-
PDF
- Split View
-
Views
-
Cite
Cite
A. Taggart, E. Filippucci, G. Wright, A. Bell, A. Cairns, G. Meenagh, A. Pendleton, M. Rooney, S. Wright, A. Grey, W. Grassi, Musculoskeletal ultrasound training in rheumatology: the Belfast experience, Rheumatology, Volume 45, Issue 1, January 2006, Pages 102–105, https://doi.org/10.1093/rheumatology/kei162
Close - Share Icon Share
Abstract
Objectives. Despite the increasing use of musculoskeletal ultrasound (MSUS) as a clinical tool in rheumatology, there is no consensus yet regarding the standards required to achieve a basic level of competence in the use of this imaging technique. A number of sonographers worldwide are developing curricula and standardizing teaching methods in order to improve training in MSUS for rheumatologists. In the meantime, clinicians are devising informal means of training in order to acquire these new skills. Here we describe the informal team approach to MSUS training adopted by a group of rheumatologists from the Regional Rheumatology Centre in Belfast, UK.
Methods. Over a 5-yr period, eight rheumatologists from Musgrave Park Hospital in Belfast used a variety of means to learn the basic skills of MSUS.
Results. Seven of the team underwent a formal assessment of their competency in a practical examination devised by an experienced sonographer. All were judged to have attained a basic competency in MSU.
Conclusions. This Belfast experience shows what can be achieved despite the absence of formal MSUS training. Nevertheless, the development of recognized training programmes and international standards of competency are important goals on the way to achieving more widespread acceptance of MSUS as a useful tool in everyday clinical practice.
Over the last decade, there has been an explosion of interest in the potential of musculoskeletal ultrasound (MSUS) as a clinical tool in rheumatology [1–5]. Despite its undeniable value in a wide range of rheumatic conditions, several issues concerning both training and competency still wait to be addressed [6–12]. The lack of a standardized training curriculum and the scarcity of recognized training programmes are significant obstacles to the more widespread use of MSUS in the field of rheumatology.
It is not uncommon for a rheumatologist in training to be given the opportunity to acquire ultrasonographic (US) skills and experience while the more senior members of the medical team remain untrained. This can lead to a situation where the rheumatologist–sonographer becomes an isolated figure within the team. In this context, our experience in a busy rheumatology department could represent one way of solving the problem of sonographic training.
This paper describes how a group of rheumatologists from Belfast adopted a team approach to enable them to acquire the basic skills of MSUS.
The Belfast Rheumatology Unit
The Regional Rheumatology Centre for Northern Ireland is based in Musgrave Park Hospital in Belfast and provides a specialist service for a population of approximately one million people. Five years ago, the medical team consisted of nine medical specialists (five consultants and four specialist registrars in training). At that time, our particular interests included the use of biological therapies for severe inflammatory arthritis and the management of systemic lupus erythematosus and paediatric rheumatology, but none of us had any practical experience of MSUS.
In early 2000, two senior members of the team (A.T. and G.W.) decided to explore the possibility of using clinic-based MSUS in the unit. By a number of different means, we sought to acquire the practical skills to enable the whole team to achieve basic competency in MSUS. The Belfast training experience can be summarized in five main steps:
Attending courses in basic ultrasonography;
Purchasing our own US equipment;
Sabbatical leave in a centre of excellence;
Direct experience assisted by a tutor;
Competency assessment.
Acquiring US skills
First step: attending courses in basic ultrasonography
Our introduction to MSUS began in April 2000 when five members of the team attended the second EULAR (European League Against Rheumatism) Course in Basic Sonography in Zurzach, Switzerland. This was our first practical experience of the use of US in rheumatic patients. It reinforced our determination to continue to invest in US training. Later that year, seven of us attended the first BSR Course in Basic Ultrasound in Cambridge, UK and the following April, five attended the third EULAR Basic Sonography Course in Milan. In this way, the majority of the rheumatologists from Belfast were introduced to the practicalities of basic US and the conditions for learning together as a group were created. From 2001 to 2004, different members of the team attended a total of seven sonography courses (four EULAR Sonography Courses and three British Society for Rheumatology Courses), thus giving further impetus and continuity to our training.
