Abstract
Objective
To compare medication treatment patterns for patients with schizophrenia following initiation on olanzapine versus risperidone.
Methods
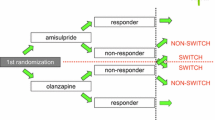
Retrospective analysis of a large, geographically diverse claims database of insured individuals identified 670 enrollees who: (1) were diagnosed with schizophrenia; (2) were initiated on olanzapine (n = 423) or risperidone (n = 247) monotherapy, and (3) had not been treated with olanzapine or risperidone during 1 year prior to initiation. Multivariate analyses were used to compare olanzapine and risperidone groups on treatment duration, the likelihood of receiving medication for at least 80% of days in the year post-initiation, the likelihood of receiving concomitant anti-Parkinsonian agents, and the likelihood of switching between medications of interest, by controlling for demographics, co-morbidities, and previous medication-use patterns.
Results
Compared with risperidone patients (mean dosage = 3.32 mg/day), patients treated with olanzapine (mean dosage = 10.45 mg/day) experienced a 29.4% increase in treatment duration (162 vs 213 days; p<0.0001), and a significantly higher probability of receiving medication for at least 80% of days in the year post-initiation (Odds Ratio [OR] = 2.057, p = 0.0002). Patients initiated on olanzapine versus risperidone were also found to be significantly less likely to use anti-Parkinsonian medications (OR = 0.639; p = 0.0284) and were significantly less likely to switch to risperidone than vice versa (OR = 0.275; p<0.0001).
Conclusions
Compared with risperidone, patients initiated on olanzapine experienced more favourable medication-use patterns. Olanzapine patients had a significantly longer duration of pharmacotherapy, a significantly higher likelihood of receiving medication treatment for at least 80% of days in the year post-initiation, a significantly lower likelihood of concomitant use of anti-Parkinsonian agents, and a significantly lower probability of switching between medications of interest than risperidone patients. Findings that patients initiated on olanzapine had more favourable medication treatment patterns have important clinical and economic implications. Interruptions in antipsychotic therapy have been previously linked to increases in psychotic symptoms and increased use of costly acute-care services.



Similar content being viewed by others
References
Rice DP, Miller LS. The economic burden of schizophrenia: conceptual and methodological issues, and cost estimates. In: Moscarelli M, Rupp A, Sartorius N, editors. Handbook of mental health economics and health policy. Schizophrenia 1996; I: 321–34
Wyatt RJ, Henter I, Leary MC, et al. An economic evaluation of schizophrenia: 1991. Soc Psychiatry Psychiatr Epidemiol 1995; 30(5): 196–205
De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res 2001; 47(2–3): 127–34
Mueser KT, Webb C, Pfeiffer M, et al. Family burden of schizophrenia and bipolar disorder: perceptions of relatives and professionals. Psychiatr Serv 1996; 47(5): 507–11
McCombs JS, Nichol MB, Stimmel GL, et al. Use patterns for antipsychotic medications in medicaid patients with schizophrenia. J Clin Psychiatry 1999; 60 Suppl. 19: 5–11; discussion 12-3
Soumerai SB, McLaughlin TJ, Ross-Degnan D, et al. Effects of limiting Medicaid drug-reimbursement benefits on the use of psychotropic agents and acute mental health services by patients with schizophrenia. N Engl J Med 1994; 331(10): 650–5
Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv 2001; 52(6): 805–11
Naber D, Moritz S, Lambert M, et al. Improvement of schizophrenic patients’ subjective well-being under atypical anti-psychotic drugs. Schizophr Res 2001; 50(1–2): 79–88
Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull 1995; 21(3): 419–29
Olfson M, Mechanic D, Hansell S, et al. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatr Serv 2000; 51(2): 216–22
