Abstract
We examined the association between elevated concentrations of 25 blood proteins in blood spots collected on postnatal d 1, 7, and 14 from infants <28 wk gestation who survived to 24 mo and the risk of two patterns of early lung disease i.e. early and persistent pulmonary dysfunction (EPPD) and normal early pulmonary function followed by pulmonary deterioration (PD). Thirty-eight percent (n = 347) of our cohort had PD, and 43% (n = 383) had EPPD. On postnatal d 14, elevated concentrations of two proteins (RANTES and VEGF) were associated with reduced risk of PD. Similarly, the risk of EPPD was also reduced if three proteins had elevated concentrations on postnatal d 14 (RANTES, MMP-1, and VEGF). In contrast, the risk of EPPD was increased if on d 14 two proteins had elevated concentrations (IL-8 and ICAM-1). Inflammation might influence the risk of EPPD and PD or be a consequence of lung damage or therapies to minimize lung dysfunction.
Similar content being viewed by others
Main
Early pulmonary dysfunction in extremely low GA newborns (ELGANs; <28 wk gestation) can be characterized by three distinct patterns, based on the fraction of inspired oxygen (FiO2) they require in the first 2 postnatal wk (1). A minority of ELGANs have relatively normal pulmonary function throughout the first 2 postnatal wk (low FiO2). Another group has pulmonary deterioration (PD), characterized by resolution of their initial lung disease during the first week, and deterioration during the second postnatal week, resulting in the need for increased supplemental oxygen. A third group has early and persistent pulmonary dysfunction (EPPD) requiring treatment with high concentrations of supplemental oxygen throughout the first 2 postnatal wk.
We previously investigated the clinical risk factors for each pattern of respiratory dysfunction. Low GA, fetal growth restriction, and receipt of mechanical ventilation on postnatal d 7 were associated with both PD and EPPD in the ELGAN Study sample (1). Confirmed bacteremia, receipt of vitamin A and surfactant, and treatment of patent ductus arteriosus (PDA) were associated with an increased risk of EPPD. However, histologic chorioamnionitis and funisitis were not associated with either PD or EPPD.
In our large cohort of ELGANs, the risk of chronic lung disease (CLD) was lowest in children who had persistently low FiO2, intermediate in those who developed PD, and highest in children who had EPPD (1). In this cohort, the risk of CLD is associated with elevated blood concentrations during the first 2 postnatal wk of a variety of proteins integral to inflammation, including proinflammatory cytokines, adhesion molecules, and matrix metalloproteinases (2). Others have also found that inflammation probably plays a role in the development of CLD (3,4). These observations led us to hypothesize that systemic markers of inflammation, as manifested by blood concentrations of a variety of inflammatory proteins, would be elevated in the EPPD group and elevated to a lesser degree in the PD group compared with infants in the low FiO2 group.
METHODS
The ELGAN Study.
The infants included in this analysis are a subset of infants enrolled in a multicenter epidemiologic study to identify characteristics and exposures that increase the risk of structural and functional neurologic disorders in ELGANs (the ELGAN Study) (1,5,6). From March 2002 to August 2004, women delivering before the 28th wk of gestation at 1 of 14 participating institutions were asked to enroll in the study. Individual institutional review boards (including the University of North Carolina at Chapel Hill; see acknowledgments for full list of institutions) approved the enrollment and consent processes. The original consent and approval included the provision for secondary analyses of deidentified data. Therefore, separate approval was not necessary for the analyses reported in this article. The subset for this study included all infants enrolled in the ELGAN Study for whom sufficient information was available to determine an early respiratory group assignment, and measurements of proteins in a blood specimen were obtained during the first 2 postnatal wk. We limited our sample of newborns to the 908 who survived to 24 mo because protein measurements were available only for children who had a developmental assessment at 24 mo postterm equivalent. A full description of the methods is provided elsewhere (1,5–7). Here, we focus on those most relevant to the current study.
Newborn variables.
The GA estimates were based on a hierarchy of the quality of available information. Most desirable were estimates based on the dates of embryo retrieval or intrauterine insemination or fetal ultrasound before the 14th wk (62%). When these were not available, reliance was placed sequentially on a fetal ultrasound at 14 or more wk (29%), last menstrual period without fetal ultrasound (7%), and GA recorded in the log of the NICU (1%).
