Abstract
This study was designed to identify differences in red blood cell (RBC) incorporation and iron absorption in premature infants between iron provided in a premature infant formula compared with iron provided as a supplement between feedings. We used a triple stable isotope technique in which 13 infants received 57Fe mixed with Enfamil Premature Formula on d 1 of the study, and 54Fe with a multivitamin supplement between meals on d 2. Two weeks later, blood was drawn for isotope analysis and 58Fe was given i.v. The percentage RBC incorporation of the 54Fe and 57Fe was calculated, and the percent absorption of these tracers was estimated by dividing by the percentage of 58Fe identified in RBCs 14 d after its infusion. We found a small, but significantly greater, percentage of RBC incorporation of the 54Fe given as a supplement compared with the 57Fe given in the formula (9.7 ± 3.8% versus 7.8 ± 3.1%, p = 0.02). The RBC 57Fe incorporation was closely correlated with the reticulocyte count (r = 0.80, p = 0.001), but not the serum ferritin or the Hb concentration. Approximately 68% of an i.v. dose of 58Fe was incorporated into RBCs. These findings indicate 1) iron is incorporated well into RBCs from preterm infant formula, with only a small increase in incorporation when given as a supplement, and 2) the reticulocyte count, but not the Hb concentration, is a good measure of RBC iron-incorporating capacity.
Similar content being viewed by others
Main
The benefits of iron supplementation for premature infants are well documented (1–3). However, the optimal timing and method of iron supplementation remain controversial. Concerns regarding iron toxicity and adverse reactions, such as gastrointestinal intolerance and infection, led to recommendations to delay iron supplementation (1–3). More recently, a desire to decrease the rate of blood transfusions given to premature infants, together with studies on the use of recombinant human erythropoietin to induce erythropoiesis, have led to an interest in providing iron as soon as enteral feedings are established, and identifying specific populations of premature infants in whom iron supplementation may be most beneficial (4).
To meet this need for early iron therapy, premature infant formulas containing supplemental iron have been introduced. Despite wide utilization of these formulas, there is uncertainty regarding premature infants' absorption of the iron contained in fortified formulas compared with that of iron given as a separate, nonfeeding-related, supplement. This concern is partly related to the potentially adverse effect on iron absorption of the high calcium concentrations such as those found in cow's milk and in formulas designed for premature infants (5,6).
Few studies of iron absorption in premature infants are available due to difficulties in the use of mass balance and radioactive tracer techniques in these infants (7,8). Recently, however, the availability of iron-stable isotope techniques has made studies of iron metabolism more practical and safe for infants (5,9–11). These studies are done by administering a minor stable isotope of iron orally and determining its presence (incorporation) in RBCs 14 d later. When an i.v. dose of a different isotope of iron is also administered, the relative recovery of these isotopes is a measure of iron absorption. This study was designed to use this multitracer technique to compare the absorption and RBC incorporation in premature infants of iron provided in premature infant formulas compared with iron given as a separate supplement between feedings.
METHODS
Subjects. We studied 13 premature infants, 27-30 wk of gestational age, who were less than 1500 g in birth weight and appropriate for gestational age. Infants were excluded from enrollment if they had a diagnosis of bronchopulmonary dysplasia or an oxygen requirement >30% at the time of the study, major intraventricular hemorrhage, history of necrotizing enterocolitis or gastrointestinal surgery, or chronic disorders affecting liver or renal function.
The protocol was approved by the Institutional Review Board for Human Subject Research at Baylor College of Medicine and Affiliated Hospitals. Informed written consent was obtained from the parents of each subject before the study.
