Abstract
Background: Use of a long-acting inhaled bronchodilator, either an anticholinergic or a β-adrenergic receptor agonist (β-agonist), is recommended for maintenance treatment of chronic obstructive pulmonary disease (COPD). In COPD, the organ system most frequently requiring medical care, other than the respiratory system, is the cardiac system.
Objectives: To compare the risk of total mortality and certain respiratory and cardiac adverse events among users of the two types of recommended long-acting bronchodilators, we conducted a cohort study. Specifically, the study compared the safety of the only approved long-acting anticholinergic, tiotropium bromide, with the single-ingredient long-acting β-agonists (LABAs) salmeterol or formoterol in a broad population of users.
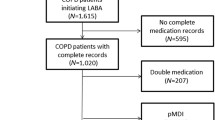
Methods: We used automated general practitioner data from the UK THIN (The Health Information Network) database as the data source for this study. We used Cox proportional hazards models to compute hazard ratio (HR) estimates and 95% CI controlling for propensity scores comprising various baseline demographic variables, medical therapies and illnesses.
Results: The 1061 tiotropium users and 1801 LABA users were similar with regard to risk of total mortality (HR 0.93; 95% CI 0.59, 1.44) and most cardiac events, including angina (HR 0.77; 95% CI 0.37, 1.59), atrial fibrillation or flutter (HR 0.60; 95% CI 0.25, 1.42), myocardial infarction (HR 1.29; 95% CI 0.45, 3.66) and tachycardia (HR 0.66; 95% CI 0.29, 1.51). Though imprecise, there was evidence of a decreased risk of heart failure (HR 0.65; 95% CI 0.37, 1.12) in tiotropium users. As regards respiratory endpoints, the risk of COPD exacerbation (HR 1.15; 95% CI 0.79, 1.67) and pneumonia (HR 1.11; 95% CI 0.38, 3.26) were similar among users of each type of drug, although there was a decreased risk of asthma exacerbation (HR 0.41; 95% CI 0.26, 0.64) in tiotropium users compared with LABA users.
Conclusions: Users of tiotropium and single-ingredient LABA had similar risk of total mortality and cardiovascular endpoints. The decreased risk of asthma exacerbations with tiotropium may be due to residual confounding by indication. Confidence limits for most events include reduced risks for tiotropium and also small increases in risk. Nevertheless, the point estimates suggest that tiotropium was associated with a lower risk of each cardiac event except myocardial infarction. However, the small number of cases means that further studies are needed to confirm these results.


Similar content being viewed by others
Notes
1The use of trade names is for product identification purposes only and does not imply endorsement.
References
Pauwels RA, Buist AS, Calverley PM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001; 163: 1256–76
Sin DD, Man P. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? Circulation 2003; 107(11): 1514–9
Disse B, Speck GA, Rominger KL, et al. Tiotropium (Spiriva): mechanistical considerations and clinical profile in obstructive lung disease. Life Sci 1999; 64: 457–64
Casaburi R, Kukafka D, Cooper CB, et al. Improvement in exercise tolerance with the combination of tiotropium and pulmonary rehabilitation in patients with COPD. Chest 2005; 127(3): 809–17
Niewoehner DE, Rice K, Cote C, et al. Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, 1160 a once-daily inhaled anticholinergic bronchodilator: a randomized trial. Ann Intern Med 2005; 143(5): 317–26
Maltais F, Hamilton A, Marciniuk D, et al. Improvements in symptom-limited exercise performance over 8 hours with once-daily tiotropium in patients with COPD. Chest 2005; 128(3): 1168–78
Kesten S, Jara M, Wentworth C, et al. Pooled clinical trial analysis of tiotropium safety. Chest 2006; 130: 1695–703
Morganroth J, Golisch W, Kesten S. Lack of cardiac safety signals in COPD patients receiving tiotropium as defined by electrocardiographic monitoring in placebo controlled trials. J COPD 2004; 1: 181–90
Covelli H, Bhattacharya S, Cassino C, et al. Absence of electrocardiographic findings and improved function with daily tiotropium in patients with chronic obstructive pulmonary disease. Pharmacotherapy 2005; 25: 1708–18
