Abstract
Prion diseases are transmissible neurodegenerative diseases of humans and animals. The prion agent consists of a misfolded protein, PrPSc (prion protein, scrapie form), of a glycosylphosphatidylinositol-anchored host protein, PrPC (PrP cellular form) of unknown function. During prion replication, PrPSc induces host PrPC to adopt its pathogenic conformation. Some PrPSc may aggregate to microscopically visible, extracellular prion plaques that stain for amyloid.
The development of antiprion vaccines presents some challenges. While there is strong self-tolerance to an endogenous antibody response to PrPC and PrPSc, highly potent monoclonal antibodies (mAbs) have been raised in mice in which the prion protein gene has been deleted by gene targeting. These mAbs have been demonstrated to be antiprion-active in permanently scrapie-infected neuroblastoma (ScN2a) cells, primarily when bound to one of four epitopes (the octarepeat region, the region around codons 90–110, helix 1 region codons 145–160, and the extreme C-terminal codons 210–220). The mAbs directed against codon regions 90–110 or 145–160 are also antiprion-active in vivo, but only after intraperitoneal infection with prions, not intracerebral infection, suggesting their blood-brain barrier (BBB) impermeability. The challenge will be to make antibodies, or recombinant derivatives thereof, BBB permeable; this is preferably achieved by monovalent antibody fragments since divalent ones were found to be neurotoxic.
Self-tolerance of wild-type animals to PrP immunizations was found to be of extrathymic origin. Even though antibodies raised in wild-type mice were found to display antiprion activity in ScN2a cells, these mice did not have significant extensions of incubation times when challenged intraperitoneally with prions. A general low affinity of these antibody responses to native surface-bound PrPC may account for this.
Since wild-type mice were found to develop sufficient T-cell responses to codon regions 145–160 and 210–220, we believe that there is a theoretical chance of a successful vaccination therapy. The influence of the way the immunogen is presented has already been shown to be of major importance for the ensuing immune response, in that presentation of PrP with CpG oligodeoxynucleotides as adjuvant or viral packaging improved antibody responses. Major progress for active immunizations may therefore be expected in this field. Eradication programs will be one of the most important uses of active immunization protocols. For this purpose, vaccines will have to be inexpensive, easy to handle, and effective. In the short term, passive immunizations will likely be most promising for therapy of prion disease, including for human medical interventions. Active immunization protocols are less likely to succeed quickly, and will take years if not decades to be validated for domestic or free-ranging animals.
Similar content being viewed by others
Prion diseases are transmissible neurodegenerative diseases of humans and animals.[1] Animal prion diseases include scrapie of goat and sheep, bovine spongiform encephalopathy (BSE) from cattle, chronic wasting disease (CWD) of American mule deer and elk, as well as transmissible mink encephalopathy. Animal prion diseases such as scrapie are endemic in some countries, with prevalences of up to 10% of the sheep population,[2] and can be epidemic in scale, like the BSE epidemic that peaked in the 1990s in Great Britain and moved to almost all European countries. On the other hand, they can be highly prevalent in strictly local areas, like CWD in some Rocky Mountain states in the US, with prevalences of up to 10% of the wildlife population of mule deer and elk.[2,3]
Human prion diseases are still very rare. The most prevalent human prion disease is Creutzfeldt-Jakob disease (CJD), with a worldwide prevalence of ≈1 per million.[4] Other, even rarer, human prion diseases are of genetic origin and include Gerstmann-Sträussler Scheinker disease or fatal familial insomnia. Most cases of CJD (≈90%) are of sporadic origin, ≈9% are of genetic origin, and <1% are of an infectious origin. The major routes of CJD transmission are iatrogenic transfer of prions via organ transplantations from patients with (subclinical) CJD, for example, dura or cornea transplantations.[5] One form of infectious human prion disease has been Kuru of the Fore tribe in Papua New Guinea, which was transmitted through ritualistic cannibalism and disappeared once cannibalism was abolished.[6]
It is widely believed that humans are protected from prevalent animal prion diseases by a species barrier, i.e. the inability of prions from one species to infect another, phylogenetically more remote, species. For example, endemic scrapie has been described for centuries,[7] but epidemiological and transmission studies have consistently led to the conclusion that a species barrier protects humans from sheep prions.[4,8] Public concern was raised with the appearance of cases of a new strain of CJD, termed variant (v) CJD, that were caused by ingestion of BSE prions, indicating that there was no strict species barrier in humans for bovine prions.[9,10] The danger of this strain was emphasized by its transmissibility via blood.[11]
The infectious agent, the prion, is thought to consist solely of a misfolded conformation of the prion protein (PrP).[12,13] In the absence of nucleic acids,[14] replication of prions is thought to occur via conversion of the normal cellular prion protein, PrPC, into the disease-associated PrP scrapie form, PrPSc.[1,12] PrPC is a protein of unknown function that is highly expressed in lymphoid and neuronal tissues. Conversion is currently hypothesized to occur either by a monomer/small oligomer PrPSc[1] or, according to the amyloid self-polymerization model, by a template in a larger fibril consisting of PrPSc, which induces conversion/adhesion through a nucleation-like process.[15
Prion diseases are classed between infectious diseases and amyloid diseases of the brain. In fact, prions have sometimes been called ‘infectious amyloid.’ It is clear, however, that prion diseases are the only infectious amyloid diseases of the brain, and that other amyloid diseases of the brain like Alzheimer disease are not infectious.[16,17] Nevertheless, for both infectious diseases and Alzheimer disease (the classical and most prevalent amyloid disease), antibody- or vaccination-based therapies have been successful.[18] Active immunization or vaccination is the term used when the whole immune system is stimulated by a suitable immunogen to mount a complete nonspecific and specific immune response, including T-cell and B-cell/antibody responses, whereas passive immunization is understood to solely comprise administration of antibodies to a defined antigen.
