Abstract
Introduction and objectives
To assess the cost effectiveness of a clinical decision support system (CDSS) based on the recommendations of the European Society of Cardiology and other societies for Hypercholesterolemia Management (ESCHM).
Study design and perspective
A cluster-randomized, unblinded, pragmatic trial was conducted. To assess the impact in effectiveness and costs of a CDSS implementing an adapted version of the ESCHM recommendations, a parallel comparison with a usual care group was carried out over 1 year. The recruitment period started in April 2000 and ended 1 year later. Effectiveness was defined as the achievement of the low-density lipoprotein-cholesterol (LDL-C) reduction goals in patients with initial cardiovascular risk (CVR) >20% over 10 years (the goals being LDL-C <115 mg/dL for patients with coronary heart disease [CHD], or LDL-C <130 mg/dL for patients without CHD), or keeping CVR <20% at study end in patients with initial CVR <20%. The costs of treatments, visits, and laboratory assessments were estimated from the social perspective (year of costing 2002).
Methods
The ESCHM guidelines adapted by a steering committee included therapeutic recommendations directed to achieve LDL-C objectives in a cost-effective manner. To promote healthy cardiovascular lifestyles, items such as table cloths and magnets for the refrigerator (with relevant promotional messages) were distributed to intervention practices. All study physicians recorded the patients’ data in a specific-purpose application installed on their computer. In the case of intervention physicians, the CDSS was installed as an additional module of this application and they were requested to use it but were otherwise free to adopt or ignore the recommendations. Adherence to the guideline was monitored by the CDSS. Patients with hypercholesterolemia were selected from 44 general practices in Spain, mainly in the Catalonia region.
Main outcome measures and results
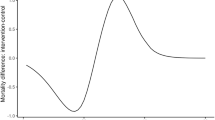
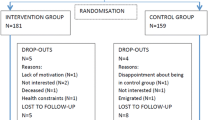
2221 patients were included in the study (1161 in usual care group and 1060 in the intervention group). The intervention was shown to be as effective as usual care, both in an unadjusted analysis and after adjusting for absolute CVR and previous treatment with lipid-lowering drugs (LLDs) [odds ratio (OR) 1.02; 95% CI 0.58, 1.77]. The intervention had no impact on lipid profiles. Intervention patients were prescribed LLDs less frequently than usual care patients (OR = 0.37; 95% CI 0.26, 0.52; p = 0.0001), particularly when CVR was low. This induced important savings in treatments (p = 0.0001) and total costs (p = 0.001), which were estimated as 24.9% and 20.8%, respectively. The intervention increased the number of laboratory analyses. The recommendations issued by the CDSS were accepted in 71.3% of the visits.
Discussion and conclusions
The CDSS based on the recommendations of the ESCHM did not modify the effectiveness of usual care but induced considerable savings.










Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Luepker RV. Current status of cholesterol treatment in the community: the Minnesota Heart Survey. Am J Med 1997; 102 (2 Pt A): 37–42
Shepherd J. A call to action. Eur Heart J 1998; 19 Suppl. M: M2–7
Frolkis JP, Zyzanski SJ, Schwartz JM, et al. Physician noncompliance with the 1993 National Cholesterol Education Program (NCEP-ATPII) guidelines. Circulation 1998; 98: 851–5
Lai LL, Poblet M, Bello C. Are patients with hyperlipidemia being treated? Investigation of cholesterol treatment practices in an HMO primary care setting. South Med J 2000; 93: 283–6
Straka RJ, Taheri R, Cooper SL, et al. Assessment of hypercholesterolemia control in a managed care organization. Pharmacotherapy 2001; 21: 818–27
Xhignesse M, Laplante P, Grant AM, et al. Antiplatelet and lipid-lowering therapies for the secondary prevention of cardiovascular disease: are we doing enough? Can J Cardiol 1999; 15: 185–9
Villar B, Rodriguez C, Rodriguez C, et al. Secondary prevention of ischemic heart disease in the Ciudad Real province, Spain: effectiveness of lipid-lowering therapy in primary health care. Med Clin (Barc) 2000; 115: 321–5
De Velasco JA, Llargues E, Fito R, et al. Risk factor prevalence and drug treatment in coronary patients hospital discharge: results of a multicenter registry (3C programme). Rev Esp Cardiol 2001; 54: 159–68
Abookire SA, Karson AS, Fiskio J, et al. Use and monitoring of “statin” lipid-lowering drugs compared with guidelines. Arch Intern Med 2001; 161: 53–8
Ballesteros LC, San Martin MIF, Cuesta TS, et al. The cost of inadequate prescriptions for hypolipidaemic drugs. Pharmacoeconomics 2001; 19: 513–22
Cobos A, Jovell AJ, Garcia-Altes A, et al. Which statin is most efficient for the treatment of hypercholesterolemia? A cost-effectiveness analysis. Clin Ther 1999; 21: 1924–36
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285(19): 2586–97
Pasternak R. Adult Treatment Panel II versus Adult Treatment Panel III: what has changed and why? Am J Cardiol 2002; 89: 3C–7C
Maviglia SM, Teich JM, Fiskio J, et al. Using an electronic medical record to identify opportunities to improve compliance with cholesterol guidelines. J Gen Intern Med 2001; 16: 531–7
Headrick LA, Speroff T, Pelecanos HI, et al. Efforts to improve compliance with the National Cholesterol Education Program Guidelines: Results of a randomized controlled trial. Arch Intern Med 1992; 152: 2490–6
Braunwald E. Changing the practice of cardiovascular medicine. Atheroscler Suppl 2001; 2: 27–30
Stamos TD, Shaltoni H, Girard SA, et al. Effectiveness of chart prompts to improve physician compliance with the National Cholesterol Education Program guidelines. Am J Cardiol 2001; 88: 1420–3
Davidson MH. Strategies to improve Adult Treatment Panel III guideline adherence and patient compliance. Am J Cardiol 2002; 89: 8C–22C
Kris-Etherton PM, Taylor DS, Smiciklas WH, et al. High-soluble-fiber foods in conjunction with a telephone-based, personalized behavior change support service result in favorable changes in lipids and lifestyles after 7 weeks. J Am Diet Assoc 2002; 102: 503–10
Second Joint Task Force of European and Other Societies on Coronary Prevention. Prevention of coronary heart disease in clinical practice. Eur Heart J 1998; 19: 1434–503
Edwards SJL, Braunholtz DA, Lilford RJ, et al. Ethical issues in the design and conduct of cluster randomized controlled trials. BMJ 1999; 318: 1407–9
Soikos. Base de Dates de Costes Sanitarios SOIKOS, 2002
