-
PDF
- Split View
-
Views
-
Cite
Cite
Marcella D. Walker, Donald J. McMahon, William B. Inabnet, Ronald M. Lazar, Ijeoma Brown, Susan Vardy, Felicia Cosman, Shonni J. Silverberg, Neuropsychological Features in Primary Hyperparathyroidism: A Prospective Study, The Journal of Clinical Endocrinology & Metabolism, Volume 94, Issue 6, 1 June 2009, Pages 1951–1958, https://doi.org/10.1210/jc.2008-2574
Close - Share Icon Share
Abstract
Context: Data regarding the presence, extent, and reversibility of psychological and cognitive features of primary hyperparathyroidism (PHPT) are conflicting.
Objective: This study evaluated psychological symptoms and cognitive function in PHPT.
Design: This is a case-control study in which symptoms and their improvement 6 months after surgical cure of PHPT were assessed.
Settings: The study was conducted in a university hospital metabolic bone disease unit and endocrine surgery practice.
Participants: Thirty-nine postmenopausal women with PHPT and 89 postmenopausal controls without PHPT participated in the study.
Intervention: Participants with PHPT underwent parathyroidectomy.
Outcome Measures: Measurements used in the study were: Beck Depression Inventory (BDI); State-Trait Anxiety Inventory, Form Y (STAI-Y); North American Adult Reading Test (NAART); Wechsler Memory Scale Logical Memory Test, Russell revision (LM); Buschke Selective Reminding Test (SRT); Rey Visual Design Learning Test (RVDLT); Booklet Category Test, Victoria revision (BCT); Rosen Target Detection Test (RTD); Wechsler Adult Intelligence Scale-Revised Digit Symbol Subtest (DSy); Wechsler Adult Intelligence Scale Digit Span Subtest (DSpan).
Results: At baseline, women with PHPT had significantly higher symptom scores for depression and anxiety than controls and worse performance on tests of verbal memory (LM and SRT) and nonverbal abstraction (BCT). Depressive symptoms, nonverbal abstraction, and some aspects of verbal memory (LM) improved after parathyroidectomy to the extent that scores in these domains were no longer different from controls. Baseline differences and postoperative improvement in cognitive measures were independent of anxiety and depressive symptoms and were not linearly associated with serum levels of calcium or PTH.
Conclusions: Mild PHPT is associated with cognitive features affecting verbal memory and nonverbal abstraction that improve after parathyroidectomy.
Classical primary hyperparathyroidism (PHPT) was a symptomatic disease with commonly recognized neurological, cognitive, and psychiatric manifestations (1, 2). Many patients with PHPT are now asymptomatic or report only nonspecific symptoms, including weakness, easy fatigability, depression, intellectual weariness, loss of initiative, anxiety, irritability, and sleep disturbance (3). Although these symptoms are concerning, they are difficult to quantify, and there is debate about whether they are directly attributable to the underlying disease. At the Third International Workshop on Asymptomatic Primary Hyperparathyroidism (4), studies on the psychological and cognitive features of PHPT were reviewed and were not considered to be an indication for parathyroidectomy (5). The workshop recognized inconsistencies in the abnormalities described, their association with the underlying disease, and the extent to which these features were reversible after parathyroidectomy.
A number of studies have attempted to delineate the psychological and cognitive features of PHPT and their resolution with surgical cure (6–24). Most have focused on psychological symptoms, such as depression, anxiety, or quality of life (QOL), rather than cognitive function such as logic, memory, abstraction, attention/concentration, and mental manipulation. Most have suggested that there are psychological features of the disease. A number of observational studies, some without control groups, report improved psychological symptoms or QOL with parathyroidectomy. Findings of the three randomized controlled trials (RCTs) of parathyroidectomy in mild PHPT were inconsistent; two found improved QOL after surgery (18, 25), whereas one did not (17).
A smaller number of studies have examined cognitive function in PHPT (6, 9, 12, 14, 15, 26–28). Explanations for the conflicting results from these studies include: small sample sizes; investigation of only one or two aspects of cognition, making generalization difficult; lack of control groups or validated measures in some studies; and failure to take into account demographic differences in others. Some studies monitored subjects shortly after parathyroidectomy, an experimental design that introduces biases due to nonspecific benefits of surgery. Finally, no studies examining cognitive function have assessed the influence of psychological symptoms upon cognition, which is critical because depression and anxiety are known to affect cognitive function (29).
Therefore, it remains unclear whether cognitive impairment is a feature of modern PHPT. The purpose of this study was: 1) to examine whether cognitive function is affected in mild PHPT using a battery of tests that measure many different facets of cognition; 2) to evaluate psychological symptoms to adjust for the potentially confounding effect of depression or anxiety on performance; 3) to assess improvement in measures with surgical cure; and 4) to explore relationships between cognitive function and biochemical indices of disease severity.
Subjects and Methods
This case-control study compared cognitive function and psychological symptoms between two groups of postmenopausal women: 1) those with PHPT who decided to undergo parathyroidectomy [because they either met 2002 surgical guidelines (30) or preferred surgery over observation, despite not meeting surgical indications]; and 2) normal controls. The prospective arm of the study assessed changes in these features after parathyroidectomy. All patients gave written, informed consent. Patients were paid for participation in the study and travel expenses. This study was approved by the Institutional Review Boards of Columbia University Medical Center and Helen Hayes Hospital.