In the classical infectious diseases, the infectious agent provides novel epitopes for the cellular and humoral immune system, against which antibodies will be directed. In the amyloid diseases, presentation of novel, disease-associated conformation-specific epitopes,[17] i.e. novel 3-dimensional foldings of a protein population, signals the immune system to raise a protective immune response, which leads to opsonization and clearance of aggregated extracellular protein deposits. By analogy, presentation of prion plaques, or PrPSc, should elicit such an immune response, clearing this aberrant conformational species. The problem is that, because of its infectious nature, the agent cannot be used for immunization itself. Also, no laboratory has yet reported the emergence of a PrPSc-specific immune response during prion disease.[19]
What is the potential use of vaccination or antibody-based therapies? Recent investigations in an inducible PrP-knockout transgenic mouse model demonstrated that when PrP was knocked out after experimental prion infection started to produce clinical symptoms, early symptoms as well as vacuolation and dendritic changes were reversible.[20,21] These surprising results raised hopes that therapies even after disease onset might not be in vain. For humans, there are two likely major applications of antiprion (α-PrP) antibodies: (i) passive immunization, i.e. antibody-based therapy of human prion disease, possibly with antibodies recombinantly optimized to cross the BBB; and (ii) post-exposure prophylaxis after accidental contact with prions and decontamination of (vCJD) prion-infected blood.
For animals, prevention and eradication of the major diseases (scrapie, BSE, and CWD) with highly efficient active immunization strategies will be the goal. One consideration for a commercial immunotherapy-based eradication program is that the total cost of the therapy per animal should not exceed the market price of the animal itself, in order to elicit a user demand. Therefore, vaccination strategies have to be both efficient and inexpensive. It is also clear that because of the long incubation time of natural prion diseases, the validation of the efficacy of potential, experimentally successful vaccination strategies will take decades rather than years.
1. Antiprion-Active Antibodies
An early proof of the antiprion effect of anti-PrP antibodies was the decrease of inoculum titer of an experimental prion infection when it was preincubated with a polyclonal antiserum generated against PrP in rabbits.[22] The question then was whether antibodies could also induce cellular procedures leading to the complete disappearance of prions.
1.1 Antiprion Activity in Cell Assays
Permanently scrapie-infected neuroblastoma (ScN2a) cells have been a major model for investigating prion diseases.[23–25] These cell lines have been used to identify a variety of small-molecule antiprion compounds.[26–29] Initial monoclonal antibodies (mAbs) produced in mice were against Syrian hamster PrP and did not cross-react with mouse PrP, because of the high homology of PrP within mammalian species and ensuing self-tolerance.[30,31] The first high-affinity mAbs were produced in PrP-knockout mice.[32,33] mAb 6H4, recognizing helix 1 of the prion protein,[34] an exposed domain in the PrP structure that is thought to have a key role in the conversion process, proved to be highly antiprion active in ScN2a cells[35] (figure 1). A concentration of 6H4 antibody of 1 µg/mL cleared any residual PrPSc after 14 days. The cells continued to express PrPC and remained free of PrPSc for at least 6 weeks after the antibody had been removed from culture medium.[35] Subsequently, the effectiveness of helix 1 as an antiprion antigen was confirmed by other mAbs, with inhibitory concentration (IC50) values mostly in the low nanomolar or subnanomolar range.[36–39] Helix 1 of PrPC was also shown to be an interaction domain of PrPSc, thus likely to have a role in PrP conversion[40] (figure 1).
Schematic summary of the current knowledge on mouse prion protein (PrP) sequence-associated immunological features. Sequence is schematic, not to scale; longitudinal lines are in steps of 50 amino acids along the PrP sequence. Secondary structure according to Riek et al.:[41] β-strand 1 (B1) 128–131, α-helix 1 (H1) 145–155, β-strand 2 (B2) 161–164, α-helix 2 (H2) 175–193, α-helix 3 (H3) 200–219. Darker green filled bars indicate strong binding/reaction with the respective polypeptide sequence indicated at top, and lighter green filled bars indicate weak binding/reaction. B-cell ko = B-cell epitopes in PrP knockout (ko) mice; B-cell wt = B-cell epitopes in wild-type (wt) C57BL/6 mice; Fab = fragment, antibody binding; mAb = monoclonal antibody; MHC II = major histocompatibility complex type II binding motifs; PrP C -PrP Sc = PrP cellular form — PrP scrapie form interaction domain; T-cell ko = T-cell proliferation domains in PrP ko mice; T-cell wt = T-cell proliferation domains in wt C57BL/6 mice.