Second step: purchasing our own US equipment
After attending the EULAR Sonography Course in Switzerland, we started to investigate the various options for acquiring our own MSUS equipment, as none was freely available to us in our hospital.
Initially, we purchased a Diasus (Dynamic Imaging, Livingstone, UK), which is a dedicated MSUS machine with high-frequency linear probes. Although this machine was not equipped with power Doppler, it provided high quality B-mode US imaging at a reasonable cost.
This proved ideal for training and detailed greyscale MSUS examination. Subsequently, we acquired several portable SonoSite 180 machines (Sonosite, Bothwell, WA, USA), which could be easily transported to outlying clinics for day-to-day clinical use, such as joint injections. Even though these portable US systems do not provide high-quality images, they permit a rapid assessment of the basic US findings, which can be confirmed by more detailed study at a later date, if necessary.
The acquisition of our own US equipment proved very important for the development of our US skills. The equipment was available to members of the team at all times and we were able to practice our US techniques on each other as well as on our patients.
During this phase, some members of our team attended US clinics conducted by an experienced local radiologist with a particular interest in sonography. He demonstrated US examination techniques at these clinics and at evening sessions specially organized for the group as a whole. With his assistance, we were able to build on the initial experience gained at the basic US courses.
Finally, in April 2004, we acquired a top-quality US system with power Doppler capability (Sonoline Antares; Siemens, Munich, Germany). This machine has enhanced our assessment of inflammatory rheumatic conditions and has enabled us to embark on a number of US research projects.
Third step: sabbatical leave in a centre of excellence
Attending sonography courses was an important way to maintain our enthusiasm for training in US but it was also a means of meeting the experts who conducted these courses. One such meeting led to an important training experience for several members of our team. Following the EULAR Sonography Course in Milan, Professor Walter Grassi invited one of our registrars (G.M.) to spend a week in the Clinica Reumatologica of the Università Politecnica delle Marche in Ancona, Italy. During that visit, the trainee performed US examinations for a minimum of 5 h each day under the direct supervision of an experienced US rheumatologist (with 7 yr of experience) and a member of the faculty of the EULAR Sonography Courses (E.F.). The experience was such a success that, over the next 18 months, a total of seven members of the Belfast team spent a sabbatical in Ancona, performing US in this way. Each visit was organized as an intensive 1-week US course for a maximum of two participants at a time.
Fourth step: direct experience assisted by a tutor
Following these visits to Ancona, the medical team in Belfast invited E.F. to come and study in the Regional Rheumatology Centre in Northern Ireland. From April to June 2004, E.F. spent 3 months in Belfast. During that time, he assisted and supervised members of the Belfast Rheumatology Unit in their MSUS practice. Every Monday afternoon, he conducted a 2-h seminar in practical MSUS techniques, focusing on specific topics as well as interesting cases drawn from the rheumatology wards and clinics. During this 3-month period, each trainee in the Belfast Rheumatology Unit performed no less than 100 MSUS examinations under expert supervision.
From July to November 2004, six members of the Belfast team performed MSUS on a regular basis. The average time devoted to MSUS by each member during this period was approximately 5 h a week.
Fifth step: competency assessment
Following his visit to Belfast, E.F. was invited to design a formal examination to test basic competency in clinical US which might be applicable to rheumatology trainees. In November 2004, he returned to Northern Ireland to conduct an evaluation of seven of the Belfast rheumatologists in obtaining and interpreting MSUS images.
The examination consisted of three parts: (i) a written paper of multiple-choice questions; (ii) a MSUS examination of healthy subjects; and (iii) a MSUS examination of patients with rheumatic diseases.
The multiple-choice questions focused on four main topics: MSUS technique, MSUS anatomy, MSUS pathology and MSUS image interpretation. Each question had five possible answers, only one of which was correct. There were 30 questions in total and candidates were given 60 min to answer them. The pass mark was 80%.