Subjects
Subjects were female, at least 45 yr old, menopausal for at least 1 yr, and English speaking, and they were recruited at Columbia University College of Physicians and Surgeons hospitals. PHPT patients were referred from the Metabolic Bone Diseases and Endocrine Surgery Units at Columbia University Medical Center. Normal controls, recruited by newspaper advertisements, fliers, and direct mailing, were studied at Helen Hayes Hospital, West Haverstraw, New York. PHPT patients had hypercalcemia and an elevated or inappropriately normal PTH level. Exclusion criteria (to eliminate the potential confounding effects of sex, menopausal status, or significant comorbidities on study outcomes) included male sex, malignancy other than nonmelanoma skin cancer, alcoholism, significant liver or kidney disease, illnesses requiring more than 2 wk of corticosteroids per year, traumatic brain injury or neurosurgery, seizure disorders, untreated mood disorders, and use of medications known to affect mineral metabolism. Between September 2003 and December 2007, a total of 119 women with PHPT were screened for enrollment; 46 were eligible and agreed to participate. The 73 women with PHPT who declined participation were similar to those enrolled (mean ± sem): age, 64.3 ± 1.3 yr; 98.6% white (97.2% non-Hispanic, 2.8% Hispanic) and 1.4% black. Three women in the PHPT group never underwent parathyroidectomy, two were not cured, and two were lost to follow-up, leaving 39 evaluable cases. The control group included 89 subjects without PHPT.
The study was designed to have 80% power with 1% α-level to detect a between-group difference of 0.62 sd change in at least one of four test measures (Rosen Target Symbol, WAIS Logical Recall Immediate and Delayed, and total score on Beck Depression Inventory). Cases and controls were enrolled in a 1:2 ratio to improve the precision of the estimate of change in cognitive functioning.
Study design
The PHPT group was evaluated preoperatively with nine standardized, validated cognitive and psychological tests. A serum sample was collected for measurement of biochemistries. Demographic factors and information on comorbid conditions and clinical symptoms were assessed by history. The PHPT group was reevaluated using the same procedures 6 months postoperatively. This interval was chosen to obviate biases that might be due to the nonspecific benefits of surgery. The control group underwent testing with the same test battery at an identical interval.
Biochemical evaluation
Serum calcium, albumin, phosphate, blood urea nitrogen, creatinine, and alkaline phosphatase activity were measured with colorimetric or spectrophotometric methods. Intact PTH was measured by immunochemiluminometric assay (Scantibodies Laboratories, Inc., Santee, CA). Vitamin D metabolites were measured by RIA (DiaSorin, Inc., Stillwater, MN).
Cognitive and psychological testing
Testing, conducted by three individuals using identical procedures, lasted approximately 1.5 h. Test administrators were not blinded to disease state or time of testing. Psychological tests refer to those measuring depression [Beck Depression Inventory (BDI)] and anxiety [State-Trait Anxiety Inventory (STAI)], whereas the remainder of the tests measured cognitive function.
1. Estimated Intellectual Quotient (IQ)
The North American Adult Reading Test (NAART) provides an estimate of intellectual ability. Estimated full-scale IQ (FSIQ) scores are obtained: estimated FSIQ = 127.8 − (0.78) (NAART errors) (31, 32). The mean normal value (± sd) is 100 ± 15 (33).
2. Depression
The BDI (2nd ed.) is a 21-item depression severity scale for adults. Higher scores indicate more symptoms: 0–13 indicates no or minimal depression; 14–19, mild depression; 20–28, moderate depression; and 29–63, severe depression (34).
3. Anxiety
The STAI-Y (35) measures anxiety and consists of two 20-item scales measuring trait anxiety (anxiety proneness) and state anxiety (a current emotional condition). Mean raw values (± sd) for working adults, ages 50–69 yr, are 32.2 ± 8.7 for state anxiety and 31.8 ± 7.8 for trait anxiety.
4. Memory for contextually related material
The Wechsler Memory Scale Logical Memory Test, Russell revision (LM) requires examinees to repeat two brief, orally presented stories immediately and after a 30-min delay. Results indicate idea units recalled in the two stories (36). Immediate recall mean values (± sd) for individuals ages 50–59 and 60–69 are 23.6 ± 6.1 and 20.5 ± 6.4, respectively. Delayed recall mean values (± sd) for individuals ages 50–59 and 60–69 are 20.1 ± 6.5 and 17.3 ± 6.7, respectively (37).
5. Word list memory
The Buschke Selective Reminding Test (SRT) (38, 39) assesses recall and learning for a word list. Results indicate words correctly recalled over six trials (maximum = 72) and after a 30-min delay (maximum = 12).
6. Visual memory
The Rey Visual Design Learning Test (RVDLT) requires subjects to recall and draw visually presented geometric designs. Results are scored as the number of correctly reproduced designs during three learning trials (40).