Antibodies to at least three other domains of PrP seem to confer antiprion potency: (i) the octarepeat region;[42,43] (ii) the region around codons 91–110 (mAb ICSM 35;[36] Fab D13[39]); and (iii) the extreme C-terminus (Fab R1, R2[39]) [see figure 1]. A synergistic antiprion effect was observed after treatment with different antibodies,[37] suggesting that combining antibodies with different epitopes might be beneficial in therapeutic strategies.
The mechanism of action of antibodies clearing PrPSc in cells is not completely understood. Antiprion effects can, theoretically, arise through interference with several molecular targets.[44] For antibodies, these primarily involve the shielding of PrPC from the presumed docking of PrPSc, or sequestering of the PrPSc template itself. While it has been argued that shielding PrPC might be the most efficient antiprion strategy of single antibodies,[39] others have reported that dual targeting of PrPC and PrPSc improved the efficiency of antiprion antibodies.[36] No reports have been published on the antiprion effects of mAbs specific for the PrPSc conformation.[34,45,46] If PrPSc is present in post-membrane compartments inaccessible to antibodies, exclusive targeting of PrPSc may not be as effective as targeting of both PrPC and PrPSc. From these studies it can be concluded that conformation specificity or conformational epitopes are not a prerequisite of antiprion mAb potency.
Multivalent ligands of cell surface antigens can sometimes trigger signal transduction events. Direct intracerebral injection of full length anti-PrP antibodies (mAbs D13 and P against residues 95–105), but not their monovalent Fab fragments, were reported to induce extensive neural loss after 24 hours, albeit at an unphysiologically high concentration (1 mg/mL).[47] Interestingly, a full length mAb (D18), binding to helix 1, induced no cell damage under the same conditions. These studies suggest that monovalent antibodies might be better suited for in vivo immunization therapies than full length antibodies. Accordingly, ScN2a cells treated with single-chain fragments (scFv) to prion protein helix 1 expressed in a mammalian co-culture system were shown to reduce PrPSc efficiently.[48] If the existence of an essential conversion factor like the elusive protein X[49] was proven, or an essential uptake receptor for prions was demonstrated, blocking their interaction sites with PrP might be a target for antibody-based therapies. It has been claimed that the laminin receptor is required for prion propagation;[50] however, the use of scFv antibodies has so far not led to a complete PrPSc clearance and has failed to exhibit significant antiprion effects in vivo.[51]
1.2 Effects of Antiprion Antibodies in Animal Models of Prion Disease
Antiprion activity of antibodies in vivo was shown in two seminal experiments. A transgenic mouse model expressing a fragment of mAb 6H4 (6H4μ)[52] demonstrated that (i) the antibody titers generated were sufficient to protect from a peripheral (intraperitoneal) prion inoculation; and (ii) the antibodies did not generate an autoimmune disease or toxic effects. No PrPSc was detected in spleens of 6H4μ-mice 234 days post-inoculation (dpi), whereas controls showed splenic infectivity after 50 days.
In a true passive immunization experiment it was shown that a twice-weekly 2 mg per mouse administration of either mAbs ICSM 35 (recognizing amino acids 91–110) or ICSM 18 (recognizing amino acids 146–159; see figure 1) over a prolonged period (starting 7 or 30 days after inoculation for) protected FVB/N wild-type mice from peripheral (intraperitoneal) infection of prions.[53] At 60 days after inoculation, splenic PrPSc levels were almost completely reduced by ICSM 18, and to a somewhat lesser extent by ICSM 35. Of note, all treated animals inoculated intraperitoneally survived longer than 500 days without signs of illness. Although mABs were effective even when applied 30 dpi (when peripheral PrPSc accumulation reached plateau levels), mice were not protected if administration was started after the appearance of the first clinical signs.
In both the antibody-expressing transgenic mice and passively immunized mice, antibody protection was effective only when inoculation was peripheral and had to go through the phase of neuroinvasion, during which the antibodies likely executed their neutralizing effects. Whether failing protection of these antibodies to intracerebral inoculation was due to their lack of BBB permeability is currently unclear.
Summarizing these experiments, we can state that:
-
antibodies can clear prions in vitro (cells) and in vivo (mice);
-
antibody protection in vivo seems confined to peripheral inoculations;
-
those antibodies with high antiprion efficacy are derived from immunizations of PrP-knockout mice; and
-
there do not seem to be relevant autoimmune effects when endogenous PrP and α-PrP antibodies meet.
2. Vaccination
2.1 Overcoming Self-Tolerance
The major problem of active immunization against prion disease is the strong self-tolerance of recipient subjects to PrP. This is in strong contrast to successful immunizations with Aβ peptide in animal models of Alzheimer disease[18] or in humans,[54] where a humoral immune response was developed, indicating that major epitopes of oligomeric or multimeric Aβ are, in fact, immunogenic. During experimental or natural prion disease, no prion-specific antibody response has been reported.[19,55] Whether this is due to the non-immunogenicity of the conformational difference between PrPC and PrPSc, or a low-abundance ‘physiological’ PrPSc of unknown function establishing self-tolerance, is unknown.