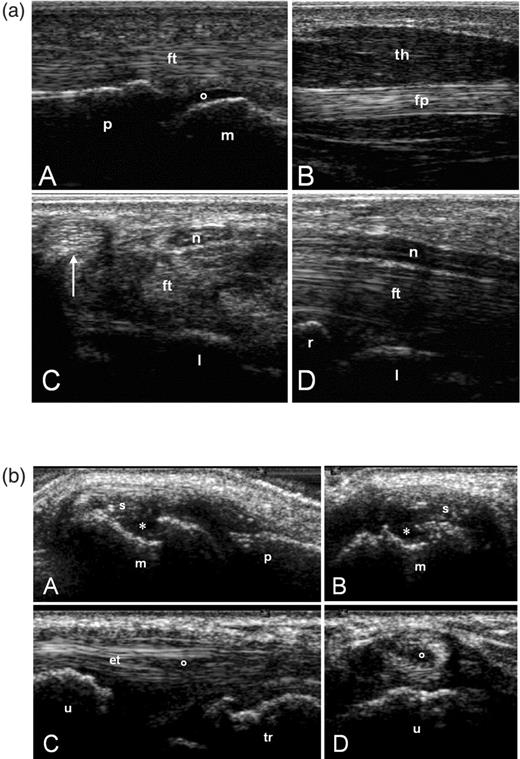
In the practical session with healthy subjects, each candidate was asked to perform 15 standard MSUS scans and store the best example of each scan. The scans were chosen randomly from the list of the standard scans outlined in the EULAR Guidelines for Musculoskeletal Ultrasound in Rheumatology [13]. Candidates were allowed 30 min to perform the 15 scans. The stored images were judged for quality according to a set of predefined criteria, which included satisfactory equipment setup, proper handling of the US probe and the presence of correct bony landmarks. Eighty per cent of the images had to be of satisfactory quality in order to pass this part of the examination. Figure 1a shows a representative sample of the US images taken in healthy subjects.
(a) US images taken during the practical session with healthy subjects. (A) Longitudinal volar scan of a metacarpophalangeal joint. (B) Longitudinal scan of the thenar eminence. Transverse (C) and longitudinal (D) volar scans of the carpal tunnel. m, metacarpal head; p, proximal phalanx; o, articular cartilage; ft, finger flexor tendons; fp, flexor pollicis longus tendon; th, muscles of the thenar eminence; l, lunate bone; n, median nerve; arrow, flexor carpi radialis tendon; r, radius. (b) US images taken during the practical session with patients with rheumatoid arthritis. (A, B) Metacarpophalangeal joint. Longitudinal (A) and transverse (B) dorsal scans showing synovial hypertrophy (s) and a bone erosion (*) of the metacarpal head (m). p = proximal phalanx. (C, D) Wrist. VI compartment of the extensor tendons. Longitudinal (C) and transverse (D) lateral scans showing a partial rupture (o) of the extensor carpi ulnaris tendon (et). u, ulna; tr, triquetrum.
The practical session with patients consisted of an US examination of two different anatomical sites. These were randomly chosen from the eight sites indicated in the EULAR Guidelines for Musculoskeletal Ultrasound in Rheumatology [13]: shoulder, elbow, wrist, hand, hip, knee, ankle and foot. The total time allowed to perform the two MSUS examinations was 30 min. Each candidate was asked to fill out a written report on their examination outlining the presence or absence of each pathological finding detectable by US. The day before the examination, the same examination was performed on all the patients by an experienced rheumatologist–sonographer (E.F.) or a local radiologist with a particular interest in sonography (A.G.). This provided a gold standard by which to judge the performance of each candidate. Candidates had to concur with not less than 80% of the examiners’ findings in order to pass this part of the examination. Figure 1b provides some examples of pathological conditions detected by the candidates during their US examination of the patients.
The results of the competency assessment are summarized in Table 1.