ELGANs were classified into three mutually exclusive groups: those with consistently low FiO2 (a FiO2 consistently <0.23 on all days between 3 and 7 postnatal d and receiving FiO2 ≤ 0.25 on d 14), those with PD (a FiO2 < 0.23 on any days between 3 and 7 d and receiving FiO2 > 0.25 on d 14), and those with EPPD (a FiO2 consistently ≥ 0.23 on all days between 3 and 7 postnatal d and receiving FiO2 > 0.25 on d 14) (1,6). For individual infants, the FiO2 assigned for each day of life was the mode FiO2 for that day.
Blood spot collection.
Drops of blood were collected on filter paper (Schleicher & Schuell 903, Keene, NH) after specimens were obtained for clinical indications between postnatal d 1–3, 5–8, and 12–15. Dried blood spots were stored at −70°C in sealed bags with desiccant until processed.
Elution of proteins from blood spots.
For protein elution, 12-mm punched biopsies of the frozen blood spots were submerged in 300 μL PBS containing 0.1% Triton ×100 (Sigma Chemical Co.-Aldrich, St. Louis, MO) and 0.03% Tween-20 (Fisher, Hampton, NH), vortexed for 30 s, and incubated on a shaker for 1 h at 4°C. The buffer and biopsy were then transferred over the filter of a SpinX tube (Corning Fisher), centrifuged at 2000 × g followed by collection of the filtered eluted blood. An additional wash of the punch was performed in 100 μL for a final elution volume of 400 μL.
Protein measurements.
The ELGAN Study was designed to identify antecedents of brain injury in ELGANs. Thus, all the proteins to be measured in the blood spots were chosen because of their potential to provide information about the risks and consequences of brain damage and because they could be measured with validity and reasonable precision. Blood spot collection, elution of proteins from blood spots, and the electrochemiluminescence protein-measurement procedures are described in detail elsewhere (8,9). The electrochemiluminescence system provides measurements comparable with those obtained with traditional ELISA (10,11). In addition, split quality control blood pools tested on each plate showed interassay variation of <20% for each protein.
We measured CRP (C-reactive protein), SAA (serum amyloid A), MPO (myeloperoxidase), IL-1β; IL-6; IL-6R; TNF-α; TNF-R1; TNF-R2; IL-8 (CXCL8); MCP-1 (monocyte chemoattractant protein-1; CCL2), MCP-4 (monocyte chemoattractant protein-4; CCL13), MIP-1B (macrophage inflammatory protein-1 β; CCL4), RANTES (regulated upon activation, normal T cell expressed, and secreted; CCL5), I-TAC (interferon-inducible T cell α-chemoattractant; CXCL11), ICAM-1 (CD54), ICAM-3 (CD50), VCAM-1 (vascular cell adhesion molecule-1; CD106), E-SEL (E-selectin; CD62E), MMP-1 (matrix metalloproteinase-1), MMP-9 (matrix metalloproteinase-9), VEGF, VEGF-R1, VEGF-R2, and IGFBP-1 (insulin growth factor binding protein-1).
Data analysis.
We evaluated the generalized null hypothesis that the occurrence of PD and EPPD are not associated with blood protein concentrations in the highest quartile for GA on the day the blood was collected. We began our analyses by exploring the frequency of each entity in the 4 quartiles of the concentration of each protein. Rarely was a linear trend seen. Thus, the analyses we present here compare children whose protein concentration was in the highest quartile with children whose protein concentration was in the lower 3 quartiles.
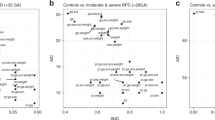
The risk of each pattern of respiratory disease entity associated with a protein concentration in the highest quartile is presented as an OR and the 99% CI. We selected this CI because we wanted to modify our analyses for multiple comparisons (25 proteins measured at 3 times) thereby avoiding a type I (false positive) error, while not appreciably increasing the risk of a type II (false negative) error (12). Because PD and EPPD are mutually exclusive, and each is appropriately compared with the same referent group (children in the low FiO2 group), we used multinomial logistic regression (13).