There have been attempts to circumvent self-tolerance to PrP in wild-type mice by immunization of a dimeric recombinant PrP generated in Escherichia coli,[56] by using CpG oligodeoxynucleotides as adjuvant in a DNA immunization strategy,[57] utilizing multiple-antigen peptides,[58] cross-linking to keyhole limpet hemocyanin,[59] or packaging of PrP in viral particles.[60,61] Attempts to circumvent self-tolerance by immunizing with PrP of different species revealed that BALB/c mice immunized with bovine recombinant PrP and complete Freund adjuvant (CFA) led to a slight prolongation of survival time after intraperitoneal prion challenge.[62] So far, neither of these strategies has been shown to cure or to have dramatic effects on survival time when applied to in vivo experiments where wild-type animals were challenged with prions.
Particular attention has to be given to the adjuvants used, which in ≈80% of all immunization studies was CFA. Administration of CFA alone, a common immunostimulant and carrier solution for immunogens in animals, was demonstrated to prolong incubation time after intracerebral or intraperitoneal prion challenge.[63] Single boosts of CpG oligodeoxynucleotides are similarly known to stimulate the innate, nonspecific immune system.[64,65] When CpG oligodeoxynucleotides were repeatedly administered to prion-infected mice over several or many days, a prolongation of incubation time was observed.[66] However, this was later attributed to a massive suppression or destruction of follicular dendritic cells — sites of peripheral prion replication.[67]
Whether antiprion-active antibodies could be raised in wild-type mice was investigated by immunization of C57BL/6 with recombinantly expressed mouse PrP/CFA.[56] The antibodies generated were demonstrated to have antiprion activity in ScN2a cells (major epitopes mapped to residues 129–148), but the immunization did not protect from an intraperitoneal prion challenge.[68] This discrepancy was attributed to a remaining self-tolerance to PrP resulting in low-affinity antibodies against non-ideal epitopes.[68] Using lines of transgenic mice expressing PrP under tissue-specific promoters on the PrP-knockout background, it was demonstrated that thymic PrP expression was not a prerequisite for an absent or weak humoral α-PrP response, since PrP expressed exclusively on T cells, B cells, hepatocytes, or neurons had an equally insufficient immune response. Only complete PrP knockout or PrP exclusively expressed on Schwann cells and oligodendrocytes led to strong humoral immune responses.[68] These investigators also suggested that only antibodies binding native PrP on the cell surface, but not antibodies binding solely to recombinant PrP, had sufficient affinity to elicit antiprion effects.
2.2 Focusing the Immune Response
Attempts to identify major immunogenic regions of PrP in wild-type animals have been made through systematic screening or thoughtful design of PrP polypeptides.
Peptides corresponding to codons 131–150 and 211–230 were found to have a major histocompatibility complex (MHC) II binding motif in wild-type mice[69] and equally were found to elicit the highest T-cell proliferative responses in a screen of 20mer peptides (codons 31–50, and 151–170 weak response; figure 1); for (unconjugated) peptide 131–150, a decrease of PrPSc levels in mouse-implanted ScN2a cells was demonstrated.[69] Another group showed in a 30mer screen that peptides corresponding to codons 143–172 and 156–187 elicited the strongest T-cell proliferation responses in PrP-knockout mice, with 98–127 also displaying weaker, but sufficient, T-cell proliferative responses (figure 1).[70]
Comparing B-cell immune responses of 30mer overlapping peptides in PrP-knockout versus wild-type mice (both on the C57BL/6 genetic background, and immunized with CpG oligonucleotides as adjuvant) revealed that wild-type mice had a preferred response to epitopes in the region codon 158–187, and 193–212, whereas PrP-knockout mice covered epitopes in the codon regions 118–172 and 212–218[71] (see figure 1). PrP-knockout mice mounted a mixed antibody response with IgG1 and IgG2b, whereas wild-type mice had a strong abundance of IgG2b antibodies; IgG2a antibodies were of low abundance in both mouse types.[71] Interestingly, from immunization studies in Alzheimer disease it is known that IgG1 antibodies, although binding with higher affinity to Aβ plaques, are less efficient for clearing plaques than IgG2a antibodies.[72]
Thus, there is an overlap of PrP polypeptides evoking T-cell proliferation with B-cell epitopes in wild-type mice, particularly around residues 150–170, and 210–220 (which coincide with antiprion activity in ScN2a cells) and, for codon region 150–170, with antiprion activity in vivo (see figure 1).
2.3 Viral Packaging for Antigen Presentation
Viruses can be very strong inducers of immune reactions, to the extent of being able to trigger autoimmune diseases.[73] Packaging of major antigenic regions of PrP into suitable viruses or viral particles may therefore improve the way the self-tolerant PrP antigen is presented and help elicit antiprion antibody titers.