Weiden P, Rapkin B, Mott T, et al. Rating of medication influences (ROMI) scale in schizophrenia. Schizophr Bull 1994; 20(2): 297–310
Cramer JA, Rosenheck R. Compliance with medication regimens for mental and physical disorders. Psychiatr Serv 1998; 49(2): 196–201
Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull 1997; 23(4): 637–51
Lindstrom E, Bingefors K. Patient compliance with drug therapy in schizophrenia: economic and clinical issues. Pharmacoeconomics 2000; 18(2): 105–24
Ruscher S, de Wit R, Mazmanian D. Psychiatric patients’ attitudes about medication and factors affecting noncompliance. Psychiatr Serv 1997; 48(1): 82–5
Hermann RC, Yang DW, Ettner SL, et al. Prescription of antipsychotic drugs by office-based physicians in the United States, 1989–1997. Psychiatr Serv 2002; 53(4): 425–30
Ashcroft D, Frischer M, Lockett J, et al. Variations in prescribing atypical antipsychotic drugs in primary care: cross-sectional study. Pharmacoepidemiol Drug Saf 2002; 11: 1–5
Owen R, Feng W, Thrush C, et al. Variations in prescribing practices for novel antipsychotic medications among veterans affairs hospitals. Psychiatr Serv 2001; 52(11): 1523–5
Sauriol L, Laporta M, Edwardes MD, et al. Meta-analysis comparing newer antipsychotic drugs for the treatment of schizophrenia: evaluating the indirect approach. Clin Ther 2001; 23(6): 942–56
Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol 1997; 17(5): 407–18
Purdon S. Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. Arch Gen Psychiatry 2000; 57: 259–8
Conley RR, Mahmoud R. A randomized double-blind study of risperidone and olanzapine in the treatment of schizophrenia or schizoaffective disorder. Am J Psychiatry 2001; 158(5): 765–74
Schillevoort I, de Boer A, Herings R, et al. Risk of extra-pyramidal syndromes with haloperidol, risperidone, or olanzapine. Ann Pharmacother 2001; 351: 517–22
Ayuso-Gutierrez JL, del Rio Vega JM. Factors influencing relapse in the long-term course of schizophrenia. Schizophr Res 1997; 28(2–3): 199–206
Revicki D, Brown R, Keller M, et al. Cost-effectiveness of newer antidepressants compared with tricyclic antidepressants in managed care settings. J Clin Psychiatry 1997; 58: 47–58
Clark W, Churchill D, Forwell L, et al. To pay or not to pay? CMAJ 2000; 162: 195–8
Marder SR. Facilitating compliance with antipsychotic medication. J Clin Psychiatry 1998; 59 Suppl. 3: 21–5
McCombs JS, Nichol MB, Johnstone BM, et al. Antipsychotic drug use patterns and the cost of treating schizophrenia. Psychiatr Serv 2000; 51(4): 525–7
Weiden PJ, Aquila R, Dalheim L, et al. Switching antipsychotic medications. J Clin Psychiatry 1997; 58 Suppl. 10: 63–72
Williams CL, Johnstone BM, Kesterson JG, et al. Evaluation of antipsychotic and concomitant medication use patterns in patients with schizophrenia. Med Care 1999; 37 (4 Suppl Lilly): AS81–6
Whitworth AB, Fleischhacker WW. Adverse events of antipsychotic drugs. Int Clin Psychopharmacol 1995; 9(5): 21–7
Fleischhacker WW, Meise U, Günther V, et al. Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatr Scand 1994; 89( Suppl. 382): 11–5
Gerlach J. The continuing problem of extrapyramidal symptoms: strategies for avoidance and effective treatment. J Clin Psychiatry 1999; 60 Suppl. 23: 20–4
Acknowledgements
Eli Lilly and Company provided financial support for this study. This manuscript was based on a presentation presented at the American Psychiatric Association’s 53rd Institute on Psychiatric Services, 10–14 October 2001, Orlando, Florida, and ISPOR 7th Annual International Meeting, 19-22 May 2002, Arlington, Virginia, USA.
The authors would like to thank Danielle Loosbrock and Beth Reeves for their editorial contributions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhao, Z., Tunis, S.L. & Lage, M.J. Medication Treatment Patterns following Initiation on Olanzapine versus Risperidone. Clin. Drug Investig. 22, 741–749 (2002). https://doi.org/10.2165/00044011-200222110-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-200222110-00003