Abstract
Background
Veteran populations have five times the incidence of hepatocellular carcinoma (HCC) compared with the general population. The incidence of HCC has increased in the Veteran’s Affairs Health System (VAHS), primarily due to the increased prevalence of cirrhosis. This study aimed to characterize differences in treatment patterns and overall survival rates across the five VAHS geographic regions.
Methods
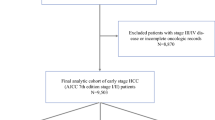
Using the VA Corporate Data Warehouse, the authors built a comprehensive national dataset of Veteran patients with HCC diagnosed between 2001 and 2015 to compare patients across VAHS regions. A multivariable Cox proportional hazards model was used to identify factors associated with 5-year all-cause mortality. Kaplan-Meier curves were used to visualize the patient survival function, and the log-rank test was applied to test statistical significance.
Results
This retrospective study analyzed 13,434 patients. The West region had the highest rate of overall treatment receipt (63.6%), and the Southwest had the lowest rate (52.9%). After adjustment for demographic, clinicopathologic, treatment, and hospital factors, treatment in a non-West region continued to be significantly associated with a 10% to 13% increased risk of 5-year mortality (Midwest: hazard ratio [HR], 1.11; 95% confidence interval [CI], 1.03–1.17; Northeast: HR, 1.10; 95% CI, 1.03–1.17; Southeast: HR, 1.13; 95% CI, 1.06–1.21; Southwest: HR, 1.11; 95% CI, 1.03–1.19) (p < 0.01).
Conclusions
Treatment patterns and overall survival rates of HCC patients differ significantly across VAHS geographic regions. Targeted interventions to increase the rate of treatment in the non-West regions are needed to improve survival of HCC Veterans and provide uniformly high-quality care across VAHS facilities.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–21.
Forner ALJ, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245–55.
Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology. 2015;149:1471–82.
Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing quality of care in veterans affairs and non-veterans affairs settings. J Gen Intern Med. 2018;33:1631–8.
Hanlon C, Huang C, Sloss E, et al. Comparing VA and non-VA quality of care: a systematic review. J Gen Intern Med. 2017;32:105–21.
Serper M, Taddei TH, Mehta R, et al. Association of provider specialty and multidisciplinary care with hepatocellular carcinoma treatment and mortality. Gastroenterology. 2017;152:1954–64.
Polanco PM, Ju MR, Chansard M, et al. Trends and disparities in treatment utilization for early-stage hepatocellular carcinoma in the veteran population. Ann Surg Oncol. 2022;29(9):5488–97. https://doi.org/10.1245/s10434-022-11897-3.
Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with non-alcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(124–131):e121.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Kaplan DE, Dai F, Aytaman A, et al. Development and performance of an algorithm to estimate the Child-Turcotte-Pugh score from a national electronic healthcare database. Clin Gastroenterol Hepatol. 2015;13(2333–41):e2331–6.
Kamath PS, Kim WR. Advanced liver disease study G: the Model for End-Stage Liver Disease (MELD). Hepatology. 2007;45:797–805.
Kwak J, Haley WE. Current research findings on end-of-life decision-making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–41.
Bruix J, Sherman M. American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
Cabibbo G, Enea M, Attanasio M, Bruix J, Craxi A, Camma C. A meta-analysis of survival rates of untreated patients in randomized clinical trials of hepatocellular carcinoma. Hepatology. 2010;51:1274–83.
Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology. 2009;49:453–9.
Benson AB III, Abrams TA, Ben-Josef E, et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. JNCCN J Natil Comp Cancer Netwk. 2009;7:350–91.
Yopp AC, Mansour JC, Beg MS, et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol. 2014;21:1287–95.
Chang TT, Sawhney R, Monto A, et al. Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. HPB Oxford. 2008;10:405–11.
Hyder O, Dodson RM, Nathan H, et al. Referral patterns and treatment choices for patients with hepatocellular carcinoma: a United States population-based study. J Am Coll Surg. 2013;217:896–906.
Davila JA, Kramer JR, Duan Z, et al. Referral and receipt of treatment for hepatocellular carcinoma in United States veterans: effect of patient and nonpatient factors. Hepatology. 2013;57:1858–68.
Ju M, Wang SC, Syed S, Agrawal D, Porembka MR. Multidisciplinary teams improve gastric cancer treatment efficiency at a large safety net hospital. Ann Surg Oncol. 2020;27:645–50.
Marshall CL, Petersen NJ, Naik AD, et al. Implementation of a regional virtual tumor board: a prospective study evaluating feasibility and provider acceptance. Telemed e-Health. 2014;20:705–11.
Shea CM, Teal R, Haynes-Maslow L, et al. Assessing the feasibility of a virtual tumor board program: a case study. J Healthcare Manage Am Coll Healthcare Exec. 2014;59:177.
Hede K. Teleoncology gaining acceptance with physicians, patients. Oxford: Oxford University Press; 2010.
Mair F, Whitten P, May C, Doolittle GC. Patient perceptions of a telemedicine specialty clinic. J Telemed Telecare. 2000;6:36–40.
Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: an acceptable telehealth model for rural patients and health workers. Intern Med J. 2012;42:780–5.
Salami AC, Barden GM, Castillo DL, et al. Establishment of a regional virtual tumor board program to improve the process of care for patients with hepatocellular carcinoma. J Oncol Pract. 2015;11:e66–74.
Sapisochin G, Bruix J. Liver transplantation for hepatocellular carcinoma: outcomes and novel surgical approaches. Nature Rev Gastroenterol Hepatol. 2017;14:203–17.
Adam R, Karam V, Delvart V, et al. Evolution of indications and results of liver transplantation in Europe: a report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57:675–88.
De Villa V, Lo CM. Liver transplantation for hepatocellular carcinoma in Asia. Oncologist. 2007;12:1321–31.
Santopaolo F, Lenci I, Milana M, Manzia TM, Baiocchi L. Liver transplantation for hepatocellular carcinoma: where do we stand? World J Gastroenterol. 2019;25:2591.
Acknowledgment
John D. Karalis was supported by a Physician-Scientist Institutional Award from the Burroughs Wellcome Fund (award no. 1018897). Work by Patricio M. Polanco was supported by the New Investigator Award Program of the North Texas VA Health Care System and the Eugene P. Frenkel, M.D. Scholar in Clinical Medicine Program of UT Southwestern.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ju, M.R., Karalis, J.D., Chansard, M. et al. Variation of Hepatocellular Carcinoma Treatment Patterns and Survival Across Geographic Regions in a Veteran Population. Ann Surg Oncol 29, 8413–8420 (2022). https://doi.org/10.1245/s10434-022-12390-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12390-7