7. Nonverbal abstraction
This was assessed with the Booklet Category Test, Victoria revision (BCT) (41), an 81-item version of the Halstead Category Test (HCT) (42), requiring examinees to infer the governing principle for sets of visual stimuli. Errors are summed, and full HCT performance is predicted: 4.335 + [1.839 × (Victoria Revision errors)] (43), then converted to a T-score adjusting for age, education, and gender (42). T-scores are interpreted as follows: 55 or higher, above average; 45–54, average; 40–44, below average; 35–39, mildly impaired; 30–34, mildly to moderately impaired; 25–29, moderately impaired; 20–24, moderately to severely impaired; and 19 or below, severely impaired.
8. Visual concentration/attention
The Rosen Target Detection Test (RTD) examines sustained visual concentration and attention. Examinees find a target among similar items. Results indicate time to completion and errors. The mean normal values (± sd) for the symbol version of the test and errors are 35.7 ± 8.4 and 3.8 ± 2.8, respectively. The Wechsler Adult Intelligence Scale-Revised Digit Symbol Subtest (DSy) (33) measures response speed and visual attention. Examinees fill in the blank squares with a nonsense symbol corresponding to a digit. Results are scored as symbols transcribed in 90 sec. Raw scores are converted to scaled scores, which adjusts for age differences. The mean scaled score (± sd) is 10 ± 3 (33).
9. Auditory attention and mental manipulation
The Wechsler Adult Intelligence Scale Digit Span Subtest (DSpan) tests immediate span of auditory attention and mental manipulation [mean scaled score (± sd) is 10 ± 3] (33).
Statistics
Differences between PHPT and control test performance at baseline and after 6 months were evaluated for each outcome with linear mixed models for repeated measures with fixed effects for group, time and their interaction, random effect of subjects, and an unstructured covariance structure. Model estimated means ± sem adjusted for covariates are reported. The method of simultaneous confidence limits was used to assess between-group differences at baseline or 6 months when the effects of group or the group-by-time interaction attained statistical significance, and again for within-group differences between times when the fixed effects of time or group-by-time interaction achieved statistical significance. Test scores were adjusted for age, education, and sex as suggested by the test manual when methods of adjustment were available. Because not all tests had methods of correction, all scores were additionally adjusted statistically for age, education, and estimated IQ. Scores were not adjusted for years since menopause due to its colinearity with age. Education level was coded as number of years of schooling completed. Cognitive measures were also evaluated with adjustment for levels of anxiety and depression to minimize the influence of affective factors on cognition. Linear associations between biochemical measures and cognitive and psychological test scores were assessed with Pearson correlation coefficients. For all analyses, a two-tailed P ≤ 0.05 was considered to indicate statistical significance. Statistical analysis was performed using SAS, version 9.1.3 (SAS Institute, Inc., Cary, NC).
Results
Clinical and biochemical results
Cases had biochemical evidence of PHPT (serum calcium, 10.6 ± 0.1 mg/dl; PTH, 77 ± 4 pg/ml; Table 1). At baseline, PHPT patients were slightly older (61.3 ± 1.0 vs. 55.6 ± 0.4 yr; P < 0.001) and were further from menopause (10.8 ± 1.1 vs. 5.7 ± 0.5 yr; P < 0.001) than controls. They were also better educated (16.5 ± 0.3 vs. 14.9 ± 0.3 yr; P = 0.001) and had a higher estimated IQ (116 ± 1 vs. 112 ± 1; P = 0.004). All participants were Caucasian. Most participants with PHPT were asymptomatic, but 23% had nephrolithiasis, and 21% were osteoporotic. Serum calcium was at least 1 mg/dl above the upper limit of normal in 33%. Mean time from diagnosis to surgery was 47 ± 11 months. Histological findings, adenoma number, and size were not specifically collected as part of this investigation, but only patients who were cured by parathyroidectomy, as assessed by postoperative PTH and calcium, were included (n = 39). Postoperatively, PTH and calcium levels normalized, serum phosphate and 25-hydroxyvitamin D increased, whereas serum 1,25-dihydroxyvitamin D and alkaline phosphatase activity decreased (Table 1).