Study protocol. Infants were enrolled at 1-4 wk of age while receiving full intermittent orogastric bolus tube feedings (given over 10-20 min) of Enfamil Premature Formula with iron (EPF with iron, Mead Johnson Nutritionals, Evansville, IN) at a volume of 150-160 mL·kg-1 d-1. The study was begun when the feeding volume was at this level, and the infant had not been receiving parenteral nutrition for 7-10 d. This amount of formula delivers approximately 2.2 mg of iron·kg-1 d-1. On the first day of the study, 0.7 mg of 57Fe was given by mixing it in two feedings of low iron-containing Enfamil Premature Formula. Low iron formula was used so that the total iron in the two feedings after addition of the 57Fe would be similar to the amount of iron in two feedings of the routine iron-fortified formula. Blood was obtained for Hb concentration, serum ferritin, and reticulocyte count. The next day, 2.0 mg of 54Fe were given with 1.0 mL of a multivitamin supplement, Tri-Vi-Sol (without iron, Mead-Johnson Nutritionals, Evansville, IN) 1.5 h after completion of a bolus tube feeding. Tri-Vi-Sol contains 35 mg/mL vitamin C, as well as vitamins A and D. Before dosing, gastric residual content was assessed by syringe aspiration from the orogastric tube, and if <20% of a feeding remained, the isotope was given. Fourteen days later, a 1-mL sample of blood was obtained for isotope ratio analysis and measurement of Hb concentration. Immediately thereafter, the infants received 0.2 mg of 58Fe i.v. An additional 1 mL of blood was obtained 14 d later for isotope ratio analysis.
Isotope and sample preparation and analysis. The methods for the preparation of iron-stable isotopes for human use and mass spectrometric analysis of samples from studies in infants have been described previously (5,12,13). In brief, iron isotopes are purchased as the metal and prepared as ferrous sulfate. This is done by dissolving the metal in concentrated nitric acid and 0.5 M sulfuric acid. For isotope administered with an infant formula, the tracer is mixed with the formula 12-24 h before feeding. The 58Fe administered i.v. was prepared as 58Fe-citrate in saline at a concentration of 0.01 mg/mL 58Fe by Merck-Frosst of Canada. It was tested for sterility and pyrogenicity before use. A total of 20 mL of the solution were administered i.v. using a butterfly infusion set over 30 min.
Iron samples were prepared for mass spectrometric analysis using an anion exchange technique (13). Isotope ratio analysis was performed using a magnetic sector thermal ionization mass spectrometer. Because three isotopes were used in this study, fractionation correction could not be applied to the final analysis of the 58Fe/56Fe ratio obtained after i.v. administration of 58Fe. Fractionation correction is a mathematical adjustment in which the measured isotope ratios are corrected by comparison with the known ratio of two unadministered isotopes (14). In this case, because there are only four iron isotopes, when three are given in a study, this correction cannot be applied. When fractionation correction cannot be applied, the accuracy of the final isotope ratios is lowered, depending on the element- and heat-specific magnitude of the fractionation. This is minimized using careful temperature monitoring of the filament mass spectrometer during analysis. However, even using careful temperature control, the accuracy of the noncorrected final enrichment measurement for iron worsens from 0.2% to 1.0% compared with fractionation-corrected measurements (12). To allow for this diminished measurement accuracy, we administered a dose of 58Fe that would result in an enrichment of the 58Fe/56Fe ratio of 30-60%. Serum ferritin was measured using a fluoroimmunoassay (Wallac Inc., Gaithersburg, MD).
Calculations. Iron incorporation was determined from RBCs as previously described by evaluating the recovery of the isotope in RBC obtained 14 d after isotope administration (5,10,12). Circulating iron was calculated using a mean blood volume of 80 mL/kg (15), the measured Hb concentration, and the concentration of iron in Hb (3.47 mg/g). In this study, the body weight and Hb concentration used in the calculation were those on the day the isotopes were administered.
The percentage absorption of iron was estimated for the 54Fe and 57Fe by dividing the percentage RBC incorporation of these isotopes by the percentage of the i.v. dose, 58Fe, which was incorporated into RBCs. A limitation in this study is that the i.v. isotope was administered 14 d after the oral isotopes. This was done to enhance the accuracy of the isotope ratio measurements performed after oral dosing and to ensure that low doses of these isotopes were used. However, it is likely that some change in absorbing capacity occurred in the premature infants during these 14 d that might affect the ultimate calculation of absorption. For these reasons, the primary outcome variable of this study is the RBC incorporation, rather than the fractional absorption.