Vademecum Internacional de especialidades farmacéuticas y biológicas [online]. Available from URL: http://www.vademecum.medicom.es/paginas_htm/home.asp [Accessed 2002 Aug 8]
Anderson KM, Wilson PWF, Odell PM, et al. An updated coronary risk profile: a statement for health professionals. Circulation 1991; 83: 356–62
Simons LA, Levis G, Simons J. Apparent discontinuation rates in patients prescribed lipid-lowering drugs. Med J Aust 1996; 164: 208–11
Machin D, Campbell MJ. Statistical tables for the design of clinical trials. Oxford: Blackwell Scientific Publications, 1987
Kerry SM, Bland JM. Sample size in cluster randomisation. BMJ 1998; 316: 549
Kerry SM, Bland JM. The intracluster correlation coefficient in cluster randomisation. BMJ 1998; 316: 1455–60
Cobos A, Muñío S, Bigorra J. El consumo de estatinas en las comunidades autónomas de España: oportunidades para el ahorro. Aten Primaria 1999; 24: 188–93
Thompson SG, Barber A. How should cost data in pragmatic randomised trials be analysed? BMJ 2000; 320: 1197–200
Koch GG, Gansky SA. Statistical considerations for multiplicity in confirmatory protocols. Drug Inf J 1996; 30: 523–33
Durrington PN, Prais H, Bhatnagar D, et al. Indication for cholesterol-lowering medication: comparison of risk-assessment methods. Lancet 1999; 353: 278–81
Van Hout BA, Simoons ML. Cost-effectiveness of HMG coenzyme reductase inhibitors: whom to treat? Eur Heart J 2001; 22: 751–61
Griffin JP. The withdrawal of Baycol (cerivastatin). Adverse Drug React Toxicol Rev 2001; 20: 177–80
Fox J, Jones K. Lipid-lowering interventions in managed care settings. Am J Med 2001; 110: 24S–30S
Patel B, Perez E. A means to an end: an overview of a hyperlipidemia outcomes management program. Am J Med 2001; 110: 12S–6S
Latts LM. Assessing the results: phase 1 hyperlipidemia outcomes in 27 Health Plans. Am J Med 2001; 110: 17S–23S
Feachem RGA, Sekhri NK, White KL. Getting more for their dollar: a comparison of the NHS with California’s Kaiser Permanente. BMJ 2002; 324: 135–41
Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work?. Meta-analysis of published reports. BMJ 2002; 325: 925–32
Kupets R, Covens A. Strategies for the implementation of cervical and breast cancer screening of women by primary care physicians. Gynecol Oncol 2001; 83: 186–97
Phillips LS, Brach WT, Cook CB, et al. Clinical inertia. Ann Intern Med 2001; 135: 825–34
Acknowledgments
Cardiocare Research Group: Via M, Alegre J, Muñoz M, Steiner E, Alvarado C (ABS Molí Nou, Sant Boi, Spain); Barceló C, Gens M, Bobé F, Ferrández MC, Palacios L (ABS Salou, Salou, Spain); Vilalta J, Basora T, Manrique E, Garola MD, Fernández M (ABS Riera Miró-Reus 4, Reus, Spain); Donado-Mazarrón A, Campaní M, Moltó E, Folch S, Isach A, Costa B (ABS Reus 2, Reus, Spain); Casadevall de la Herrán J, Inglés MR, Orús MA, Manero S, Rodríguez JM, Estrada P, Omonte J (ABS Casc Antic, Barcelona, Spain); Sorribes M, de León MR (EAP Riu Nord i Riu Sud — 4, Sta. Coloma de Gramanet, Spain); Montaña LM, Latre LM, Royo JM, García M, Segarra M, Buera E, Aviñó T, Valen E (CAP Flix, Flix, Spain); Sancho A, Muñoz D, Morató T (ABS-1 Centre Can Mariné, Sta. Coloma de Gramanet, Spain); Marín J, Llobet P, Andreu M, Euba R, Iglesias PF (ABS Montroig del Camp, Montroig del Camp, Spain); Benet JM, Caballero JC (CAP Roquetes. ABS Garraf Rural, Roquetes de Mar, Spain); Palacio F, Dolz F, Boj J, Descàrrega R (CAP St Jordi — Reus III, Reus, Spain); Alvarez M, Pérez S (ABS La Llagosta, La Llagosta, Spain); Martos J, Calvera R, Antoja P, Canals J, Vila C (ABS Martorelles, Martorelles, Spain); Araque J, Benaiges D, Dobon A, Fuster J, Martínez