Biochemical variables in PHPT group before and after surgery
| . | Normal range . | PHPT . | ||
|---|---|---|---|---|
| . | Before parathyroidectomy (mean ± sem) . | After parathyroidectomy (mean ± sem) . | Pre- vs. postoperative Pvalue . | |
| Serum calcium (mg/dl) | 8.5–10.2 | 10.6 ± 0.1 | 9.5 ± 0.1 | <0.001 |
| PTH (pg/ml) | 14.0–66.0 | 77 ± 4 | 38 ± 3 | <0.001 |
| Phosphate (mg/dl) | 2.5–4.3 | 2.7 ± 0.1 | 3.5 ± 0.1 | <0.001 |
| 25-hydroxyvitamin D (ng/dl) | 16–74 | 24.0 ± 1.2 | 28.9 ± 1.4 | 0.008 |
| 1,25-dihydroxyvitamin D (ng/dl) | 18–62 | 54 ± 4 | 42 ± 4 | 0.001 |
| Creatinine (mg/dl) | 0.5–0.9 | 0.78 ± 0.02 | 0.84 ± 0.03 | <0.001 |
| Albumin (g/dl) | 4.0–5.0 | 4.6 ± 0.04 | 4.5 ± 0.04 | 0.20 |
| Alkaline phosphatase (U/liter) | 33–96 | 75 ± 4 | 65 ± 3 | 0.001 |
| . | Normal range . | PHPT . | ||
|---|---|---|---|---|
| . | Before parathyroidectomy (mean ± sem) . | After parathyroidectomy (mean ± sem) . | Pre- vs. postoperative Pvalue . | |
| Serum calcium (mg/dl) | 8.5–10.2 | 10.6 ± 0.1 | 9.5 ± 0.1 | <0.001 |
| PTH (pg/ml) | 14.0–66.0 | 77 ± 4 | 38 ± 3 | <0.001 |
| Phosphate (mg/dl) | 2.5–4.3 | 2.7 ± 0.1 | 3.5 ± 0.1 | <0.001 |
| 25-hydroxyvitamin D (ng/dl) | 16–74 | 24.0 ± 1.2 | 28.9 ± 1.4 | 0.008 |
| 1,25-dihydroxyvitamin D (ng/dl) | 18–62 | 54 ± 4 | 42 ± 4 | 0.001 |
| Creatinine (mg/dl) | 0.5–0.9 | 0.78 ± 0.02 | 0.84 ± 0.03 | <0.001 |
| Albumin (g/dl) | 4.0–5.0 | 4.6 ± 0.04 | 4.5 ± 0.04 | 0.20 |
| Alkaline phosphatase (U/liter) | 33–96 | 75 ± 4 | 65 ± 3 | 0.001 |
Biochemical variables in PHPT group before and after surgery
| . | Normal range . | PHPT . | ||
|---|---|---|---|---|
| . | Before parathyroidectomy (mean ± sem) . | After parathyroidectomy (mean ± sem) . | Pre- vs. postoperative Pvalue . | |
| Serum calcium (mg/dl) | 8.5–10.2 | 10.6 ± 0.1 | 9.5 ± 0.1 | <0.001 |
| PTH (pg/ml) | 14.0–66.0 | 77 ± 4 | 38 ± 3 | <0.001 |
| Phosphate (mg/dl) | 2.5–4.3 | 2.7 ± 0.1 | 3.5 ± 0.1 | <0.001 |
| 25-hydroxyvitamin D (ng/dl) | 16–74 | 24.0 ± 1.2 | 28.9 ± 1.4 | 0.008 |
| 1,25-dihydroxyvitamin D (ng/dl) | 18–62 | 54 ± 4 | 42 ± 4 | 0.001 |
| Creatinine (mg/dl) | 0.5–0.9 | 0.78 ± 0.02 | 0.84 ± 0.03 | <0.001 |
| Albumin (g/dl) | 4.0–5.0 | 4.6 ± 0.04 | 4.5 ± 0.04 | 0.20 |
| Alkaline phosphatase (U/liter) | 33–96 | 75 ± 4 | 65 ± 3 | 0.001 |
| . | Normal range . | PHPT . | ||
|---|---|---|---|---|
| . | Before parathyroidectomy (mean ± sem) . | After parathyroidectomy (mean ± sem) . | Pre- vs. postoperative Pvalue . | |
| Serum calcium (mg/dl) | 8.5–10.2 | 10.6 ± 0.1 | 9.5 ± 0.1 | <0.001 |
| PTH (pg/ml) | 14.0–66.0 | 77 ± 4 | 38 ± 3 | <0.001 |
| Phosphate (mg/dl) | 2.5–4.3 | 2.7 ± 0.1 | 3.5 ± 0.1 | <0.001 |
| 25-hydroxyvitamin D (ng/dl) | 16–74 | 24.0 ± 1.2 | 28.9 ± 1.4 | 0.008 |
| 1,25-dihydroxyvitamin D (ng/dl) | 18–62 | 54 ± 4 | 42 ± 4 | 0.001 |
| Creatinine (mg/dl) | 0.5–0.9 | 0.78 ± 0.02 | 0.84 ± 0.03 | <0.001 |
| Albumin (g/dl) | 4.0–5.0 | 4.6 ± 0.04 | 4.5 ± 0.04 | 0.20 |
| Alkaline phosphatase (U/liter) | 33–96 | 75 ± 4 | 65 ± 3 | 0.001 |
Psychological function
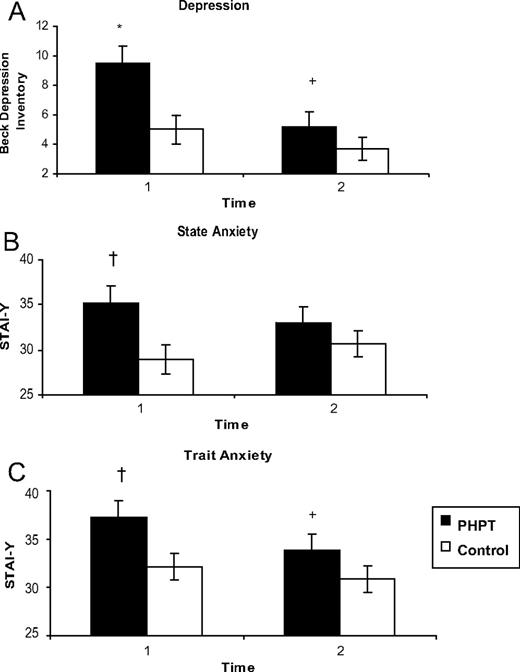
Patients with PHPT had more symptoms of depression (9.5 ± 1.2 vs. 5.0 ± 1.0; P = 0.006) and anxiety (state anxiety, 35.2 ± 1.9 vs. 29.0 ± 1.6; P = 0.017; trait anxiety, 37.3 ± 1.7 vs. 32.1 ± 1.4; P = 0.033) at baseline compared with controls (Fig. 1). Although these symptoms were more prominent in those with PHPT, mean performance levels on these tests were not in a range suggestive of clinical depression or anxiety. Depressive symptoms improved—the pattern of change in depressive symptoms over time differed between the groups (group by time interaction; P = 0.024) such that there was no difference between the control and postoperative groups (PHPT, 5.2 ± 1.0, vs. control, 3.7 ± 0.8; P = 0.28) after parathyroidectomy. Trait anxiety but not state anxiety decreased after parathyroidectomy in the PHPT group compared with baseline. However, there were no differences in change over time between the groups for either trait or state anxiety (P = 0.152 and P = 0.184, respectively).
