Abstract
Objective: To describe associations between the use of benzodiazepines or related drugs (BZDs/RDs) and health, functional abilities and cognitive function in the elderly.
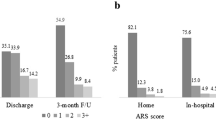
Methods: A non-randomised clinical study of patients aged ≥65 years admitted to acute hospital wards during 1 month. 164 patients (mean age ± standard deviation [SD] 81.6 ± 6.8 years) were admitted. Of these, nearly half (n = 78) had used BZDs/RDs before admission, and the remainder (n = 86) were non-users. Cognitive ability was assessed by the Mini-Mental State Examination (MMSE). Patients scoring ≥20 MMSE sum points were interviewed (n = 79) and questioned regarding symptoms and functional abilities during the week prior to admission. Data on use of BZDs/RDs before admission, current medications and discharge diagnoses were collected from medical records. Health, physical abilities and cognitive function were compared between BZD/RD users and non-users, and adjustments were made for confounding variables. The residual serum concentrations of oxazepam, temazepam and zopiclone were analysed.
Results: The mean ± SD duration of BZD/RD use was 7 ± 7 years (range 1–31). Two or three BZDs/RDs were concomitantly taken by 26% of users (n = 20). Long-term use of these drugs was associated with female sex and use of a higher number of drugs with effects on the CNS, which tended to be related to diagnosed dementia. After adjustment for these variables as confounders, use of BZDs/RDs was not associated with cognitive function as measured by the MMSE. However, use of BZDs/RDs was associated with dizziness, inability to sleep after awaking at night and tiredness in the mornings during the week prior to admission and with stronger depressive symptoms measured at the beginning of the hospital stay. Use of BZDs/RDs tended to be associated with a reduced ability to walk and shorter night-time sleep during the week prior to admission. A higher residual serum concentration of temazepam correlated with a lower MMSE sum score after adjustment for confounding variables.
Conclusions: Long-term use and concomitant use of more than one BZD/RD were common in elderly patients hospitalised because of acute illnesses. Long-term use was associated with daytime and night-time symptoms indicative of poorer health and potentially caused by the adverse effects of these drugs.









Similar content being viewed by others
References
Neutel CI, Perry S, Maxwell C. Medication use and risk of falls. Pharmacoepidemiol Drug Saf 2002; 11(2): 97–104
Barker MJ, Greenwood KM, Jackson M, et al. Cognitive effects of long-term benzodiazepine use: a meta-analysis. CNS Drugs 2004; 18(1): 37–48
Linjakumpu T, Hartikainen S, Klaukka T, et al. Psychotropics among the home-dwelling elderly: increasing trends. Int J Geriatr Psychiatry 2002; 17(9): 874–83
Paakkari P, Voipio T. The growing consumption of hypnotics and sedatives evens out. TABU (drug information from the National Agency for Medicines, Finland) 2005; (3): 37–8
Ohayon MM, Caulet M, Priest RG, et al. Psychotropic medication consumption patterns in the UK general population. J Clin Epidemiol 1998; 51(3): 273–83
Ohayon MM, Lader MH. Use of psychotropic medication in the general population of France, Germany, Italy, and the United Kingdom. J Clin Psychiatry 2002; 63(9): 817–25
Vermeeren A. Residual effects of hypnotics: epidemiology and clinical implications. CNS Drugs 2004; 18(5): 297–328
Barker MJ, Greenwood KM, Jackson M, et al. Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: a meta-analysis. Arch Clin Neuropsychol 2004; 19(3): 437–54
Poyares D, Guilleminault C, Ohayon MM, et al. Chronic benzodiazepine usage and withdrawal in insomnia patients. J Psychiatr Res 2004; 38(3): 327–34
Glass J, Lanctot KL, Herrmann N, et al. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005; 331(7526): 1169–76
National Agency for Medicines. Drug consumption statistics [online]. Available from URL: http://www.nam.fi/english/medicines/drug_consumption/index.html [Accessed 2006 Dec 15]
National Agency of Medicines. Classification of medicines (ATC) and defined daily doses (DDD) 2004. Helsinki: National Agency of Medicines, 2004
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12(3): 189–98
Salokangas RK, Stengard E, Poutanen O. DEPS: a new tool in screening for depression. Duodecim 1994; 110(12): 1141–8
World Health Organization. Tautiluokitus ICD-10 (Classification of Diseases ICD-10). Rauma: Kirjapaino Oy West Point, 1995
Laakkonen UM, Heiskanen A. Screening and quantitation of benzodiazepines in serum samples. In: Kaempe B, editor. T.I.A.F.T., proceedings of the 29th international meeting. Copenhagen: Mackeenzie, 1991: 262–6
Byles JE, Mishra GD, Harris MA, et al. The problems of sleep for older women: changes in health outcomes. Age Ageing 2003; 32(2): 154–63
Christer GM, Hublin CGM, Partinen MM. The extent and impact of insomnia as a public health problem. Prim Care Companion J Clin Psychiatry 2002; 4Suppl. 1: 8–12
Nielsen GH, Nordhus JH, Kvale G. Clinical geropsychology. In: Nordhus JH, Vandenbos GR, Berg S, et al., editors. Insomnia in older adults. Washington, DC: American Psychiatric Association, 1998: 167–75
Morgan K. Sleep problems in the elderly. In: Woods RT, editor. Handbook of the clinical psychology of ageing. Chichester: John Wiley & Sons, 1996: 303–14
Neubauer DN. Sleep problems in the elderly. Am Fam Physician 1999; 59(9): 2551–8, 2559–60
Socialstyrelsen/National Board of Social Welfare, Sweden. Indikatorer för utvärdering av kvaliteten i äldres läkemedelsterapia [indicators for evaluating the quality of medication therapy in the aged]. Stockholm: Socialstyrelsen/National Board of Social Welfare, Sweden, 2003: report no. 2003-110-20
Acknowledgements
This study was economically supported by grants from the Nordic Red Feather Campaign by the Finnish Lions Association, a Härkätie Health Center Grant and Turku University Hospital Grant EVO13390. The financial sponsors played no role in the design, execution, analysis or interpretation of data or writing of the study.
The authors thank Teemu Kemppainen BBA for his contribution as a computer designer to management of the data and coding the SAS queries, Ritva Kultalahti, Selena Nitecki, Pia Rytkölä and Mervi Strömberg for their contributions as research assistants and Mike Nelson MEd, PhD for proofreading and checking the grammar of the final manuscript. The personnel in the wards of Pori City Hospital kindly assisted in collection of the data.
JP has lectured in further education courses for physicians, nurses and physiotherapists sponsored by Janssen-Cilag, Lundbeck and Novartis. JN, MK and TV have no conflicts of interest that are directly relevant to the content of this study. KL is a medical director and partner in Medifront Ltd and has lectured in further education courses sponsored by AstraZeneca, Lundbeck, Merck Sharp & Dohme, Novartis and ratiopharm. S-LK has given lectures in further education courses for physicians, nurses and physiotherapists sponsored by Janssen-Cilag, Pfizer and Novartis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puustinen, J., Nurminen, J., Kukola, M. et al. Associations between Use of Benzodiazepines or Related Drugs and Health, Physical Abilities and Cognitive Function. Drugs Aging 24, 1045–1059 (2007). https://doi.org/10.2165/00002512-200724120-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200724120-00007