MP, Moreno R, Perolada JF, Pintado JE, Tiñena F (ABS Móra La Nova, Móra la Nova, Spain); Aguilar LC, Maseda S, Ribera M (ABS Parets, Parets, Spain); Puig J (ABS Sabadell 7, Sabadell, Spain); González M, Roselló MD (EAP Raval Nord-ABS Dr. Sayé, Barcelona, Spain); Forn MC, Jiménez JR, Loscos J, Venarell MJ (ABS Agramunt, Agramunt, Spain); Moya A, Herranz M, Gálvez E, Batlle PJS, Salido A, Martínez I (ABS Castellar, Castellar del Vallés, Spain); García C (ABS Les Borges del Camp, Borges del Camp, Spain); Cabré JJ, García JM, Fugola JL, Martín F, Montañés MD, Sánchez-Oro MI (ABS Reus — 1, Reus, Spain); Cabré R, Casal R, MJ de Andrés, Gastón E, Hernández JM, Rodríguez R, Subirats R, Valldosera C (ABS Falset, Falset, Spain); Carmona M (CAP Sant Llorenç de Savall, Sant Llorenç de Savall, Spain); Guzmán MC (ABS La Salut, Badalona, Spain), Bertral C (ABS Anoia Rural-Igualada, Igualada, Spain); Viñas L, Pons J (ABS Tortosa Oest, Tortosa, Spain); Pujol R, Torras A, Cartero JM, Remón JL (ABS Tremp, Tremp, Spain); Olasolo S (ABS Castelldefels, Castelldefels, Spain); Simonet P, Villafáfila R, Bravo JL, García MC, Bentué C, Verduras MC (ABS Viladecans 2, Viladecans, Spain); Armengol F, Mateu RM, Ibars J, Teixido F, Adnan-Mahmud T (ABS Almenar-Alfarràs, Almenar-Alfarràs, Spain); García MG, Roig I (ABS Manresa 4-CAP Sagrada Familia, Manresa, Spain); Zambudio J, Espinós MC, Riera C, Vilarrubia M, Cantero X, Celles P (ABS Igualada urbà, Igualada, Spain); Masqué, Caballol, Rubio, Ramón (ABS Amposta, Amposta, Spain), García G, Clúa J, Dalmau MR (ABS Tortosa Est- El Temple, Tortosa, Spain); Garde A, Brossa A, Tobías J, Soler M, Vivancos R (ABS Manresa-CAP Plça Catalunya, Manresa, Spain); Pagès A, Hernández S, MD Gil (CAP Jaume I, Tarragona, Spain); Morales JA (ABS Borges Blanques, Borges Blanques, Spain); Martorell J, Granell J, Vera G, Camacho JM, Bobadilla ML, Camps I (ABS Cervera, Cervera, Spain); Comino J (ABS Terra Alta, Gandesa, Spain), Comino L (ABS Alt Camp Est, Nulles, Spain), Rosado A (CS San Andrés II, Villaverde Alto, Spain), Apecechea K, Martín A (EAP Linneo, Madrid, Spain), Castellanos FJ, González J (CS Potes-San Andrés I; Villaverde Alto, Spain); Segura R, MC Álvarez (CS Embajadores, Madrid, Spain).
Study supported by the Department of Outcomes Research & Disease Management, Novartis Farmacéutica SA, Spain.
The authors thank Silvia Muñío, Juan Bigorra from Novartis Farmacéutica SA, Spain, and the Agencia de Evaluación de Tecnologías Sanitarias for helpful discussions during the study design; Clara Pujol and Bonaventura Bolívar from the Fundación Gol I Gurina for their support to the study; and Gemma Gambús (Novartis Farmacéutica SA, Spain) and Jesús González (Agencia de Evaluación de Tecnologías Sanitarias) for the review of the final manuscript. We also thank Novartis Farmacéutica SA, Spain, for the funding of the study.
Albert Cobos and Salvador Bergoñón were employed by RDES, SL, the contract research organization that conducted this study. Christina Espinosa and Eva Torremadé were employed by Novartis Farmacéutica SA, Spain. All remaining co-authors were contracted as consultants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cobos, A., Vilaseca, J., Asenjo, C. et al. Cost Effectiveness of a Clinical Decision Support System Based on the Recommendations of the European Society of Cardiology and Other Societies for the Management of Hypercholesterolemia. Dis-Manage-Health-Outcomes 13, 421–432 (2005). https://doi.org/10.2165/00115677-200513060-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200513060-00007