrolled scenario on the constructed contact network, providing baseline results. Then, we simulated all-school closure with different trigger thresholds and durations, to evaluate their impacts on the effectiveness of school closure.
Experiment settings
The basic reproductive number, R 0, is defined as the average number of secondary infections produced by a randomly selected infected person in a fully susceptible population.20 We determine R 0 empirically by assuming a scenario in which only a single randomly selected individual is infected and everyone else is susceptible and not able to transmit, and then count the average number of secondary infections. R 0 is then obtained as the average number of secondary infections in 10 000 realizations. In our simulations, R 0 was estimated to be 1.9 (95 per cent CI, 1.871–1.924) and the mean generation time (T g) to be 2.522 days (95 per cent CI, 2.489–2.508). These are comparable to estimates of R 0=1.4–2.3 and T g=1.3–2.71 days for the 2009 influenza pandemic.21, 22 We used 66.7 per cent of symptomatic rate23 in the simulations, and assume that one-third of the generation time is uninfectious (latent).21 The base transmission probability at which an infectious person may infect his/her susceptible contacts is 0.04. The transmisson probability is doubled if the person is symptomatic infectious, and meanwhile, half of the contacts are randomly removed owing to self-isolation or self-shielding.
Each of the simulation scenarios, including the baseline case, ran for 200 days and iterated 100 times. All the results reported in the following section are average values of the 100 simulation runs. Every simulation started at day 0 with 10 infectious persons randomly seeded into a susceptible population without prior immunity to the influenza virus. The modeled population is assumed to be a closed system, meaning that there are no people flowing into the system and consequently no newly imported cases. In our experiments, there were four candidate trigger thresholds (0.02, 0.25, 1.5, and 5 per cent) and five implementation durations (2, 4, 6, 8, and 10 weeks) for creating an intervention scenario, leading to a total of 20 different scenarios. In addition, we simulated three more scenarios: the uncontrolled epidemic, and two scenarios for evaluating the impacts of higher trigger thresholds (10 and 15 per cent) for a short school closure (2 weeks).
We evaluated the effectiveness of interventions by examining the attack rate (AR), peak incidence (PI), and peak day (PD). AR refers to the cumulative proportion of symptomatic cases of influenza infection in the overall population; PI refers to the highest daily incidence of symptomatic cases; and PD refers to the day when the PI happens. From a public health perspective, AR indicates the size of epidemic and the overall burden on the public health system because of an epidemic; and PI and PD describe the challenge to public health system in response to patient surges.
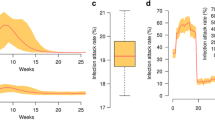
Dynamics of influenza spread without intervention
Figure 3 shows the results of the uncontrolled scenario. The epidemic reaches its peak on day 26 and fades out on day 73. The total AR is 44.47 per cent (95 per cent CI, 44.45–44.48); PI is 42.45 per 1000 people (95 per cent CI, 41.72–43.17); and the PD is day 26. This result is comparable with 43.5 per cent AR found by Germann et al. 24 It is noted that the trigger thresholds (0.02, 0.25, 1.5, 5, 10, and 15 per cent) are reached on day (7, 13, 17, 20, 22, 24), respectively.
Impacts of temporal factors on all-school closure
Figure 4 shows the effects of trigger thresholds and durations on the AR with an all-school closure scenario. The ARs after implementing school closure are in the range of 40.42–44.45 per cent, with a 0.05–9.10 per cent reduction compared to that of the baseline case. The lowest AR occurs when 10-week school closure is triggered at 0.02 per cent.
The longer intervention duration leads to a lower AR. An 8-week all-school closure is sufficient in our settings. Extending the duration of closure does not reduce the AR significantly. Moreover, the influences of trigger threshold show an interesting pattern: for duration<6 weeks, having a higher threshold leads to a lower AR; if duration>6 weeks, a rising threshold results in a slightly higher AR; if the duration=6 weeks, a convex shape appears as shown in Figure 4.
A short period of closure may be more effective, if it is implemented at reasonably higher thresholds (before the epidemic peak) when more infectious patients exist in the population. That is because a larger number of potential infections could be blocked owing to contact removal. Our results show that the 2-week closure is the least effective one, and its impacts are only noticeable when it is triggered at 1.5 per cent and above. Four-week closure is able to influence the AR when it is triggered as early as at 0.02 per cent, and a steady decline in AR is observed when its threshold rises. When the closure is sufficiently long (>6 weeks), however, significant impacts can always be achieved as contact removal can be maintained until the late stage of the epidemic. To achieve a more significant reduction in AR or PI, it is advisable to start the long-duration closure as early as reasonable. At the cutoff point, the ARs for 6-week closures have a shape of convex curve, showing the existence of both trends.