A, Depression measured by BDI. B and C, State and trait anxiety as measured by STAI-Y. Higher scores indicate more symptoms. Scores are adjusted for age, IQ, and education. *, P < 0.01 compared with control group; †, P < 0.05 compared with control group; +, P < 0.01 compared with baseline. The test used to determine significance is the linear mixed model for repeated measures. Error bars represent 1 sem.
Cognitive function
Memory
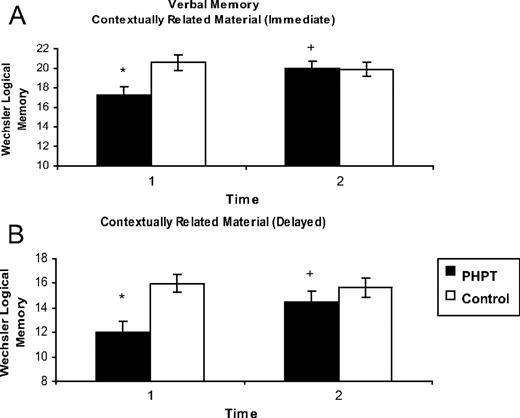
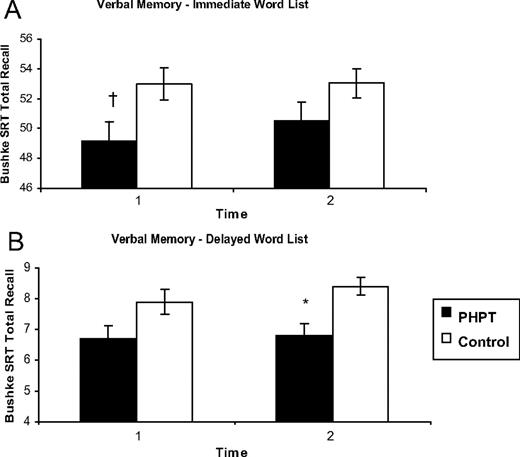
Those with PHPT had worse scores for both immediate and delayed recall of contextually related material (immediate, 17.2 ± 0.9 vs. 20.6 ± 0.8; P = 0.01; delayed, 12 ± 0.9 vs. 16.0 ± 0.7; P = 0.002; Fig. 2). Both tests improved to levels that were no longer different from control subjects after parathyroidectomy (immediate, 20.0 ± 0.8 vs. 20.0 ± 0.7; P = 0.97; delayed, 14.5 ± 0.9 vs. 15.7 ± 0.8; P = 0.36), and the change over time differed between normal and PHPT subjects (P = 0.003 immediate, and P = 0.009 delayed recall). Immediate, but not delayed, word list recall (SRT) was also worse at baseline in the PHPT group (immediate, 49.2 ± 1.3 vs. 53 ± 1.1; P = 0.04; delayed, 6.8 ± 0.4 vs. 7.9 ± 0.4; P = 0.064). Neither immediate nor delayed recall changed with surgery (Fig. 3). No differences were found between PHPT and controls in visual memory (Table 2). Both groups improved to a similar extent over time, consistent with a learning effect.
Memory for contextually related material (short story) at immediate (A) and delayed intervals (B). Higher scores indicate memory for more story elements. Scores are adjusted for age, IQ, education, anxiety, and depression. *, P ≤ 0.01 compared with control group; +, P < 0.01 compared with baseline. The test used to determine significance is the linear mixed model for repeated measures. Error bars represent 1 sem.
Memory for a word list at immediate (A) and delayed intervals (B). Higher scores indicate memory for more words. Scores are adjusted for age, IQ, education, anxiety, and depression. †, P ≤ 0.05 compared with control group; *, P < 0.01 compared with control group. P value = 0.064 for comparison of PHPT vs. control at baseline for delayed recall. The test used to determine significance is the linear mixed model for repeated measures. Error bars represent 1 sem.