Nikles and colleagues[60] chose a retroviral display system presenting full-length mouse PrP 121–231 on virus-like particles derived from murine leukemia virus. Specific IgM and IgG antibodies recognizing native PrPC were induced in PrP-knockout and wild-type mice. Of note, the magnitude of PrP-specific IgM response was inversely related to the number of PRNP (prion gene) alleles expressed. The highest antibody titers were, expectedly, induced in PrP-knockout mice, however intermediate and lower levels were also present in heterozygous and wild-type mice, respectively.[60]
In another recent study, the immunogenic surface loop of the bovine papillomavirus type 1 major capsid protein was used to display a helix 1 peptide of the murine PrP (codon 144–152) at up to 360 copies/capsid.[61] With this vaccine, high titers of antibodies recognizing native PrPC could be raised in rabbit and rat, and the rabbit antisera interfered with prion replication in ScN2a cells.[61] Unfortunately, results on whether this antigen-presenting strategy provides protection from a prion challenge in vivo have not been reported.
2.4 Mucosal Vaccination
Since the major route of prion transmission in animals is thought to occur via ingesting contaminated food,[74,75] investigations have also included the possibility of inducing mucosal immunity for protecting against prion disease. The idea is to prevent entry of PrPSc from the gut into the body.
In one set of experiments, BALB/c mice were immunized either intragastrically or intranasally with a recombinant PrP fragment (codon 90–231) and cholera toxin adjuvant.[76] Intranasal immunization elicited a low but significant IgA response, and slightly prolonged incubation time after an oral challenge.[76] Similarly, intranasal immunization with fusion proteins of bovine PrP (codon 132–242) or mouse PrP (codon 120–231) with the B subunit of E. coli heat-labile enterotoxin was able to elicit IgA responses, although weakly, when PrP of the same species was used.
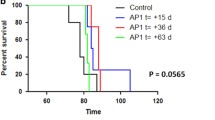
In yet another set of experiments, a live attenuated Salmonella typhimurium vaccine strain-expressing mouse PrP cDNA was used to immunize wild-type CD-1 mice.[77] This vaccine induced both IgA and, to a lower extent, IgG responses. Whereas all control animals died within 300 days of post-oral challenge and displayed scrapie-infected brain homogenate, survival of two independent treatment groups was markedly prolonged. After 500 days, 30% of treated mice were still alive, without showing any evidence of PrPSc in their brains or spleens.[77]
3. Conclusions and Challenges
The last 7 years have brought huge successes in antibody-based therapies of prion diseases. A breakthrough was clearly the demonstration that peripherally administered mAbs could prevent a peripheral prion challenge.[53] Even though antibody therapy was effective against peripheral prion challenge, it did not protect from intracerebral prion challenge, similar to transgenic expression of an antiprion mAb 6H4 fragment.[52] Thus, antiprion antibodies do not easily pass the BBB, unlike many anti-Aβ antibodies in successful passive immunization of Alzheimer disease.[78] Here, the future challenge will be to make these mAbs or, preferably, recombinant antibodies thereof, BBB permeable in order to increase their antiprion efficacy. Because of the possible neurotoxicity of bivalent mAbs,[47] monovalent recombinant antibodies may be the way forward. In fact, scFv fragments derived from mAb 6H4 have been shown to decrease PrPSc levels in ScN2a cells significantly.[48] Recombinant scFv fragments offer the prospect of being recombinantly modified with signal sequences or chimeric proteins facilitating BBB entry. They can further be optimized for antiprion therapy by directed mutagenesis, and later on be humanized for therapeutic applications in humans.
The best current target within PrP for immunization, be it active or passive, is the area around helix 1 (residues 145–160, see figure 1), which has been shown to induce T-cell proliferation in wild-type mice and to be a preferred B-cell epitope with high antibody titers. At the same time, antibodies against the helix 1 region have consistently been shown to be antiprion active in ScN2a cells, and in vivo. Helix 1 seems to be an interaction site with PrPSc, thus providing a solid mechanism of action for the antiprion effects. All these facts argue for focusing vaccine development on this region. To date, the only limitation is that no single mAb against this region has been raised in wild-type mice with convincing antiprion activity. Nonetheless, generating such a mAb in wild-type mice may be an excellent read-out system for screening active immunization strategies.
Active immunization strategies are likely to focus on antigen presentation. For example, change of adjuvant from CFA to CpG changed immune responses to PrP significantly,[71] and viral packaging is likely to have considerable future potential in this direction. Simple, inexpensive, and effective active immunization strategies are sought for eradication programs of the major animal prion diseases scrapie, BSE, and CWD. CWD is currently the most rapidly spreading prion disease that, uniquely, also affects wild living animals, with possible ecological consequences. While active immunization with recombinant immunogens may be practicable in domestic animals, in order to cover a wild population of deer or elk, live antiprion vaccines — i.e. nonpathogenic viruses presenting PrP epitopes in such a way that an efficient antiprion response is elicited — may be worth consideration.