Because protein concentrations can be influenced by processes associated with earlier events, we created logistic regression models in which protein concentrations are temporally ordered, so that the earliest occurring protein concentrations are entered first and are not displaced by later protein concentrations (14–19). For these time-oriented risk models (TORMs), we categorize sets of protein concentrations by the day the blood spot was obtained. Each set is called an epoch and are labeled 1, 7, and 14, corresponding to the days on which blood spots were collected. Endogenous variables, GA at birth, and birth weight Z-score, were entered in epoch 1. We used a step-down procedure seeking a parsimonious solution without interaction terms.
RESULTS
Of the 1506 infants enrolled in the ELGAN Study, 1302 infants had information available to determine the respiratory pattern in the first 2 postnatal wk (Fig. 1). Of these, 908 survived to 24 mo, had proteins measured on one or more days, and were included in the analyses presented here. Among these infants, 19% (n = 172) were in the low FiO2 group, 38% (n = 347) were in the PD group, and 42% (n = 383) were in the EPPD group. Five percent of children in the low FiO2 group died before 24 mo, compared with 9% in the PD group and 16% in the EPPD group. CLD developed in 16% of children in the low FiO2, 51% of children in the PD group, and 70% of children in the EPPD group.
Multinomial analyses of risk of PD versus low FiO2.
Elevated concentrations of none of the 25 inflammation-related proteins that were measured were associated with increased risk of PD (Table 1). A decreased risk of PD was found if the newborn had elevated d 7 concentrations of RANTES (CCL5), VCAM-1 (CD106) or MMP-1, or elevated d-14 concentrations of RANTES (CCL5) or VEGF.
Multinomial analyses of risk of EPPD versus low FiO2.
A reduced risk of EPPD was found among infants with elevated d-1 concentrations of RANTES (CCL5), elevated d-7 concentrations of MIP-1β (CCL4) or VEGF, or elevated d-14 concentrations of IL-8 (CXCL8) or ICAM-1 (CD54; Table 1). An increased risk of EPPD was found among infants with elevated d-7 concentrations of MCP-1 (CCL2) and those with elevated d-14 concentrations of IL-8 (CXCL8) or ICAM-1 (CD54). RANTES was the only protein whose concentration seemed to be inversely related to EPPD risk on all days.
Time-oriented regression.
In time-oriented regression, PD was not associated with any d-1 protein elevations, but a reduced risk of PD was associated with an elevation of VCAM-1 in d-7 blood and with an elevation of VEGF in d-14 blood (Table 2). In the EPPD versus low FiO2 TORM (Table 2), elevated concentrations of RANTES on d 1 and 7 and of SAA on d 7 were associated with a decreased risk of EPPD. However, an elevated concentration of ICAM-1 on d 7 was associated with increased risk.
DISCUSSION
We examined the association between elevated concentrations of 25 blood proteins in the first 2 postnatal wk and the risk of EPPD and PD among extremely preterm infants. In light of evidence that pulmonary inflammation contributes to the occurrence of CLD (3,20), we hypothesized that systemic inflammation would be present in infants who developed EPPD, and to lesser degree in infants who developed PD.
Only a small amount of predictive information about PD and EPPD is available in blood spots collected on d 1, with increasing information on d 7, and even more on d 14. The number of inflammation-related proteins associated with EPPD increased with increasing postnatal age raising the possibility that systemic inflammation associated with lung dysfunction reflects postnatal phenomena. This is no surprise because infants who experience EPPD have such inflammation-promoting exposures as supplemental oxygen and mechanical ventilation, which are viewed as antecedents of CLD (21,22).
Elevations of inflammation-associated proteins provided more information about reduced risk of PD rather than increased risk. No protein concentration elevation on any of the 3 d was associated with increased risk of PD. In contrast, the elevated concentrations of three proteins on d 7 (RANTES, VCAM-1, and MMP-1) and two on d 14 (RANTES and VEGF) were associated with reduced risk. On one level, this is evidence that inflammation does not contribute substantially to the occurrence of PD. Our findings raise the possibility that inflammation protects. We are reluctant to accept this view just yet. Rather, we think our provocative findings need to be replicated and alternative explanations need to be considered.