We showed a trend – a higher threshold will cause a lower AR if the closure duration is<6 weeks. It is interesting that there is an upper bound of the threshold at which the trend is still valid. We show two extra scenarios where 2-week school closure is triggered at the thresholds of 10 and 15 per cent, respectively. In Figure 5, 2-week closure at 15 per cent threshold leads to a higher AR than at lower thresholds (5 and 10 per cent), not following the trend anymore. Instead, a convex function is again observed: the minimum AR is achieved at a rather high trigger threshold of about 10 per cent, probably too high to be acceptable for real-life implementations.
Our simulation results could help provide the suggestions for different needs. For cost-cautious reasons, policymakers may prefer shorter intervention, starting school closures with a relatively longer delay after the outbreak starts. To minimize the size of epidemic, policymakers should implement school closure as early as reasonable and keep it in place for more than 6 weeks. We also note that, for intervention with a shorter duration, it is more important to make a wise choice of trigger threshold. For example, for 2-week school closure, it could save extra 6.05 per cent of the overall population from infection at no additional cost by properly choosing the trigger threshold.
Figure 6 shows that all-school closure significantly reduces PI of the epidemic. The lowest PI under school closure is 30.75 per 1000 people, a 27.55 per cent reduction compared to that of the baseline case; achieved when 6-week closure is triggered at 0.25 per cent. Note that 4-week closure is sufficient for reducing the PI, as the extended closure does not bring in any significant benefit on easing the worst-case stress on public health systems. The influence of trigger thresholds on PI exhibits the similar trends, as discussed earlier: if duration>2 weeks, a rising threshold results in a slightly higher AR; if duration=2 weeks, the PIs have a shape of convex curve.
Figure 7 shows that all-school closure steadily delays the PD. Specifically, it can be observed that the PD is significantly affected by trigger threshold, but not by duration. When the threshold rises from 0.02 to 5 per cent, PD steadily moves earlier. The longest delay obtained is 5 days compared to the baseline. It is achieved when any closure longer than 2 weeks is triggered at 0.02 per cent.
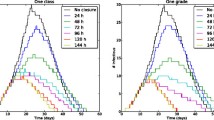
Validation of Conclusions under Different Transmission Rates
We have observed patterns of how epidemics are influenced by temporal factors when R 0=1.9. To evaluate whether the observations remain valid in social systems exposed to different virus strains, we performed simulations with different values of R 0 at 1.5 and 2.3, respectively. The new simulation results demonstrate consistent patterns as observed in earlier sections.
Figure 8 shows the ARs under all-school closure when R 0=1.5. As when R 0=1.9, the AR drops when the trigger threshold rises from 0.02 to 5 per cent if the duration is less than 6 weeks. If duration is longer than 6 weeks, the AR may increase rather than decrease once the trigger threshold is higher than a certain value. The ARs show as convex functions of trigger threshold in different cases where school closures last for 6, 8, and 10 weeks, respectively.
Figure 9 echoes the findings in Figure 8. It is clearly shown that, when trigger threshold rises, the ARs decrease for 2-week closure and increase for 6–8- and 10-week closures. At the cutoff value of 4-week closure, the ARs clearly form into a convex function of trigger threshold.
Although it is impossible to evaluate all the possible different scenarios numerically, the above results suggest wide applicable range of our conclusions.
Discussion
School closure is a social distancing measure, which aims to reduce disease-causing contacts between individuals. As the production of vaccine and stockpiling of anti-viral drugs usually takes considerable time, the shortage of pharmaceuticals is always a challenge in the preparedness plan for pandemic influenza. Social distancing measures are necessary complements to the pharmaceutical interventions, especially when a novel strain of influenza emerges with a high transmission rate.
Our simulation results have shown that school closure are likely to lower ARs and daily incidence, and delay the PD in most intervention scenarios. Our observations show that under a cost-cautious situation in which short intervention is preferred, all-school closure should be implemented at a higher threshold (a later time); if reducing the epidemic size is the top priority, it is advisable to implement a longer school closure (more than 6 weeks) as early as reasonable to enjoy the benefits of a lower AR, a smaller PI and the delayed PD. Moreover, there is an upper-bound duration (8 weeks in this study) which is sufficiently long to suppress the AR and PI to a near-minimal level. Further extension of closure beyond this upper bound may be a waste of societal resources. It is therefore recommended to evaluate the appropriate timing of school closure beforehand, especially in cost-cautious situation.