References
Prusiner SB. Prions. Proc Natl Acad Sci U S A 1998; 95: 13363–83
Prusiner SB, Williams E, Laplanche J-L, et al. Scrapie, chronic wasting disease, and transmissible mink encephalopathy. In: Prusiner SB, editor. Prion biology and diseases. Cold Spring Harbor (NY): Cold Spring Harbor Laboratory Press, 2004: 545–94
Williams ES, Miller MW. Chronic wasting disease in deer and elk in North America. Rev Sci Tech 2002; 21(2): 305–16
Kong Q, Surewicz KA, Petersen RB, et al. Inherited prion diseases. In: Prusiner SB, editor. Prion biology and diseases. 2nd ed. Cold Spring Harbor (NY): Cold Spring Harbor Laboratory Press, 2004: 673–775
Will RG. Acquired prion disease: iatrogenic CJD, variant CJD, kuru. Br Med Bull 2003; 66: 255–65
Gajdusek DC. Unconventional viruses and the origin and disappearance of kuru. Science 1977; 197: 943–60
Leopoldt JG. Der Trab ist auch eine Krankheit der Schafe, und ist ansteckend. In: Sorau H-PWdH, editor. Nützliche und auf Erfahrung gegründete Einleitung zu der Landwirtschaft. Berlin: Christian Friedrich Günthern, 1759
Collins S, Law MG, Fletcher A, et al. Surgical treatment and risk of sporadic Creutzfeldt-Jakob disease: a case-control study. Lancet 1999; 353(9154): 693–7
Will RG, Ironside JW, Zeidler M, et al. A new variant of Creutzfeldt-Jakob disease in the UK. Lancet 1996; 347: 921–5
Scott MR, Will R, Ironside J, et al. Compelling transgenetic evidence for transmission of bovine spongiform encephalopathy prions to humans. Proc Natl Acad Sci U S A 1999; 96: 15137–42
Llewelyn CA, Hewitt PE, Knight RS, et al. Possible transmission of variant Creutzfeldt-Jakob disease by blood transfusion. Lancet 2004; 363(9407): 417–21
Prusiner SB. Novel proteinaceous infectious particles cause scrapie. Science 1982; 216: 136–44
Pan K-M, Baldwin M, Nguyen J, et al. Conversion of α-helices into β-sheets features in the formation of the scrapie prion proteins. Proc Natl Acad Sci U S A 1993; 90: 10962–6
Safar JG, Kellings K, Serban A, et al. Search for a prion-specific nucleic acid. J Virol 2005; 79: 10796–806
Harper JD, Lansbury Jr PT. Models of amyloid seeding in Alzheimer’s disease and scrapie: mechanistic truths and physiological consequences of the time-dependent solubility of amyloid proteins. Annu Rev Biochem 1997; 66: 385–407
Brown P, Gibbs Jr CJ, Rodgers-Johnson P, et al. Human spongiform encephalopathy: the National Institutes of Health series of 300 cases of experimentally transmitted disease. Ann Neurol 1994; 35: 513–29
Leliveld SR, Korth C. The use of conformation-specific ligands and assays to dissect the molecular mechanisms of neurodegenerative diseases. J Neurosci Res 2007; 85: 2285–97
Schenk D, Barbour R, Dunn W, et al. Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature 1999; 400: 173–7
Bockman JM, Kingsbury DT. Immunological analysis of host and agent effects on Creutzfeldt-Jakob disease and scrapie prion proteins. J Virol 1988; 62: 3120–7
Mallucci G, Dickinson A, Linehan J, et al. Depleting neuronal PrP in prion infection prevents disease and reverses spongiosis. Science 2003; 302: 871–4
Mallucci GR, White MD, Farmer M, et al. Targeting cellular prion protein reverses early cognitive deficits and neurophysiological dysfunction in prion-infected mice. Neuron 2007; 53: 325–35
Gabizon R, McKinley MP, Groth D, et al. Immunoaffinity purification and neutralization of scrapie prion infectivity. Proc Natl Acad Sci U S A 1988; 85: 6617–21
Butler DA, Scott MRD, Bockman JM, et al. Scrapie-infected murine neuroblastoma cells produce protease-resistant prion proteins. J Virol 1988; 62: 1558–64
Race RE, Fadness LH, Chesebro B. Characterization of scrapie infection in mouse neuroblastoma cells. J Gen Virol 1987; 68: 1391–9
Bosque PJ, Prusiner SB. Cultured cell sublines highly susceptible to prion infection. J Virol 2000; 74: 4377–86
Caughey B, Race RE. Potent inhibition of scrapie-associated PrP accumulation by Congo red. J Neurochem 1992; 59: 768–71
Supattapone S, Nguyen H-OB, Cohen FE, et al. Elimination of prions by branched polyamines and implications for therapeutics. Proc Natl Acad Sci U S A 1999; 96: 14529–34
Korth C, May BCH, Cohen FE, et al. Acridine and phenothiazine derivatives as pharmacotherapeutics for prion disease. Proc Natl Acad Sci U S A 2001; 98: 9836–41
Klingenstein R, Lober S, Kujala P, et al. Tricyclic antidepressants, quinacrine and a novel, synthetic chimera thereof clear prions by destabilizing detergent-resistant membrane compartments. J Neurochem 2006; 98: 748–59