RANTES has been described as pleiotropic (23). Some of the functions of this protein contribute to reducing inflammation (24,25). Consequently, our finding elevated concentrations of RANTES associated with reduced risk of EPPD and PD might be viewed as additional support for a modulation of preexisting inflammation not otherwise apparent to us. Low concentrations of RANTES in blood shortly after birth have also been associated with increased risk of BPD or death (3,4). Elevated concentrations of VEGF were associated with reduced risk of PD. Support for the hypothesis that low VEGF levels contribute to PD comes from the observation that VEGF preserves alveolar development, and that reduced concentrations of lung VEGF disrupt lung growth and vascular distributions within the lung (26,27).
As with PD, elevations of some inflammation-associated proteins, including RANTES and VEGF, are associated with a decreased risk of EPPD. However, in contrast to PD, elevations of some proteins are associated with an increased risk of EPPD. On d 14, elevated concentrations of two proteins (IL-8 and ICAM-1) were associated with increased risk of EPPD. The association with IL-8 is not surprising because of its proinflammatory properties. ICAM-1 is an adhesion molecule that mediates the adhesion of white blood cells to the vascular endothelium and is important for recruiting leukocytes to sites of inflammation. Higher concentrations of soluble ICAM-1 have been associated with poor outcomes in adults with acute lung injury (28).
Our findings are best interpreted in light of the current understanding of the biology of inflammation. Individual proteins are only a small part of a much larger process. Inflammation-related proteins are highly interrelated (29) and together seem to contribute to organ damage (30). As a result, each protein is best interpreted as representing the interlinked web of proteins indicating inflammation and possibly promoting lung damage or phenomena likely to reduce damage. An inflammatory stimulus alters the expression of more than a thousand genes, increasing the expression of hundreds of proteins, and decreasing the expression of hundreds of others (31). For example, when the expression of VCAM-1 is increased, so, too, is the expression of other markers of inflammation (32). Consequently, what we see is a very limited snapshot of what has preceded and/or accompanied the development of lung dysfunction.
Lung dysfunction can promote and/or exacerbate an inflammatory response. Hypercapnia promotes adhesion molecule expression in both inflammatory-stimulated human pulmonary microvascular endothelial cells and in an animal model of inflammatory-induced acute lung injury (33). This, and similar observations, suggest that some of the protein concentration changes we found might be a consequence, rather than an antecedent of lung dysfunction. Such a response might very well further contribute to lung dysfunction, as lung inflammation can promote more lung inflammation. Lung exposed to an inflammatory stimulus releases circulating mediators that induce liver vascular endothelial cells to activate NF-κB and to express ICAM-1 and VCAM-1 (34). In essence, a self-reinforcing loop is generated that promotes sustained inflammation, thereby increasing the risk of inflammation-induced damage.
We do not know to what extent protein concentrations in the blood are of pulmonary origin. It is possible that under certain circumstances proteins produced by cells in the lung remain in the lung compartment, whereas under other circumstances (e.g. intense or prolonged pulmonary inflammation), they enter the circulation. It is possible that infants with PD and EPPD have inflammatory processes that are more prominent in the lung than in the blood. That is, systemic inflammation is not a prominent component of early pulmonary dysfunction, and our examination of proteins in the blood may provide only a limited and biased view of the inflammatory processes associated with early pulmonary dysfunction. Analysis of inflammatory proteins from the epithelial lung fluid might help elucidate this possibility.
Our study has several strengths and limitations. We created TORMs to provide information about the relative significance of protein concentrations at critical postnatal ages. We included a large number of infants, making it unlikely that we have missed important associations because of lack of statistical power. We selected infants based on GA, not birth weight, to minimize confounding due to factors related to fetal growth restriction (35).
The weaknesses of our study are those of all observational studies. We do not know to what extent the protein reductions or elevations contributed to PD or EPPD, and to what extent the protein reductions or elevations are surrogates for other processes that might have influenced CLD risk. We did not include infants who died before 24 mo, and more infants died in the EPPD group and PD group than in the low FiO2 group. This might bias our results if infants died because of a systemic inflammatory process. In addition, we collected all of our data prospectively. Eluting material from blood spots is likely to include the intracellular contents of disrupted cells in the circulation. Thus, what we measured is probably the sum of proteins in the circulation, and proteins released from cells whose integrity was lost in the drying of the blood spots.