Cognitive testing adjusted for age, IQ, education, anxiety, and depression
| Cognitive test . | PHPT group . | Control group . | PHPT vs. controls . | |||
|---|---|---|---|---|---|---|
| Time 1 (pre-op) . | Time 2 (post-op) . | Time 1 . | Time 2 . | Time 1 Pvalue . | Time 2 Pvalue . | |
| Visual memory | ||||||
| RVDLT total trials 1–3 | 16.6 ± 1.0 | 19.3 ± 0.9a | 17.3 ± 0.86 | 19.1 ± 0.8a | 0.639 | 0.886 |
| Response speed/visual concentration | ||||||
| Rosen Detection Test—symbol time | 43.0 ± 2.3 | 40.5 ± 1.9 | 40.6 ± 1.9 | 42.6 ± 1.7 | 0.440 | 0.465 |
| Rosen Detection Test—symbol error | 2.5 ± 0.5 | 3.2 ± 0.5 | 3.1 ± 0.4 | 2.9 ± 0.5 | 0.423 | 0.709 |
| WAIS-R Digit Symbol Standard Score | 13.0 ± 0.4 | 13.5 ± 0.4a | 13.3 ± 0.3 | 13.1 ± 0.3 | 0.662 | 0.406 |
| Auditory attention/mental manipulation | ||||||
| WAIS-R Digit Span Total Standard Score | 12.3 ± 0.4 | 12.0 ± 0.4 | 11.4 ± 0.3 | 11.7 ± 0.4 | 0.089 | 0.622 |
| Cognitive test . | PHPT group . | Control group . | PHPT vs. controls . | |||
|---|---|---|---|---|---|---|
| Time 1 (pre-op) . | Time 2 (post-op) . | Time 1 . | Time 2 . | Time 1 Pvalue . | Time 2 Pvalue . | |
| Visual memory | ||||||
| RVDLT total trials 1–3 | 16.6 ± 1.0 | 19.3 ± 0.9a | 17.3 ± 0.86 | 19.1 ± 0.8a | 0.639 | 0.886 |
| Response speed/visual concentration | ||||||
| Rosen Detection Test—symbol time | 43.0 ± 2.3 | 40.5 ± 1.9 | 40.6 ± 1.9 | 42.6 ± 1.7 | 0.440 | 0.465 |
| Rosen Detection Test—symbol error | 2.5 ± 0.5 | 3.2 ± 0.5 | 3.1 ± 0.4 | 2.9 ± 0.5 | 0.423 | 0.709 |
| WAIS-R Digit Symbol Standard Score | 13.0 ± 0.4 | 13.5 ± 0.4a | 13.3 ± 0.3 | 13.1 ± 0.3 | 0.662 | 0.406 |
| Auditory attention/mental manipulation | ||||||
| WAIS-R Digit Span Total Standard Score | 12.3 ± 0.4 | 12.0 ± 0.4 | 11.4 ± 0.3 | 11.7 ± 0.4 | 0.089 | 0.622 |
Data are expressed as mean ± sem. WAIS-R, Wechsler Adult Intelligence Scale-Revised.
P < 0.05 for comparison of time 1 to time 2.
Cognitive testing adjusted for age, IQ, education, anxiety, and depression
| Cognitive test . | PHPT group . | Control group . | PHPT vs. controls . | |||
|---|---|---|---|---|---|---|
| Time 1 (pre-op) . | Time 2 (post-op) . | Time 1 . | Time 2 . | Time 1 Pvalue . | Time 2 Pvalue . | |
| Visual memory | ||||||
| RVDLT total trials 1–3 | 16.6 ± 1.0 | 19.3 ± 0.9a | 17.3 ± 0.86 | 19.1 ± 0.8a | 0.639 | 0.886 |
| Response speed/visual concentration | ||||||
| Rosen Detection Test—symbol time | 43.0 ± 2.3 | 40.5 ± 1.9 | 40.6 ± 1.9 | 42.6 ± 1.7 | 0.440 | 0.465 |
| Rosen Detection Test—symbol error | 2.5 ± 0.5 | 3.2 ± 0.5 | 3.1 ± 0.4 | 2.9 ± 0.5 | 0.423 | 0.709 |
| WAIS-R Digit Symbol Standard Score | 13.0 ± 0.4 | 13.5 ± 0.4a | 13.3 ± 0.3 | 13.1 ± 0.3 | 0.662 | 0.406 |
| Auditory attention/mental manipulation | ||||||
| WAIS-R Digit Span Total Standard Score | 12.3 ± 0.4 | 12.0 ± 0.4 | 11.4 ± 0.3 | 11.7 ± 0.4 | 0.089 | 0.622 |
| Cognitive test . | PHPT group . | Control group . | PHPT vs. controls . | |||
|---|---|---|---|---|---|---|
| Time 1 (pre-op) . | Time 2 (post-op) . | Time 1 . | Time 2 . | Time 1 Pvalue . | Time 2 Pvalue . | |
| Visual memory | ||||||
| RVDLT total trials 1–3 | 16.6 ± 1.0 | 19.3 ± 0.9a | 17.3 ± 0.86 | 19.1 ± 0.8a | 0.639 | 0.886 |
| Response speed/visual concentration | ||||||
| Rosen Detection Test—symbol time | 43.0 ± 2.3 | 40.5 ± 1.9 | 40.6 ± 1.9 | 42.6 ± 1.7 | 0.440 | 0.465 |
| Rosen Detection Test—symbol error | 2.5 ± 0.5 | 3.2 ± 0.5 | 3.1 ± 0.4 | 2.9 ± 0.5 | 0.423 | 0.709 |
| WAIS-R Digit Symbol Standard Score | 13.0 ± 0.4 | 13.5 ± 0.4a | 13.3 ± 0.3 | 13.1 ± 0.3 | 0.662 | 0.406 |
| Auditory attention/mental manipulation | ||||||
| WAIS-R Digit Span Total Standard Score | 12.3 ± 0.4 | 12.0 ± 0.4 | 11.4 ± 0.3 | 11.7 ± 0.4 | 0.089 | 0.622 |
Data are expressed as mean ± sem. WAIS-R, Wechsler Adult Intelligence Scale-Revised.