Statistical analysis. The relationship between iron absorption from the two methods of administration was compared by paired t test. Linear regression analysis was used to relate Hb concentration, reticulocyte count, and serum ferritin to iron absorption. The sample size determination before the study was based on identifying a 25% difference (p = 0.05) in the RBC incorporation of the iron administered in the formula compared with that given as a supplement.
RESULTS
Characteristics of the study subjects are shown in Table 1. There were eight female and five male infants. Seven infants were Caucasian, four were African-American, and two were Hispanic. No infant received blood transfusions during the 2 wk before or during the study. Total blood transfusion volume (packed RBCs) was less than 35 mL in 12/13 infants. One infant (subject 3) had received 60 mL of transfused packed RBCs early in his hospital course. Results from this infant were similar to those of the other study subjects.
Isotope enrichments for each of the study subjects for the three administered isotopes are shown in Table 2. The RBC incorporation of the 57 Fe administered with Enfamil Premature Formula averaged 7.8 ± 3.1% of the dose (range 1.8-13.7%), which is significantly different (t = 2.6, p = 0.02) from the RBC incorporation of 54 Fe given as a supplement between feedings that averaged 9.7 ± 3.8% of the dose (range 4.1-16.3%) (Table 3). The RBC incorporation of the i.v. administered 58Fe averaged 68.3 ± 9.5% of the dose (range 51.8-84.9%). The estimated percent absorption for 57Fe was 11.4 ± 4.4% and for 54Fe was 14.6 ± 6.5% (p = 0.02 for the difference between these values).
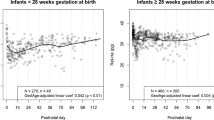
The RBC incorporation of 54Fe and 57Fe was closely correlated (r = 0.71, p = 0.007) (Fig. 1). There was no correlation between the Hb concentration (range 77-105 g/L) or the serum ferritin (range 35-200 µg/L) and the percentage absorption or the RBC incorporation of 54Fe or 57Fe. There was a significant correlation between the reticulocyte count and the R incorporation of 57Fe (r = 0.80, p = 0.001) (Fig. 2). The RBC incorporation of 54Fe from the supplement was not significantly correlated with the reticulocyte count (r = 0.48, p = 0.10). This relationship might have reached significance with a larger sample size.
There was no significant correlation between gestational age, age at the time of the study, body weight, Hb concentration, or serum ferritin at the time of the study and absorption or incorporation of any of the isotopes (r ≤ 0.25, p > 0.4 for each).
DISCUSSION
Measurement of RBC incorporation of an orally administered iron isotope allows for an assessment of the utilization of the iron from that source. We identified a small but statistically significant difference between the RBC incorporation and absorption of iron when premature infants receive the iron mixed in their formula compared with administration as a separate supplement. However, this statistical difference may not have important physiologic consequences. Rather, the small size of this difference indicates that, despite the presence of potential inhibitors of iron absorption in a formula, such as milk proteins and calcium (5,6,16,17), premature infants are able to absorb iron well when fed in premature infant formula. The effects of other nutrients present in relatively high concentrations in premature infant formula, such as ascorbic acid and zinc, on iron absorption could not be identified from this study.
Although we did not directly label the iron contained in preterm formula, our results are expected to closely simulate the results obtained in clinical use of iron-fortified preterm formula. This is because the iron in formula is principally added as ferrous sulfate extrinsically during processing, and is likely to have availability comparable to the 57Fe sulfate we extrinsically added.
The fractional iron absorption of 11% we found for iron given with preterm formula is comparable to the absorption fractions reported for term infants who are fed cow's milk, but slightly lower than for human milk-fed full-term infants (7,13). Of note is that the variability in the RBC incorporation fraction in this study is much lower than that found in previous studies involving full-term infants (12,18). This may be related to the lack of solid foods in the diet and the similarity of the dietary intake in infants at each feeding.