In conclusion, elevated concentrations of inflammation-associated proteins in the blood were associated with reduced risk of PD. A similar pattern was seen to a lesser extent among children who had EPPD, although elevated concentrations of other inflammation-related proteins were associated with increased risk. The lack of evidence of inflammation in the blood early in the neonatal period among children who had EPPD or PD suggests that systemic inflammation is not a process that begins in utero. Postnatal events or exposures are more likely to be the promoters of this phenomenon. Because of the strong association between EPPD and CLD, and to a lesser degree PD and CLD, targeted therapies designed to modulate specific elements of systemic inflammation may modify CLD risk.
Abbreviations
- CLD:
-
chronic lung disease
- ELGAN:
-
extremely low GA newborn
- EPPD:
-
early and persistent pulmonary dysfunction
- FiO2:
-
fraction of inspired oxygen
- MCP:
-
monocyte chemoattractant protein
- MIP:
-
macrophage inflammatory protein
- MMP:
-
matrix metalloproteinase
- PD:
-
pulmonary deterioration
- SAA:
-
serum amyloid A
- VCAM:
-
vascular cell adhesion molecule
References
Laughon M, Allred EN, Bose C, O'Shea TM, Van Marter LJ, Ehrenkranz RA, Leviton A 2009 Patterns of respiratory disease during the first 2 postnatal weeks in extremely premature infants. Pediatrics 123: 1124–1131
Bose C, Laughon M, Allred EN, Van Marter LJ, O'Shea TM, Ehrenkranz RA, Fichorova R, Leviton A, for the ELGAN Study Investigators 2011 Blood protein concentrations in the first two postnatal weeks that predict bronchopulmonary dysplasia among infants born before the 28th week of gestation. Pediatr Res 69: 347–353
Bose CL, Dammann CE, Laughon MM 2008 Bronchopulmonary dysplasia and inflammatory biomarkers in the premature neonate. Arch Dis Child Fetal Neonatal Ed 93: F455–F461
Ambalavanan N, Carlo WA, D'Angio CT, McDonald SA, Das A, Schendel D, Thorsen P, Higgins RD 2009 Cytokines associated with bronchopulmonary dysplasia or death in extremely low birth weight infants. Pediatrics 123: 1132–1141
Laughon M, Bose C, Allred E, O'Shea TM, Van Marter LJ, Bednarek F, Leviton A 2007 Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics 119: 273–280
Laughon M, Bose C, Allred EN, O'Shea TM, Ehrenkranz RA, Van Marter LJ, Leviton A 2011 Antecedents of chronic lung disease following three patterns of early respiratory disease in preterm infants. Arch Dis Child Fetal Neonatal Ed 96: F114–F120
O'Shea TM, Allred EN, Dammann O, Hirtz D, Kuban KC, Paneth N, Leviton A 2009 The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev 85: 719–725
Leviton A, Fichorova R, Yamamoto Y, Allred EN, Dammann O, Hecht J, Kuban K, McElrath T, O'Shea TM, Paneth N 2011 Inflammation-related proteins in the blood of extremely low gestational age newborns. The contribution of inflammation to the appearance of developmental regulation. Cytokine 53: 66–73
Hecht JL, Fichorova RN, Tang VF, Allred EN, McElrath TF, Leviton A 2011 Relationship between neonatal blood protein concentrations and placenta histologic characteristics in extremely low GA newborns. Pediatr Res 69: 68–73
Fichorova RN, Richardson-Harman N, Alfano M, Belec L, Carbonneil C, Chen S, Cosentino L, Curtis K, Dezzutti CS, Donoval B, Doncel GF, Donaghay M, Grivel JC, Guzman E, Hayes M, Herold B, Hillier S, Lackman-Smith C, Landay A, Margolis L, Mayer KH, Pasicznyk JM, Pallansch-Cokonis M, Poli G, Reichelderfer P, Roberts P, Rodriguez I, Saidi H, Sassi RR, Shattock R, Cummins JE Jr, 2008 Biological and technical variables affecting immunoassay recovery of cytokines from human serum and simulated vaginal fluid: a multicenter study. Anal Chem 80: 4741–4751