P < 0.05 for comparison of time 1 to time 2.
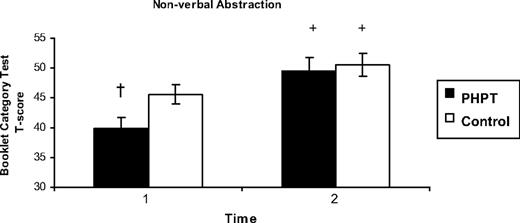
Other cognitive functions
Nonverbal abstraction was worse in the PHPT group (39.9 ± 1.9 vs. 45.6 ± 1.6; P = 0.041; Fig. 4). Although scores in both PHPT and control subjects improved over time, those with PHPT improved to a greater extent so that they were indistinguishable from normal subjects (49.5 ± 2.3 vs. 50.5 ± 1.9; P = 0.74; group by time interaction, P = 0.036). Visual concentration and attention as measured by the RTD or Wechsler Adult Intelligence Scale-Revised Digit Symbol Test was similar in the PHPT and control groups (Table 2). Although target detection did not change over time, the PHPT group improved compared with baseline on one test of visual concentration and attention (Digit Symbol test), whereas the control group did not (between groups change over time, P = 0.014). There was no difference on performance on the Wechsler Adult Intelligence Scale-Revised Digit Span Test of auditory attention and mental manipulation, and neither group improved compared with baseline (Table 2).
Nonverbal abstraction assessed by BCT. Higher scores indicate better performance. Scores are adjusted for age, IQ, education, anxiety, and depression. †, P < 0.05 compared with control group; +, P < 0.01 compared with baseline. The test used to determine significance is the linear mixed model for repeated measures. Error bars represent 1 sem.
Association of psychological and cognitive test results with disease severity
No linear associations were observed between any psychological or cognitive variable that was abnormal at baseline and serum calcium, PTH, or vitamin D metabolite concentration, nor was a relationship observed between changes in psychological or cognitive variables and change in biochemical measures.
Discussion
The nature and extent of psychological and cognitive involvement in PHPT remains an area of great interest. Although earlier studies have arbitrarily selected one or two aspects of cognitive function, this study used a wide array of tests because the facets of cognition that could be affected by PHPT were unclear a priori. We sought to document the presence of any abnormalities and to determine their reversibility and their relationship to ambient serum calcium, PTH, and other biochemical indices of the disease. A control population allowed for assessment of learning effects on repeated testing. The results of statistical analyses demonstrate that PHPT in postmenopausal women is associated with alterations in cognition that are independent of depression and anxiety. Those with PHPT performed less well than control subjects on some tests of cognitive function, including tests of verbal memory and nonverbal abstraction. Nonverbal abstraction and some aspects of verbal memory improved after parathyroidectomy. Visual memory and concentration and auditory attention and mental manipulation were not impaired. Finally, whereas patients with PHPT were not clinically depressed or anxious, they had more symptoms of depression and anxiety than control subjects. Depressive symptoms decreased after parathyroidectomy, whereas anxiety did not.
Many case-control studies (7, 11, 16, 22, 23) and a recent RCT (17) support the presence of psychological symptoms, including depression, anxiety, fearfulness, inferiority, lassitude, lack of initiative, fatigability, and apathy (11, 16, 23) or decreased QOL (7, 17, 22) in PHPT. Whereas observational studies have tended to show improvement of these symptoms with parathyroidectomy (7, 11, 13, 16, 19, 21, 22, 24), RCT results have been inconsistent (17, 25, 44). Rao et al. (44) found [using Short Form-36 (SF-36) and Symptom Checklist 90-revised (SCL-90R)] a worsening of social functioning and emotional problem domains in patients followed without intervention for 2 yr, although there was little improvement in the operative group. Those who had surgery, however, had a decline in anxiety and phobic symptoms. Bollerslev et al. (17) found significantly lower baseline QOL (SF-36) and more psychological symptoms, but did not demonstrate postoperative improvement. Ambrogini et al. (25) reported a modest benefit of surgery in four QOL domains (SF-36), including bodily pain, general health, vitality, and mental health but found no difference in SCL-90R measures. Possible explanations for the conflicting results of these studies could include differences in the size and composition of the populations sampled, type of analyses performed, or differential attrition in the studies. Our study specifically measured depression and anxiety because they are known confounders of neuropsychological testing. Together with the findings of the current report, the available results support the presence of some depressive and anxiety symptoms in PHPT.