Results of the competency assessment
| CANDIDATE . | Multiple-choice questions: number of correct answers/number of questions (%) . | Practical session with the healthy subject: number of satisfactory US images/total number of US images (%) . | Practical session with the patients: number of correct US findings/number of US findings to detect (%) . | . | |
|---|---|---|---|---|---|
| 01 | 29/30 (96.7%) | 15/15 (100%) | Knee 13/14 (92.9%) | Ankle 20/21(95%) | |
| 02 | 24/30 (80%) | 15/15 (100%) | Knee 14/14 (100%) | Ankle 20/21(95%) | |
| 03 | 26/30 (86.7%) | 15/15 (100%) | Hand 9/9 (100%) | Knee 12/14(85.7%) | |
| 04 | 26/30 (86.7%) | 15/15 (100%) | Hand 8/9 (88.9%) | Knee 13/14(92.9%) | |
| 05 | 24/30 (80%) | 15/15 (100%) | Shoulder 18/19 (94.7%) | Foot 8/8 (100%) | |
| 06 | 29/30 (96.7%) | 15/15 (100%) | Wrist 11/11 (100%) | Foot 7/8 (87.5%) | |
| 07 | 29/30 (96.7%) | 15/15 (100%) | Shoulder 16/19 (84%) | Ankle 21/21(100%) | |
| Total | 187/210 (89%) | 105/105 (100%) | 190/202 (94.1%) | ||
| CANDIDATE . | Multiple-choice questions: number of correct answers/number of questions (%) . | Practical session with the healthy subject: number of satisfactory US images/total number of US images (%) . | Practical session with the patients: number of correct US findings/number of US findings to detect (%) . | . | |
|---|---|---|---|---|---|
| 01 | 29/30 (96.7%) | 15/15 (100%) | Knee 13/14 (92.9%) | Ankle 20/21(95%) | |
| 02 | 24/30 (80%) | 15/15 (100%) | Knee 14/14 (100%) | Ankle 20/21(95%) | |
| 03 | 26/30 (86.7%) | 15/15 (100%) | Hand 9/9 (100%) | Knee 12/14(85.7%) | |
| 04 | 26/30 (86.7%) | 15/15 (100%) | Hand 8/9 (88.9%) | Knee 13/14(92.9%) | |
| 05 | 24/30 (80%) | 15/15 (100%) | Shoulder 18/19 (94.7%) | Foot 8/8 (100%) | |
| 06 | 29/30 (96.7%) | 15/15 (100%) | Wrist 11/11 (100%) | Foot 7/8 (87.5%) | |
| 07 | 29/30 (96.7%) | 15/15 (100%) | Shoulder 16/19 (84%) | Ankle 21/21(100%) | |
| Total | 187/210 (89%) | 105/105 (100%) | 190/202 (94.1%) | ||
Results of the competency assessment
| CANDIDATE . | Multiple-choice questions: number of correct answers/number of questions (%) . | Practical session with the healthy subject: number of satisfactory US images/total number of US images (%) . | Practical session with the patients: number of correct US findings/number of US findings to detect (%) . | . | |
|---|---|---|---|---|---|
| 01 | 29/30 (96.7%) | 15/15 (100%) | Knee 13/14 (92.9%) | Ankle 20/21(95%) | |
| 02 | 24/30 (80%) | 15/15 (100%) | Knee 14/14 (100%) | Ankle 20/21(95%) | |
| 03 | 26/30 (86.7%) | 15/15 (100%) | Hand 9/9 (100%) | Knee 12/14(85.7%) | |
| 04 | 26/30 (86.7%) | 15/15 (100%) | Hand 8/9 (88.9%) | Knee 13/14(92.9%) | |
| 05 | 24/30 (80%) | 15/15 (100%) | Shoulder 18/19 (94.7%) | Foot 8/8 (100%) | |
| 06 | 29/30 (96.7%) | 15/15 (100%) | Wrist 11/11 (100%) | Foot 7/8 (87.5%) | |
| 07 | 29/30 (96.7%) | 15/15 (100%) | Shoulder 16/19 (84%) | Ankle 21/21(100%) | |
| Total | 187/210 (89%) | 105/105 (100%) | 190/202 (94.1%) | ||
| CANDIDATE . | Multiple-choice questions: number of correct answers/number of questions (%) . | Practical session with the healthy subject: number of satisfactory US images/total number of US images (%) . | Practical session with the patients: number of correct US findings/number of US findings to detect (%) . | . | |
|---|---|---|---|---|---|
| 01 | 29/30 (96.7%) | 15/15 (100%) | Knee 13/14 (92.9%) | Ankle 20/21(95%) | |
| 02 | 24/30 (80%) | 15/15 (100%) | Knee 14/14 (100%) | Ankle 20/21(95%) | |
| 03 | 26/30 (86.7%) | 15/15 (100%) | Hand 9/9 (100%) | Knee 12/14(85.7%) | |
| 04 | 26/30 (86.7%) | 15/15 (100%) | Hand 8/9 (88.9%) | Knee 13/14(92.9%) | |
| 05 | 24/30 (80%) | 15/15 (100%) | Shoulder 18/19 (94.7%) | Foot 8/8 (100%) | |
| 06 | 29/30 (96.7%) | 15/15 (100%) | Wrist 11/11 (100%) | Foot 7/8 (87.5%) | |
| 07 | 29/30 (96.7%) | 15/15 (100%) | Shoulder 16/19 (84%) | Ankle 21/21(100%) | |
| Total | 187/210 (89%) | 105/105 (100%) | 190/202 (94.1%) | ||
Current practice