Fichorova RN, Trifonova RT, Gilbert RO, Costello CE, Hayes GR, Lucas JJ, Singh BN 2006 Trichomonas vaginalis lipophosphoglycan triggers a selective upregulation of cytokines by human female reproductive tract epithelial cells. Infect Immun 74: 5773–5779
Rothman KJ 1990 No adjustments are needed for multiple comparisons. Epidemiology 1: 43–46
Dubin N, Pasternack BS 1986 Risk assessment for case-control subgroups by polychotomous logistic regression. Am J Epidemiol 123: 1101–1117
Leviton A, Pagano M, Kuban KC, Krishnamoorthy KS, Sullivan KF, Allred EN 1991 The epidemiology of germinal matrix hemorrhage during the first half- day of life. Dev Med Child Neurol 33: 138–145
Leviton A, Kuban KC, Pagano M, Allred EN, Van Marter L 1993 Antenatal corticosteroids appear to reduce the risk of postnatal germinal matrix hemorrhage in intubated low birth weight newborns. Pediatrics 91: 1083–1088
Leviton A, Paneth N, Reuss ML, Susser M, Allred EN, Dammann O, Kuban K, Van Marter LJ, Pagano M 1999 Hypothyroxinemia of prematurity and the risk of cerebral white matter damage. J Pediatr 134: 706–711
Leviton A, Dammann O, Allred EN, Kuban K, Pagano M, Van Marter L, Paneth N, Reuss ML, Susser M 1999 Antenatal corticosteroids and cranial ultrasonographic abnormalities. Am J Obstet Gynecol 181: 1007–1017
Leviton A, Paneth N, Reuss ML, Susser M, Allred EN, Dammann O, Kuban K, Van Marter LJ, Pagano M, Hegyi T, Hiatt M, Sanocka U, Shahrivar F, Abiri M, DiSalvo D, Doubilet P, Kairam R, Kazam E, Kirpekar M, Rosenfeld D, Schonfeld S, Share J, Collins M, Genest D, Heller D, Shen-Schwarz S 1999 Maternal infection, fetal inflammatory response, and brain damage in very low birthweight infants. Pediatr Res 46: 566–575
Laptook AR, O'Shea TM, Shankaran S, Bhaskar B 2005 Adverse neurodevelopmental outcomes among extremely low birth weight infants with a normal head ultrasound: prevalence and antecedents. Pediatrics 115: 673–680
Speer CP 2009 Chorioamnionitis, postnatal factors and proinflammatory response in the pathogenetic sequence of bronchopulmonary dysplasia. Neonatology 95: 353–361
Hillman NH, Moss TJ, Kallapur SG, Bachurski C, Pillow JJ, Polglase GR, Nitsos I, Kramer BW, Jobe AH 2007 Brief, large tidal volume ventilation initiates lung injury and a systemic response in fetal sheep. Am J Respir Crit Care Med 176: 575–581
Johnson BH, Yi M, Masood A, Belcastro R, Li J, Shek S, Kantores C, Jankov RP, Tanswell AK 2009 A critical role for the IL-1 receptor in lung injury induced in neonatal rats by 60% O2. Pediatr Res 66: 260–265
Levy JA 2009 The unexpected pleiotropic activities of RANTES. J Immunol 182: 3945–3946
Gatt ME, Urieli-Shoval S, Preciado-Patt L, Fridkin M, Calco S, Azar Y, Matzner Y 1998 Effect of serum amyloid A on selected in vitro functions of isolated human neutrophils. J Lab Clin Med 132: 414–420
Shahrara S, Park CC, Temkin V, Jarvis JW, Volin MV, Pope RM 2006 RANTES modulates TLR4-induced cytokine secretion in human peripheral blood monocytes. J Immunol 177: 5077–5087
Bhatt AJ, Pryhuber GS, Huyck H, Watkins RH, Metlay LA, Maniscalco WM 2001 Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med 164: 1971–1980
Thébaud B, Ladha F, Michelakis ED, Sawicka M, Thurston G, Eaton F, Hashimoto K, Harry G, Haromy A, Korbutt G, Archer SL 2005 Vascular endothelial growth factor gene therapy increases survival, promotes lung angiogenesis, and prevents alveolar damage in hyperoxia-induced lung injury: evidence that angiogenesis participates in alveolarization. Circulation 112: 2477–2486