Assuming that the iron absorption we measured from the 57Fe is the rate at which iron is absorbed from each feeding, the net daily iron absorbed would be 236 µg/d. This value is similar to a recommended i.v. iron dose for premature infants, although it is less than the estimated iron needed for growing premature infants (2,19,20). However, definitive data regarding the risks and benefits of various levels of iron intake by premature infants, especially those not receiving erythropoietin, are not available (2).
Our results demonstrate that the reticulocyte count is a useful biochemical marker for assessing RBC iron incorporation. In contrast, neither the Hb concentration nor the serum ferritin was correlated with iron absorption or incorporation. This finding regarding serum ferritin is similar to that reported by Ehrenkranz et al. (10) in premature infants and is in contrast to our finding of a significant inverse correlation between serum ferritin and RBC iron incorporation in 6-mo-old infants (13).
In adults and older children, 80-90% of absorbed iron is incorporated into RBCs. This fraction may be much lower in individuals under special circumstances, such as premature infants, and children or adults with chronic diseases, such as rheumatoid arthritis. We used an i.v. 58Fe isotope to measure directly the fraction of absorbed iron that is incorporated into RBCs. However, comparisons may be made between our findings and those of other studies using similar techniques. Our study population showed an average of 68% of the i.v. administered 58Fe was incorporated into RBCs. This is much higher than the approximately 18% incorporation reported using a similar technique by Zlotkin et al. (9).
The reason for the higher incorporation in our study may be related to differences in study populations, including body weight and transfusion history. Our infants were much larger at the time of the i.v. infusion than those of Zlotkin et al. (9) and had not recently been transfused. It is likely that both of these factors led to the higher incorporation seen in our study. This conclusion is supported by the early results of Gorten et al. (6), who used balance techniques and an oral dose of 59Fe to measure a mean iron incorporation of 52% in older premature infants. Taken together, these findings suggest that absorbed iron is well used for RBC incorporation in minimally transfused infants during their period of active growth (between approximately 1.5 and 2.0 kg).
In conclusion, small but identifiable differences exist in the utilization by premature infants of iron when administered with formula or as a supplement. These data, however, support the efficacy of iron absorption from iron-fortified formulas used for feeding premature infants. Whether higher levels of supplementation would be beneficial is not known.
Abbreviations
- RBC:
-
red blood cell
REFERENCES
Siimes MA, Jarvenpaa AL 1982 Prevention of anemia and iron deficiency in very low-birth-weight infants. J Pediatr 101: 277–280
Oski FA 1985 Iron requirements of the premature infant. In: Tsang RC (ed) Vitamin and Mineral Requirements in Preterm Infants. Marcel Dekker, New York, 9–21.
American Academy of Pediatrics Committee on Nutrition 1985 Nutritional needs of low-birth-weight infants. Pediatrics 75: 976–986
Gallagher PG, Ehrenkranz RA 1993 Erythropoietin therapy for anemia of prematurity. Clin Perinatol 20: 169–191
Abrams SA, O'Brien KO, Wen J, Liang LK, Stuff JE 1996 Absorption by 1-year-old children of an iron supplement given with cow milk or juice. Pediatr Res 39: 171–175
Heinrich HC, Gabbi EE, Whang DH, Bender-Gotze C, Shafer KH 1975 Ferrous and hemoglobin 59Fe absorption from supplemented cow milk in infants with normal and depleted iron stores. Z Kinderheik 120: 251–258
Gorten MK, Hepner R, Workman JB 1963 Iron metabolism in premature infants. I. Absorption and utilization of iron as measured by isotope studies. J Pediatr 63: 1063–1071