In our Department, MSUS is now used regularly as a clinical tool to assist with patient assessment and joint or soft tissue injection. Time constraints make it difficult for us to perform MSUS in our busy out-patient follow-up clinics but more time is available in the new patient clinics and in the in-patient and day ward setting. We have not reduced the patient numbers at any of our clinics but would have to do so were we to use US in our routine follow-up clinics. Of the eight rheumatologists who embarked on this programme of informal training, six are still practising MSUS on a regular basis. On average, each member of the team performs ultrasound during three or four clinical sessions per week on a total of 15–20 patients. Some of these US examinations will be assessments prior to joint aspiration/injection and others will consist of more detailed study of an anatomical area. Because of the nature of our clinical practice, over half of our scans are carried out on patients with inflammatory arthritis (rheumatoid arthritis, psoriatic arthritis, juvenile arthritis etc.) but a substantial number are in patients with painful shoulders or soft-tissue rheumatism (carpal tunnel syndrome, painful heel, tennis elbow).
Some joint injections are carried out under direct ultrasound guidance (e.g. heel, shoulder) but others are performed after scanning the joint and marking the skin (e.g. hip). US enables us to pinpoint the exact depth of the structure to be injected as well as its position. Simple joint injections are still carried out blindly but the majority benefit from US assessment prior to injection.
In many cases, the examination reveals unsuspected abnormalities of the tendons and soft tissues where isolated joint pathology was suspected. Workers from Leeds have demonstrated the value of MSUS in everyday clinical practice [5] and our experience bears this out. In a recent audit, we estimated that US scanning influenced the clinical management of our patients in 70% of cases.
Five years ago, approximately 5% of our patients were referred to the Department of Radiology for formal US examination. This figure has not changed significantly since then but this service is still invaluable to us in cases of diagnostic uncertainty. In many cases, our practice of clinic-based US complements rather than duplicates that of the radiologist–sonographer. We do not seek to use US to provide a detailed anatomical diagnosis but use the technique to refine and extend our clinical skills. MSUS requires a detailed knowledge of musculoskeletal anatomy. Acquiring that knowledge has improved our musculoskeletal examination technique and has given us a better understanding of exactly how different diseases affect the joints.
Our overall investment in US equipment and courses now exceeds £250 000. These funds have come from a variety of different sources, including the pharmaceutical industry, a local arthritis charity and two health-care trusts. These figures do not take account of the considerable time invested in training. Constant practice under expert guidance is the single most important key to success in MSUS training.
Discussion
The development of MSUS in the Belfast Rheumatology Unit has been unusual in that a majority of the medical team have been involved in the enterprise from the outset. Our experience shows what can be achieved in a relatively short period of time despite the lack of a formal training programme or curriculum. Although our training has been largely informal, in many ways it has been more rigorous than that undertaken by most UK radiology trainees. In our case, the main obstacle to progress has been the lack of an expert trainer in MSUS within our own hospital. We have overcome this difficulty with the help of colleagues from outside, but undoubtedly our task would have been easier if we had been able to train under constant expert supervision and had had a curriculum to follow.