Few other studies have examined cognitive function in PHPT. The clear learning effect over testing trials, as was evident in our investigation, limits the interpretation of studies without control groups (6, 14, 26, 45). Comparison of this report to the few existing controlled studies is difficult because each employed a different battery of tests, assessed individuals at different intervals from surgery, and included populations with varying calcium levels. Furthermore, no prior studies have adjusted for the presence of anxiety or depression symptoms. Numann et al. (12) used a large battery of tests and found postparathyroidectomy improvement in verbal memory as we did. Their positive findings despite a very small sample size (10 patients undergoing parathyroidectomy and 10 normocalcemic orthopedic controls) may be due to the more severe disease in their patients (12). Roman et al. (15) compared two tests of cognitive function in patients with PHPT and those with benign goiter preoperatively, 2, and 4 wk postoperatively. In contrast to our study, they did not find impaired memory for word lists compared with controls, but they did find changes in spatial learning and memory, which our study did not assess. Two other studies found no cognitive impairment in PHPT or postoperative improvement but may have been underpowered to do so (n = 14 and n = 20) (27, 28).
We found no linear association between serum calcium or PTH and cognitive abnormalities. This may be because the study had limited power to evaluate this relationship or because the range of serum calcium and PTH levels was too narrow to be able to discern the association. Studies in which the mean serum calcium values were much higher reported a relationship between preoperative neuropsychological symptoms and extent of hypercalcemia (19). Several studies from our group and others support the presence of increased vascular stiffness and endothelial dysfunction in PHPT (46–49). If present in the carotid or cerebral vasculature, vascular stiffness could represent a pathophysiological pathway leading to cognitive impairment.
The study has several limitations. First, the PHPT and control groups differed with regard to two important parameters: estimated IQ and education level. The direction of the differences (PHPT subjects were better educated and with a higher estimated IQ), however, should have biased against our finding of worse cognitive function in the PHPT group. Although these differences were taken into account in the statistical analysis, adjustment may not fully account for these disparities. It is therefore possible that, if cases could have been ideally matched, the results may have differed. Although specific socioeconomic data were not available, the communities from which the samples were obtained are similar in this regard. We also suspect an association between socioeconomic level and education, for which we adjusted.
There were also limitations inherent in the study design. An RCT of surgery vs. no surgery is a superior design compared with a case-control study but is extremely difficult to carry-out. Additionally, test administrators were not blinded to disease state and time of testing, which could have influenced results. Because we did not have a surgical control group, it is also possible that the preoperative increase in symptoms of anxiety and depression could be explained by anticipation of surgery. Improvement in psychiatric symptoms may have been due to the knowledge of being free of disease or a nonspecific effect of surgery rather than the correction of PHPT itself. However, if preoperative anxiety findings were related to impending surgery, an improvement would have been expected. Finally, we studied a convenience sample of PHPT patients including patients who did and did not meet 2002 criteria for surgery. The size of the cohort precludes a subgroup analysis (of those meeting vs. those not meeting indications for surgery) to address the issue of differing responses in these groups. However, it allowed us to achieve our main goal: to document the existence of cognitive symptoms among patients with mild PHPT.
The clinical significance of the cognitive improvement after surgery is unclear because the magnitude of changes was within 1 sd of the group mean. It is notable, however, that the mean value for nonverbal abstraction, logic, and problem solving was within one point of the mildly impaired range, a finding that was unexpected given participants’ high level of education. In addition, we do not know whether these results apply to premenopausal women and men with PHPT.
Despite these limitations, the study has several notable strengths. We characterized cognitive function in a moderate-sized group of patients with mild PHPT. Control data are available, and a large battery of validated tests, which evaluated many aspects of cognition, was used. Patients and controls were studied at two identical time points, obviating confounding by learning effects known to exist in cognitive testing. Additionally, we studied patients well after the immediate postoperative period to prevent biases due to the nonspecific benefits of surgery. Finally, we controlled for variables known to affect cognitive performance, including age, education, and estimated IQ, and the presence of anxiety and depressive symptoms.
We conclude that mild PHPT in postmenopausal women is associated with weaker performance in the cognitive domains of verbal memory and nonverbal abstraction. This is independent of anxiety and depressive symptoms, which are also more common in PHPT than in a control population. Parathyroidectomy leads to improvement in some of the psychiatric and cognitive deficits. Although these results cannot be extrapolated to predict clinical expectations in any given patient, they may provide an explanation for the improved sense of well-being reported by many, but not all, patients after successful parathyroidectomy. Furthermore, these results may be useful in further research into specific neuroanatomical regions that may be specifically affected by the hyperparathyroid process.
Acknowledgments
We are grateful to Dr. John Bilezikian for his counsel and support throughout this project.
This work was supported by National Institutes of Health Grants R01 DK32333, K24 DK74457, and UL1 RR024156.
Disclosure Summary: The authors have nothing to disclose.