Currie GP, Lipworth BJ. ABC of chronic obstructive pulmonary disease: pharmacologic management-inhaled treatment. BMJ 2006; 332: 1439–41
Nelson HS, Weiss ST, Bleecker ER, et al. The salmeterol multicenter asthma research trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129: 15–26
GlaxoSmithKline. Serevent® product information, RL-2033. Research Triangle Park (NC): GlaxoSmithKline, 2003Aug
Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care 2004; 12: 171–7
Lewis JD, Schinnar R, Bilder WB, et al. Validation studies of The Health Improvement Network (THIN) database for Pharmacoepidemiology research. Pharmacoepidemiol Drug Saf 2007; 16: 393–401
Oracle9i database. Redwood Shores (CA): Oracle Corporation, 2000
STATA 7.0. College Station (TX): StataCorp, 2002
CDC. Chronic obstructive pulmonary disease surveillance: United States, 1971–2000 [online]. Available from URL: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5106a1.htm [Accessed 2006 May 12]
CDC. Surveillance for asthma: United States, 1980–1999 [online]. Available from URL: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5101a1.htm [Accessed 2006 May 12]
Braitman LE, Rosenbaum PR. Rare outcomes, common treatments: analytic strategies using propensity scores. Ann Intern Med 2002; 137: 693–6
Joffe MM, Rosenbaum PR. Invited commentary: propensity scores. Am J Epidemiol 1999, 333
Robins JM, Mark SD, Newey WK. Estimating exposure effects by modelling the expectations of exposure conditional on confounders. Biometrics 1992; 48: 479–95
Rubin DB. On principles for modeling propensity scores in medical research. Pharmacoepidemiol Drug Saf 2005; 13: 855–7
Rothman KJ, Greenland S. Approaches to statistical analysis. In: Rothman KJ, Greenland S, editors. Modern epidemiology. 2nd ed. Philadelphia (PA): Lippincott-Raven Publishers, 1998: 183–99
SensTool.xls from the Boston University School of Public Health [online]. Available from URL: http://www.bu.edu/dbin/sph/departments/epidemiology/epidemiologic_method-s_research.php [Accessed 2006 Feb 8]
Fox MP, Lash TL, Greenland S. A method to automate probabilistic sensitivity analyses of misclassified binary variables. Int J Epidemiol 2005; 34: 1370–6
Garcia Rodriguez LA, Pérez-Gutthann S, Jick S. The UK General Practice Research Database. In: Strom BL, editor. Pharmacoepidemiology. 3rd ed. New York: John Wiley & Sons, Ltd, 2000: 375–85
Curkendall SM, DeLuise C, Jones JK, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada: cardiovascular disease in COPD patients. Ann Epidemiol 2006; 16: 63–70
Donohue JF, van Noord JA, Bateman ED, et al. A 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterol. Chest 2002; 122: 47–55
Brusasco V, Hodder R, Miravitlles M, et al. Health outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPD. Thorax 2003; 58: 399–404
Mintzer J, Burns A. Anticholinergic side-effects of drugs in elderly people. J R Soc Med 2000; 93: 457–62
Costello R. Pharmacology. In: Calverly PMA, MacNee W, Pride NB, et al., editors. Chronic obstructive pulmonary disease. 2nd ed. London: Arnold, 2003: 341–56
Sovani MP, Whale CI, Tattersfield AE. A benefit-risk assessment of inhaled long-acting β2-agonists in the management of obstructive pulmonary disease. Drug Saf 2004; 27(10): 689–715
Ferguson GT, Funck-Brentano C, Fisher T, et al. Cardiovascular safety of salmeterol in COPD. Chest 2003; 123: 1817–24
Cepeda MS, Boston R, Farrar JT, et al. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol 2003; 158: 280–7
Cazzola M, Imperatore F, Salzillo A, et al. Cardiac effects of formoterol and salmeterol in patients suffering from COPD with preexisting cardiac arrhythmias and hypoxemia. Chest 1998; 114: 411–5
Acknowledgements
This study was funded by Boehringer Ingelheim Pharmaceuticals Incorporated. Michele Jara, Steven Kesten and Stephan F. Lanes are employees of Boehringer Ingelheim. Charles Wentworth III and Corey May are consultants for Boehringer Ingelheim. The authors were responsible for all aspects of this study, including design, analysis and interpretation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jara, M., Lanes, S.F., Wentworth, C. et al. Comparative Safety of Long-Acting Inhaled Bronchodilators. Drug-Safety 30, 1151–1160 (2007). https://doi.org/10.2165/00002018-200730120-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200730120-00007