Kascsak RJ, Rubenstein R, Merz PA, et al. Mouse polyclonal and monoclonal antibody to scrapie-associated fibril proteins. J Virol 1987; 61: 3688–93
Rogers M, Serban D, Gyuris T, et al. Epitope mapping of the Syrian hamster prion protein utilizing chimeric and mutant genes in a vaccinia virus expression system. J Immunol 1991; 147: 3568–74
Büeler H, Aguzzi A, Sailer A, et al. Mice devoid of PrP are resistant to scrapie. Cell 1993; 73: 1339–47
Prusiner SB, Groth D, Serban A, et al. Ablation of the prion protein (PrP) gene in mice prevents scrapie and facilitates production of anti-PrP antibodies. Proc Natl Acad Sci U S A 1993; 90: 10608–12
Korth C, Stierli B, Streit P, et al. Prion (PrPSc)-specific epitope defined by a monoclonal antibody. Nature 1997; 389: 74–7
Enari M, Flechsig E, Weissmann C. Scrapie prion protein accumulation by scrapie-infected neuroblastoma cells abrogated by exposure to a prion protein antibody. Proc Natl Acad Sci U S A 2001; 98: 9295–9
Beringue V, Vilette D, Mallinson G, et al. PrPSc binding antibodies are potent inhibitors of prion replication in cell lines. J Biol Chem 2004; 279: 39671–6
Perrier V, Solassol J, Crozet C, et al. Anti-PrP antibodies block PrP replication in prion-infected cell cultures by accelerating PrP degradation. J Neurochem 2004; 89: 454–63
Kim CL, Karino A, Ishiguro N, et al. Cell-surface retention of PrPC by anti-PrP antibody prevents protease-resistant PrP formation. J Gen Virol 2004; 85: 3473–82
Peretz D, Williamson RA, Kaneko K, et al. Antibodies inhibit prion propagation and clear cell cultures of prion infectivity. Nature 2001; 412: 739–43
Solforosi L, Bellon A, Schaller M, et al. Toward molecular dissection of PrPC- PrPSc interactions. J Biol Chem 2007; 282: 7465–71
Riek R, Hornemann S, Wider G, et al. NMR characterization of the full-length recombinant murine prion protein, mPrP(23-231). FEBS Lett 1997; 413: 282–8
Demart S, Fournier J-G, Creminon C, et al. New insight into abnormal prion protein using monoclonal antibodies. Biochem Biophys Res Commun 1999; 265: 652–7
Feraudet C, Morel N, Simon S, et al. Screening of 145 anti-PrP monoclonal antibodies for their capacity to inhibit PrPSc replication in infected cells. J Biol Chem 2005; 280: 11247–58
Korth C, Peters PJ. Emerging pharmacotherapies for Creutzfeldt-Jakob disease. Arch Neurol 2006; 63: 497–501
Paramithiotis E, Pinard M, Lawton T, et al. A prion protein epitope selective for the pathologically misfolded conformation. Nat Med 2003; 9: 893–9
Moroncini G, Kanu N, Solforosi L, et al. Motif-grafted antibodies containing the replicative interface of cellular PrP are specific for PrPSc. Proc Natl Acad Sci U S A 2004; 101: 10404–9
Solforosi L, Criado JR, McGavern DB, et al. Cross-linking cellular prion protein triggers neuronal apoptosis in vivo. Science 2004; 303: 1514–6
Donofrio G, Heppner FL, Polymenidou M, et al. Paracrine inhibition of prion propagation by anti-PrP single-chain Fv miniantibodies. J Virol 2005; 79: 8330–8
Telling GC, Scott M, Mastrianni J, et al. Prion propagation in mice expressing human and chimeric PrP transgenes implicates the interaction of cellular PrP with another protein. Cell 1995; 83: 79–90
Leucht C, Simoneau S, Rey C, et al. The 37 kDa/67 kDa laminin receptor is required for PrP(Sc) propagation in scrapie-infected neuronal cells. EMBO Rep 2003; 4: 290–5
Zuber C, Knackmuss S, Rey C, et al. Single chain Fv antibodies directed against the 37kDa/67kDa laminin receptor as therapeutic tools in prion diseases. Mol Immunol 2088; 45: 144–51
Heppner FL, Musahl C, Arrighi I, et al. Prevention of scrapie pathogenesis by transgenic expression of anti-prion protein antibodies. Science 2001; 294: 178–82
White AR, Enever P, Tayebi M, et al. Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature 2003; 422: 80–3
Orgogozo JM, Gilman S, Dartigues JF, et al. Subacute meningoencephalitis in a subset of patients with AD after Abeta42 immunization. Neurology 2003; 61: 46–54
Barry RA, McKinley MP, Bendheim PE, et al. Antibodies to the scrapie protein decorate prion rods. J Immunol 1985; 135: 603–13
Gilch S, Wopfner F, Renner-Muller I, et al. Polyclonal anti-PrP auto-antibodies induced with dimeric PrP interfere efficiently with PrPSc propagation in prion-infected cells. J Biol Chem 2003; 278: 18524–31
Rosset MB, Ballerini C, Gregoire S, et al. Breaking immune tolerance to the prion protein using prion protein peptides plus oligodeoxynucleotide-CpG in mice. J Immunol 2004; 172: 5168–74