Enforcing a social distancing policy always has considerable cost – both economic and social. Take school closure as an example. Its major cost comes from absenteeism of working parents, who have to stay at home to take care of their children. The social consequences of school closure raise ethical and social justice issues.10 Policymakers always need to evaluate the social and economic costs together with the epidemic measurements when planning for social distancing interventions. If cost is put into the consideration, any extra reduction in AR or PI owing to proper timing would be favorable, as no direct cost is incurred when varying the thresholds; meanwhile, any enhanced effort with prolonged duration should be deliberated because a substantial increase of cost might result. Besides costs, there are other practical issues. Implementing all-school closure at a threshold as low as 0.02 per cent may be a challenging decision for the policymakers to make, as it is when closure is to be implemented at a high threshold of 10 per cent. As huge cost is at stake, adequate justifications and evaluations are necessary before decision making.
The evaluation of intervention scenarios in this study is based on Singapore's social structure. Results may vary: (1) when the social structure is dramatically different, as heterogeneity of social structure plays an important role in the disease transmission, and therefore affects the outcomes of mitigation planning strategies as well; (2) when the epidemic setting is dramatically different from the ones in this study. A new influenza virus strain, for example, may have some unexpected new features in transmission rates, rates of asymptomatic infection, age distribution of infection, baseline immunity levels, and so on. Although our study in the section ‘Validation of conclusions under different transmission rates’ implies that many conclusions are likely to hold in different scenarios, the effectiveness of school closure could be quite different. The best timing needs to be carefully re-calculated accordingly.
We used the percentage of symptomatic cases in the overall population as the trigger threshold in this article. In real-life implementations, the number of symptomatic cases is often not accessible directly but has to be estimated based on the number of reported cases and the reporting rate. The unavoidable errors in estimation may also affect the effectiveness of intervention.
Besides the caveats mentioned above, social behaviors may drastically change during the period of high influenza incidences. Such changes obviously affect the disease propagation patterns and consequently affect the effectiveness of various intervention strategies – including school closure. Parents staying at home can, for example, help strengthen the school closure distancing and at the same time, lowering the contacts at workplaces as well. On the other hand, some social gathering activities25 may easily weaken the effectiveness of school closure, especially when school closure happens at an early-stage of outbreak and people are yet not taking it very seriously. We believe that we need to conduct more comprehensive studies on such human behavior factors using relevant social survey, data collection, and careful comparisons with historical epidemic data.
In this article, we focus on studying the impacts of temporal factors on effectiveness of school closure. Whether school closure or any other intervention policy should be implemented in real life depends heavily on its associated costs, requiring careful, and sophisticated measures. In-depth studies on costs and cost-effectiveness of intervention policies are needed.
Conclusion
By conducting extensive simulations on an individual-based social network model, we studied the impacts of temporal factors on the effectiveness of school closure. Simulation results suggested that the trigger threshold and duration of school closure can both significantly affect the mitigation effectiveness, and proper timing is more important for school closure with a shorter duration. Such results provide useful insights for policymakers to make better decisions in influenza preparedness planning. The study also demonstrates the encouraging potential of a sophisticated individual-based simulation model in evaluating intervention policies in specific situations with specific constraints.
References
Nicoll, A. and Coulombier, D. (2009) Europe's initial experience with pandemic (H1N1) 2009 – Mitigation and delaying policies and practices. Eurosurveillance 14: 29.
Ortu, G., Mounier-Jack, S. and Coker, R. (2008) Pandemic influenza preparedness in Africa is a profound challenge for an already distressed region: Analysis of national preparedness plans. Health Policy and Planning 23 (3): 161–169.
Coker, R. and Mounier-Jack, S. (2006) Pandemic influenza preparedness in the Asia-Pacific region. The Lancet 368 (9538): 886–889.
Mounierjack, S. and Coker, R. (2006) How prepared is Europe for pandemic influenza? Analysis of national plans. The Lancet 367 (9520): 1405–1411.
Aledort, J., Lurie, N., Wasserman, J. and Bozzette, S. (2007) Non-pharmaceutical public health interventions for pandemic influenza: An evaluation of the evidence base. BMC Public Health 7 (1): 208.
Milne, G.J., Kelso, J.K., Kelly, H.A., Huband, S.T. and McVernon, J. (2008) A small community model for the transmission of infectious diseases: Comparison of school closure as an intervention in individual-based models of an influenza pandemic. PLoS ONE 3 (12): e4005.
