Abstract
Background: Spontaneous reporting of adverse drug reactions (ADRs) is fundamental to drug safety surveillance (pharmacovigilance); however, substantial under-reporting exists and is the main limitation of the system. Several factors could favour under-reporting.
Objective: The aim of this pilot study was to assess the effect of regular visits of a Clinical Research Assistant (CRA) on the improvement of ADR reporting in non-university hospitals.
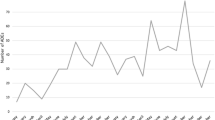
Methods: We set up an ADR report collecting system that involved regular visits by a CRA to non-university hospitals, which was similar to a system that already existed in university hospitals in Toulouse, France. Two areas in our region were chosen: Haute Garonne and Gers. We compared firstly the reporting rate (number of reports/number of beds) of total ADRs (i.e. spontaneously reported ADRs plus solicited ADRs collected by the CRA) and secondly, the percentage of serious ADRs reported by non-university hospitals in these two areas, in 2005 (the year prior to CRA visits) and after the start of CRA visits (2006 until the end of December 2008). We also compared the reporting rate of total ADRs in Haute Garonne and Gers non-university hospitals with those reported during the same period with a control group (the Ariège area, which has a similar number of beds to Gers and that was not visited by the CRA). The characteristics of ADRs collected by the CRA were also described.
Results: A total of 687 reports were collected by the CRA: 40% were classified as serious, including two deaths. The number of ADRs and the reporting rate increased significantly between 2005 and 2008 in non-university hospitals of Haute-Garonne and Gers, but not in Ariège. In Gers, the reporting rate was 3% in 2005 and 25% in 2008. In Haute-Garonne, the reporting rate was 11% in 2005 and 40% in 2008. The difference between the number of spontaneous and solicited reports also increased.
Conclusions: This study shows that regular visits by a CRA increases the number of ADRs collected by a Regional Pharmacovigilance Centre. Another interesting consequence was the rise in spontaneous reporting by healthcare professionals following the set-up of this system. Further assessment of this procedure is necessary for the long-term evaluation of its effectiveness.




Similar content being viewed by others
References
Pouyanne P, Haramburu F, Imbs JL, et al. Admissions to hospital caused by adverse drug reactions: cross sectional incidence study [letter]. French Pharmacovigilance Centres. BMJ 2000; 320: 1036
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18820 admissions. BMJ 2004; 329: 15–9
Moore N, Kreft-Jais C, Dhanani A. Spontaneous reporting: France. In: Mann RD, Andrews E, editors. Pharmacovigilance. 2nd ed. Chichester: John Wiley and Sons, Ltd, 2007: 217–26
Décret n∘95-278 du 13 mars 1995 relatif à la pharmacovigilance et modifiant le code de la santé publique. J Officiel du 14 mars 1995: 3935–8
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet 2000; 356: 1255–9
Figueiras A, Tato F, Fontainas J, et al. Influence of physicians’ attitudes on reporting adverse events. Med Care 1999; 37: 809–14
Eland IA, Belton KJ, Van Grootheest AC, et al. Attitudinal survey of voluntary reporting of adverse drug reactions. Br J Clin Pharmacol 1999; 48: 623–7
Irujo M, Beitia G, Bes-Rastrollo M, et al. Factors that influence under-reporting of suspected adverse drug reactions among community pharmacists in a Spanish region. Drug Saf 2007; 30: 1073–82
Herdeiro MT, Figueiras A, Polonia J, et al. Physicians’ attitudes and adverse drug reaction reporting: a case-control study in Portugal. Drug Saf 2005; 28: 825–33
Herdeiro MT, Figueiras A, Polonia J, et al. Influence of pharmacists’ attitudes on adverse drug reaction reporting: a case-control study in Portugal. Drug Saf 2006; 29: 331–40
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of under-reporting of adverse drug reactions: a systematic review. Drug Saf 2009; 32: 19–31
Bateman DN, Lee A, Rawlins MS, et al. Geographical differences in adverse drug reactions reporting rates in the northern region. Br J Clin Pharmacol 1991; 31: 188–9
Sacilotto K, Bagheri H, Lapeyre-Mestre M, et al. Adverse drug effect notifications by nurses and comparison with cases reported by physicians. Thérapie 1995; 5: 455–8
Begaud B, Evreux JC, Jouglard J, et al. Imputation of the unexpected or toxic effects of drugs: actualization of the method used in France. Thérapie 1985; 40: 111–8
Bürki F, Badie K, Bartoli P, et al. Reversible posterior leukoencephalopathy syndrome associated with bevacizumab/ doxorubicin regimen. Br J Clin Pharmacol 2008; 65: 793–4
Pedros C, Vallano A, Cereza G, et al. An intervention to improve spontaneous adverse drug reaction reporting by hospital physicians. Drug Saf 2009; 32: 77–83
Herdeiro MT, Polonia J, Gestal-Otero JJ, et al. Improving the reporting of adverse drug reaction: a cluster-randomized trial among pharmacists in Portugal. Drug Saf 2008; 31: 335–44
Ekman E, Bäckström M. Attitudes among hospital physicians to the reporting of adverse drug reactions in Sweden. Eur J Clin Pharmacol 2009; 65: 43–6
Castel JR, Figueras A, Pedros C, et al. Stimulating adverse drug reaction reporting: effect of a drug safety bulletin and of including yellow cards in prescription pads. Drug Saf 2003; 26: 1049–55
Feely J, Moriarty S, O’Connor P. Stimulating reporting of adverse drug reaction by using a fee. BMJ 1990; 300: 22–3
Bäckstrom A, Mjörndal T. A small economic inducement to stimulate increased reporting of adverse drug reactions: a way of dealing with an old problem? Eur J Clin Pharmacol 2006; 62: 381–5
Bäckström M, Ekman E, Mjörndal T. Adverse drug reaction reporting by nurses in Sweden. Eur J Clin Pharmacol 2007; 63: 613–8
Ranganathan SS, Houghton JE, Davies DP, et al. The involvement of nurses in reporting suspected adverse drug reactions: experience with the meningococcal vaccination scheme. Br J Clin Pharmacol 2003; 56: 658–63
Morrison-Griffiths S, Walley TJ, Park BK, et al. Reporting of adverse drug reactions by nurses. Lancet 2003; 9366: 1347–8
Ramsay LE. Bridging the gap between clinical pharmacology and rational drug prescribing. Br J Clin Pharmacol 1993; 35: 575–6
Acknowledgements
The authors would like to thank the Regional Agency of Hospitalisations of Midi-Pyrénées who financially supported the project, as well as the Regional Commission for Coordination of Health Vigilances, who helped to organize the work.
The authors have no conflicts of interest to declare that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gony, M., Badie, K., Sommet, A. et al. Improving Adverse Drug Reaction Reporting in Hospitals. Drug-Safety 33, 409–416 (2010). https://doi.org/10.2165/11319170-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11319170-000000000-00000