Saarinen UM, Siimes MA 1979 Iron absorption from breast milk, cows milk and iron supplemented formula: an opportunistic use of changes in total body iron determined by hemoglobin, ferritin, and body weight in 132 infants. Pediatr Res 13: 143–147
Zlotkin SH, Lay DM, Kjarsgaard J, Longley T 1995 Determination of iron absorption using erythrocyte iron incorporation of two stable isotopes of iron (57Fe and 58Fe) in very low birthweight premature infants. J Pediatr Gastroenterol Nutr 21: 190–199
Ehrenkranz RA, Gettner PA, Nelli CM, Sherwonit EA, Williams JE, Pearson HAN, Ting BT, Janghorbani M 1992 Iron absorption and incorporation into red blood cells by very low birth weight infants: studies with the stable isotope 58Fe. J Pediatr Gastroenterol Nutr 15: 270–278
Kastenmayer P, Davidsson L, Galan P, Cherouvrier F, Hercberg S, Hurrell RF 1994 A double stable isotope technique for measuring iron absorption in infants. Br J Nutr 71: 411–424
Abrams SA, Wen J, O'Brien KO, Stuff JE, Liang LK 1994 Application of magnetic sector thermal ionization mass spectrometry to studies of erythrocyte iron incorporation in small children. Biol Mass Spectrom 23: 771–775
Abrams SA, Wen J, Stuff JE 1997 Absorption of calcium, zinc and iron from breast milk by five- to seven-month-old infants. Pediatr Res 41: 384–390
Platzner IT, Habfast K, Walder AJ, Goetz A 1997 Modern Isotope Ratio Mass Spectrometry. Wiley & Sons, Chichester, UK, 178–181.
Maertzdorf WJ, Aldenhuyzen-Dorland W, Slaaf DW, Tangelder GJ, Blanco CE 1991 Circulating blood volume in appropriate and small for gestation age fullterm and preterm polycythemic infants. Acta Paediatr Scand 80: 620–627
Hallberg L, Rossander-Hulten L, Brune M, Gleerup A 1992 Calcium and iron absorption: mechanism of action and nutritional importance. Eur J Clin Nutr 46: 317–322
Hurrell RF, Lynch SF, Trinidad TP, Dassenko SA, Cook JD 1989 Iron absorption in humans as influenced by bovine milk proteins. Am J Clin Nutr 49: 546–552
Davidsson L, Kastenmayer P, Yuen M, Lonnerdal B, Hurrell RF 1993 Influence of lactoferrin on iron absorption from human milk in infants. Pediatr Res 35: 117–124
Friel JK, Andrews WL, Hall MS, Rodeay MS, Keith M, McCloy UC, Matthews JD, Long DR 1995 Intravenous iron administration to very-low-birth-weight newborns receiving total and parenteral nutrition. J Parenter Enteral Nutr 19: 114–118
Zlotkin S. 1985 Total parenteral nutrition in children. Pediatr Clin North Am 32: 375–400
Acknowledgements
The authors thank the nursing staff of the General Clinical Research Center of the Texas Children's Hospital; Pamela Burns, RN, for nursing care of the study subjects; Lily Liang, Jianping Wen, and Cindy Clarke, for technical assistance; and Leslie Loddeke for editorial assistance.
Author information
Authors and Affiliations
Additional information
Supported in part with federal funds from the USDA/ARS under Cooperative Agreement No. 58-6250-6-001 and the National Institutes of Health, NCRR General Clinical Research for Children Grant M01RR00188.
This work is a publication of the U.S. Department of Agriculture (USDA)/Agricultural Research Service (ARS) Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children's Hospital, Houston, TX. Contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. Funded in part by the Bristol-Myers Research Fund.
Rights and permissions
About this article
Cite this article
McDonald, M., Abrams, S. & Schanler, R. Iron Absorption and Red Blood Cell Incorporation in Premature Infants Fed an Iron-Fortified Infant Formula. Pediatr Res 44, 507–511 (1998). https://doi.org/10.1203/00006450-199810000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199810000-00007
This article is cited by
-
Physiological requirements for iron in women of reproductive age assessed by the stable isotope tracer technique
Nutrition & Metabolism (2019)
-
Iron physiological requirements in Chinese adults assessed by the stable isotope labeling technique
Nutrition & Metabolism (2018)
-
Dietary iron intake in the first 4 months of infancy and the development of type 1 diabetes: a pilot study
Diabetology & Metabolic Syndrome (2010)