Halder, N., Kelso, J. and Milne, G. (2010) Analysis of the effectiveness of interventions used during the 2009 A/H1N1 influenza pandemic. BMC Public Health 10 (1): 168.
Ferguson, N.M., Cummings, D.A., Fraser, C., Cajka, J.C., Cooley, P.C. and Burke, D.S. (2006) Strategies for mitigating an influenza pandemic. Nature 442 (7101): 448–452.
Lee, B.Y . et al (2010) Simulating school closure strategies to mitigate an influenza epidemic. Journal of Public Health Management and Practice 16 (3): 252–261.
Cauchemez, S. et al (2009) Closure of schools during an influenza pandemic. Lancet Infectious Diseases 9 (8): 473–481.
Cowling, B.J. et al (2008) Effects of school closures, 2008 winter influenza season, Hong Kong. Emerging Infectious Diseases 14 (10): 1660–1662.
Heymann, A., Chodick, G., Reichman, B., Kokia, E. and Laufer, J. (2004) Influence of school closure on the incidence of viral respiratory diseases among children and on health care utilization. Pediatric Infectious Disease Journal 23 (7): 675–677.
Newman, M.E.J. (2002) Spread of epidemic disease on networks. Physical Review E, Statistical, Nonlinear, and Soft Matter Physics 66 (1 Pt 2): 016128.
Del Valle, S., Hyman, J., Hethcote, H. and Eubank, S. (2007) Mixing patterns between age groups in social networks. Social Networks 29 (4): 539–554.
Meyers, L.A., Pourbohloul, B., Newman, M., Skowronski, D.M. and Brunham, R.C. (2005) Network theory and SARS: Predicting outbreak diversity. Journal of Theoretical Biology 232 (1): 71–81.
Girvan, M. and Newman, M.E.J. (2002) Community structure in social and biological networks. Proceedings of the National Academy of Sciences of the United States of America 99 (12): 7821–7826.
Zhang, T. et al (2009) HPCgen – A Fast Generator of Contact Networks of Large Urban Cities for Epidemiological Studies. International Conference on Computer Modelling and Simulation, Brno, Czech Republic.
Department of Statistics Singapore. (2010) Statistics Singapore – Census of population 2000 statistical release 5: Households & housing, http://www.singstat.gov.sg/pubn/popn/c2000sr5.html, accessed 4 August 2010.
Land Traffic Authority Singapore. (2010) LTA Annual Report FY08/09, http://www.lta.gov.sg/corp_info/annual_report_0809/index.htm, accessed 4 August 2010.
Diekmann, O., Heesterbeek, J.A. and Metz, J.A. (1990) On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. Journal of Mathematical Biology 28 (4): 365–382.
Fraser, C. et al (2009) Pandemic potential of a strain of influenza A (H1N1): Early findings. Science: 1176062.
Nishiura, H., Castillo-Chavez, C., Safan, M. and Chowell, G. (2009) Transmission potential of the new influenza A(H1N1) virus and its age-specificity in Japan. Euro Surveill 14 (22), http://www.ncbi.nlm.nih.gov/pubmed/19497256, accessed 19 July 2010.
Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team. (2009) Emergence of a novel swine-origin influenza A (H1N1) virus in humans. New England Journal of Medicine: 360: 2605–2615.
Germann, T.C., Kadau, K., Longini, I.M. and Macken, C.A. (2006) Mitigation strategies for pandemic influenza in the United States. Proceedings of the National Academy of Sciences 103 (15): 5935–5940.
Morbidity and Mortality Weekly Report (MMWR). (2009) Impact of seasonal influenza-related school closures on families – Southeastern Kentucky, February 2008, 58 (50): 1405–1409.
Acknowledgements
This work was supported in part by A–STAR Biomedical Research Council of Singapore under Grant 06/1/21/19/457. The authors sincerely thank Dr Mark Chen for his kind support in the local hospitalization data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Using a simulation model with real-life contact data in Singapore, the authors explored whether school closure will be effective in mitigating an influenza outbreak–and discovered the critical importance of timing of closures.
Rights and permissions
About this article
Cite this article
Zhang, T., Fu, X., Kwoh, C. et al. Temporal factors in school closure policy for mitigating the spread of influenza. J Public Health Pol 32, 180–197 (2011). https://doi.org/10.1057/jphp.2011.1
Published:
Issue Date:
DOI: https://doi.org/10.1057/jphp.2011.1