Physicians who perform US must always be aware of the limits of their experience and competence. This is particularly true for those of us who are in the earlier phases of learning this new technique. From the outset, we have audited our practice of MSUS and all our trainees are required to keep a personal logbook of their scans to facilitate this process.
At the present time, there is a lack of experienced musculoskeletal sonographers in the UK who are available to act as trainers. This situation should improve as clinic-based US becomes more widely accepted, but more controlled trials are needed if we are to convince rheumatologists that the technique can improve patient care [3, 14].
MSUS is an integral part of rheumatology training in a number of European countries [15–17] and EULAR has recognized the importance of MSUS by setting up its own Working Party on Imaging in Rheumatology. This international dimension will prove decisive in the development of recognized standards of training and competency [7, 8]. This is an essential step towards achieving more widespread acceptance of MSUS as a clinical tool in rheumatology. It will also prove important from a clinical governance perspective.
Our training experience is a testimony to the value of collaboration with colleagues when developing new clinical skills. We still have a great deal to learn before we can call ourselves rheumatologist–sonographers but we would never have got this far had it not been for the encouragement and support of our radiology colleague and of the experts from the Clinica Reumatologica of the Università Politecnica delle Marche in Ancona.
We thank Dr Michelle McHenry and Sister Joyce Patton for their assistance in organizing the competency assessment.
The authors have declared no conflicts of interest.
References
Grassi W, Filippucci E, Busilacchi P. Musculoskeletal ultrasound.
Kane D, Balint PV, Sturrock R, Grassi W. Musculoskeletal ultrasound—a state of the art review in rheumatology. Part 1: Current controversies and issues in the development of musculoskeletal ultrasound in rheumatology.
Kane D, Grassi W, Sturrock R, Balint PV. Musculoskeletal ultrasound—a state of the art review in rheumatology. Part 2: Clinical indications for musculoskeletal ultrasound in rheumatology.
Karim Z, Wakefield RJ, Conaghan PG et al. The impact of ultrasonography on diagnosis and management of patients with musculoskeletal conditions.
Grassi W, Salaffi F, Filippucci E. Ultrasound in rheumatology.
Brown AK, O’Connor PJ, Wakefield RJ, Roberts TE, Karim Z, Emery P. Practice, training, and assessment among experts performing musculoskeletal ultrasonography: toward the development of an international consensus of educational standards for ultrasonography for rheumatologists.
Brown AK, O’Connor PJ, Roberts TE, Wakefield RJ, Karim Z, Emery P. Recommendations for musculoskeletal ultrasonography by rheumatologists: setting global standards for best practice by expert consensus.
Speed CA, Bearcroft PW. Musculoskeletal sonography by rheumatologists: the challenges.
Filippucci E, Unlu Z, Farina A, Grassi W. Sonographic training in rheumatology: a self teaching approach.
D’Agostino MA, Maillefert JF, Said-Nahal R, Breban M, Ravaud P, Dougados M. Detection of small joint synovitis by ultrasonography: the learning curve of rheumatologists.
Balint PV, Sturrock RD. Intraobserver repeatability and interobserver reproducibility in musculoskeletal ultrasound imaging measurements.
Backhaus M, Burmester G-R, Gerber T et al. Guidelines for musculoskeletal ultrasound in rheumatology.
Hall S, Buchbinder R. Do imaging methods that guide needle placement improve outcome?
Manger B, Kalden JR. Joint and connective tissue ultrasonography—a rheumatologic bedside procedure? A German experience.
Grassi W, Cervini C. Ultrasonography in rheumatology: an evolving technique.
Author notes
Department of Rheumatology, Musgrave Park Hospital, 1Department of Radiology, Belvoir Park Hospital, Belfast, UK and 2Department of Rheumatology, Università Politecnica delle Marche, Ancona, Italy.



Comments