Calfee CS, Eisner MD, Parsons PE, Thompson BT, Conner ER Jr, Matthay MA, Ware LB 2009 Soluble intercellular adhesion molecule-1 and clinical outcomes in patients with acute lung injury. Intensive Care Med 35: 248–257
Sriskandan S, Altmann DM 2008 The immunology of sepsis. J Pathol 214: 211–223
Wang H, Ma S 2008 The cytokine storm and factors determining the sequence and severity of organ dysfunction in multiple organ dysfunction syndrome. Am J Emerg Med 26: 711–715
Zak DE, Aderem A 2009 Systems biology of innate immunity. Immunol Rev 227: 264–282
Haverslag R, Pasterkamp G, Hoefer IE 2008 Targeting adhesion molecules in cardiovascular disorders. Cardiovasc Hematol Disord Drug Targets 8: 252–260
Liu Y, Chacko BK, Ricksecker A, Shingarev R, Andrews E, Patel RP, Lang JD Jr, 2008 Modulatory effects of hypercapnia on in vitro and in vivo pulmonary endothelial-neutrophil adhesive responses during inflammation. Cytokine 44: 108–117
Markovic N, McCaig LA, Stephen J, Mizuguchi S, Veldhuizen RA, Lewis JF, Cepinskas G 2009 Mediators released from LPS-challenged lungs induce inflammatory responses in liver vascular endothelial cells and neutrophilic leukocytes. Am J Physiol Gastrointest Liver Physiol 297: G1066–G1076
Arnold CC, Kramer MS, Hobbs CA, McLean FH, Usher RH 1991 Very low birth weight: a problematic cohort for epidemiologic studies of very small or immature neonates. Am J Epidemiol 134: 604–613
Acknowledgements
The authors wish to acknowledge their ELGAN study colleagues:
Olaf Dammann, Tufts Medical Center, Boston MA; Bhavesh L. Shah, Baystate Medical Center, Springfield MA; Camilia Martin, Beth Israel Deaconess Medical Center, Boston MA; Robert Insoft, Brigham & Women's Hospital, Boston MA; Karl Kuban, Boston Medical Center, Boston, MA; Francis Bednarek, U Mass Memorial Health Center, Worcester, MA; John Fiascone, Tufts Medical Center, Boston MA; Richard Ehrenkranz, Yale-New Haven Children's Hospital, New Haven CT; T. Michael O'Shea, Wake Forest University/Baptist Medical Center, Winston-Salem NC; Stephen C. Engelke, University Health Systems of Eastern Carolina, Greenville NC; Carl Bose, The University of North Carolina, Chapel Hill NC; Mariel Poortenga, Ed Beaumont, DeVos Children's Hospital, Grand Rapids MI; Nigel Paneth, Sparrow Hospital, Lansing MI; Michael D. Schreiber, University of Chicago Hospital, Chicago IL; Daniel Batton, William Beaumont Hospital, Royal Oak MI; Greg Pavlov, Frontier Science and Technology Research Foundation, Amherst, NY, and our project officer, Deborah Hirtz.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Supported by a cooperative agreement with NINDS 5U01NS040069. Supported by the Thrasher Research Fund [C.B.].
Rights and permissions
About this article
Cite this article
Laughon, M., Bose, C., Allred, E. et al. Patterns of Blood Protein Concentrations of ELGANs Classified by Three Patterns of Respiratory Disease in the First 2 Postnatal Weeks. Pediatr Res 70, 292–296 (2011). https://doi.org/10.1203/PDR.0b013e3182274f35
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3182274f35
This article is cited by
-
When inflammation meets lung development—an update on the pathogenesis of bronchopulmonary dysplasia
Molecular and Cellular Pediatrics (2022)
-
Allogeneic administration of human umbilical cord-derived mesenchymal stem/stromal cells for bronchopulmonary dysplasia: preliminary outcomes in four Vietnamese infants
Journal of Translational Medicine (2020)
-
Kolonisation oder Infektion bei Früh- und Neugeborenen
Monatsschrift Kinderheilkunde (2014)