Arbel M, Lavie V, Solomon B. Generation of antibodies against prion protein in wild-type mice via helix 1 peptide immunization. J Neuroimmunol 2003; 144: 38–45
Schwarz A, Kratke O, Burwinkel M, et al. Immunisation with a synthetic prion protein-derived peptide prolongs survival times of mice orally exposed to the scrapie agent. Neurosci Lett 2003; 350: 187–9
Nikles D, Bach P, Boller K, et al. Circumventing tolerance to the prion protein (PrP): vaccination with PrP-displaying retrovirus particles induces humoral immune responses against the native form of cellular PrP. J Virol 2005; 79: 4033–42
Handisurya A, Gilch S, Winter D, et al. Vaccination with prion peptide-displaying papillomavirus-like particles induces autoantibodies to normal prion protein that interfere with pathologic prion protein production in infected cells. FEBS J 2007; 274: 1747–58
Ishibashi D, Yamanaka H, Yamaguchi N, et al. Immunization with recombinant bovine but not mouse prion protein delays the onset of disease in mice inoculated with a mouse-adapted prion. Vaccine 2007; 25: 985–92
Tal Y, Souan L, Cohen IR, et al. Complete Freund’s adjuvant immunization prolongs survival in experimental prion disease in mice. J Neurosci Res 2003; 71: 286–90
Oxenius A, Martinic MM, Hengartner H, et al. CpG-containing oligonucleotides are efficient adjuvants for induction of protective antiviral immune responses with T-cell peptide vaccines. J Virol 1999; 73: 4120–6
Vabulas RM, Pircher H, Lipford GB, et al. CpG-DNA activates in vivo T cell epitope presenting dendritic cells to trigger protective antiviral cytotoxic T cell responses. J Immunol 2000; 164: 2372–8
Sethi S, Lipford G, Wagner H, et al. Postexposure prophylaxis against prion disease with a stimulator of innate immunity. Lancet 2002 Jul 20; 360(9328): 229–30
Heikenwalder M, Polymenidou M, Junt T, et al. Lymphoid follicle destruction and immunosuppression after repeated CpG oligodeoxynucleotide administration. Nat Med 2004; 10: 187–92
Polymenidou M, Heppner FL, Pellicioli EC, et al. Humoral immune response to native eukaryotic prion protein correlates with anti-prion protection. Proc Natl Acad Sci U S A 2004; 101Suppl. 2: 14670–6
Souan L, Tal Y, Felling Y, et al. Modulation of proteinase-K resistant prion protein by prion peptide immunization. Eur J Immunol 2001; 31: 2338–46
Gregoire S, Logre C, Metharom P, et al. Identification of two immunogenic domains of the prion protein — PrP — which activate class II-restricted T cells and elicit antibody responses against the native molecule. J Leukoc Biol 2004; 76: 125–34
Gregoire S, Bergot AS, Feraudet C, et al. The murine B cell repertoire is severely selected against endogenous cellular prion protein. J Immunol 2005; 175: 6443–9
Bard F, Barbour R, Cannon C, et al. Epitope and isotype specificities of antibodies to beta-amyloid peptide for protection against Alzheimer’s disease-like neuropathology. Proc Natl Acad Sci U S A 2003; 100: 2023–8
Schattner A. Consequence or coincidence? The occurrence, pathogenesis and significance of autoimmune manifestations after viral vaccines. Vaccine 2005; 23: 3876–86
Wilesmith JW, Ryan JB, Atkinson MJ. Bovine spongiform encephalopathy: epidemiological studies on the origin. Vet Rec 1991; 128: 199–203
Miller MW, Wild MA, Williams ES. Epidemiology of chronic wasting disease in captive Rocky Mountain elk. J Wildl Dis 1998; 34: 532–8
Bade S, Baier M, Boetel T, et al. Intranasal immunization of Balb/c mice against prion protein attenuates orally acquired transmissible spongiform encephalopathy. Vaccine 2006; 24: 1242–53
Goni F, Knudsen E, Schreiber F, et al. Mucosal vaccination delays or prevents prion infection via an oral route. Neuroscience 2005; 133: 413–21
Bard F, Cannon C, Barbour R, et al. Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat Med 2000; 6: 916–9
Acknowledgments
The authors receive funding from the Research Commission of the University of Düsseldorf Medical School, the VW Stiftung, Germany, the BMBF, Germany, and EU Research Commission ANTEPRION LSHB-CT-019090. Funding agencies had no role in this manuscript.
The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller-Schiffmann, A., Korth, C. Vaccine Approaches to Prevent and Treat Prion Infection. BioDrugs 22, 45–52 (2008). https://doi.org/10.2165/00063030-200822010-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00063030-200822010-00005