Abstract
Background: Lacosamide is an antiepileptic drug (AED) approved for the adjunctive treatment of partial-onset seizures in adults. Completed phase II/III clinical trials of lacosamide provide a valuable opportunity to evaluate clinically relevant aspects of the resulting large patient pool.
Objective: To provide insight into the clinical utility of lacosamide by performing a priori-defined and post hoc analyses on a large, pooled patient population.
Study Design: Pooled data from three randomized, double-blind, multicentre, placebo-controlled phase II/III trials.
Patients: Adult patients with partial-onset seizures with or without secondary generalization (N = 1294).
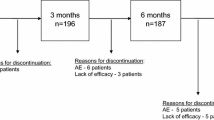
Intervention: Four- to six-week titration followed by 12-week maintenance treatment with lacosamide (Vimpat®) 200, 400 or 600mg/day or placebo.
Main Outcome Measure: A priori- defined primary efficacy variables for the pooled analysis were change in seizure frequency per 28 days and the proportion of patients experiencing a ≥50% reduction in seizure frequency (50% responder rate) from Baseline to the Maintenance Phase; a priori-defined secondary efficacy variables were the proportion of patients achieving a ≥75% reduction in seizure frequency from Baseline to the Maintenance Phase (75% responder rate), the proportion of Maintenance Phase completers remaining seizure free throughout the entire Maintenance Phase and the percentage of seizure-free days during the Maintenance Phase for patients entering the Maintenance Phase. The pooled analyses of the change in seizure frequency, and 50% and 75% responder rates were performed with an intent-to-treat (ITT) approach, including all patients receiving at least one dose of trial medication and having at least one post-baseline efficacy assessment. Similar analyses of the two primary efficacy variables and 75% responder rates were also performed using a modified ITT population (ITTm) that included ITT patients who entered the Maintenance Phase. Additional post hoc efficacy analyses were an evaluation of onset of efficacy and assessment of efficacy in patients grouped by prior surgical history and individual concomitant AED use. In addition, pharmacokinetic-pharmacodynamic modelling was performed, and safety data were assessed.
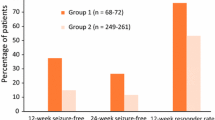
Results: In this pooled analysis of 1294 difficult-to-treat patients, all three dosages of lacosamide (200, 400 and 600 mg/day) showed a significant improvement compared with placebo for median percent seizure reduction (ITT and ITTm; p < 0.05 for 200 mg/day, p < 0.001 for 400 and 600 mg/day), as well as for 50% responder rate (ITT and ITTm; p <0.05 for 200 mg/day, p<0.001 for 400 and 600 mg/day). Evaluation of 75% responder rate in the phase II/III pooled population showed that a significantly higher proportion of patients randomized to lacosamide 400 or 600 mg/day achieved a ≥75% reduction in seizure frequency compared with placebo (ITT and ITTm; p < 0.001); statistical significance was not observed for lacosamide 200 mg/day (ITT and ITTm). A total of 2.7%, 3.3% and 4.8% of patients completing the Maintenance Phase in the lacosamide 200, 400 and 600 mg/day groups, respectively, experienced no seizures throughout the entire Maintenance Phase (placebo group = 0.9%). The mean change from baseline in the percentage of seizure-free days in patients entering the Maintenance Phase for the phase II/III pool was 8.0%, 11.6% and 14.7% with lacosamide 200 (p =0.077), 400 (p<0.001) and 600 (p<0.001) mg/day groups, respectively, compared with 6.1% in the placebo group.
The onset of efficacy relative to placebo was evident by the first week of treatment with lacosamide. Efficacy was similar in lacosamide-treated patients reporting prior surgical intervention for epilepsy compared to lacosamidetreated patients with no prior surgical intervention. Lacosamide showed a reduction in seizures, regardless of the concomitant AEDs used. The preferred pharmacokinetic-pharmacodynamic model (Emax) supported the therapeutic dose range of lacosamide, and no additional safety concerns were identified in the phase II/III pooled analysis.
Conclusions: Results of these a priori-defined and post hoc pooled data analyses from phase II/III trials demonstrate that lacosamide effectively reduces seizures in patients at all three dosages evaluated with an early onset of efficacy, regardless of patient surgical history and concomitant AED regimen.









Similar content being viewed by others
References
Bravata DM, Olkin I. Simple pooling versus combining in meta-analysis. Eval Health Prof 2001 Jun; 24(2): 218–30
VIMPAT® (lacosamide): US prescribing information. Smyrna (GA): UCB, Inc., 2008
VIMPAT®: summary of product characteristics for lacosamide. Belgium: UCB Pharma, S.A., 2008
Beyreuther BK, Freitag J, Heers C, et al. Lacosamide: a review of preclinical properties. CNS Drug Rev 2007; 13(1): 21–42
Ben-Menachem E, Biton V, Jatuzis D, et al. Efficacy and safety of oral lacosamide as adjunctive therapy in adults with partial-onset seizures. Epilepsia 2007 Jul; 48(7): 1308–17
Halász P, Kälviäinen R, Mazurkiewicz-Beldzińska M, et al. Adjunctive lacosamide for partial-onset seizures: efficacy and safety results from a randomized controlled trial. Epilepsia 2009 Mar; 50(3): 443–53
Chung S, Sperling MR, Biton V, et al. Lacosamide as adjunctive therapy for partial-onset seizures: a randomized controlled trial. Epilepsia 2010; 51(6): 958–67
Biton V, Fountain NB, Rosenow F, et al. Safety and tolerability of lacosamide: a summary of adverse events in epilepsy clinical trials [abstract]. Neurology 2009; 72(11 Suppl. 1): A225
Beydoun A, D’Souza J, Hebert D, et al. Lacosamide: pharmacology, mechanisms of action and pooled efficacy and safety data in partial-onset seizures. Expert Rev Neurother 2009 Jan; 9(1): 33–42
Chung SS. Lacosamide: new adjunctive treatment option for partial-onset seizures. Expert Opin Pharmacother 2010 Jun; 11(9): 1595–602
Ben-Menachem E, Chung S, Rudd D, et al. Evaluation of lacosamide efficacy in subjects with partial-onset seizures across the dose range used in phase II/III clinical trials [abstract]. Neurology 2009 Jun 28–Jul 2; 72(11 Suppl. 1): A329
French J, Brodie M, Hebert D, et al. Evaluation of seizure freedom and 75% responder rates with lacosamide in subjects with partial-onset seizures in phase II/III clinical trials. Innsbruck Colloquium on Status Epilepticus; 2009 Apr 2–4; Innsbruck
Gazzola DM, Balcer LJ, French JA. Seizure-free outcome in randomized add-on trials of the new antiepileptic drugs. Epilepsia 2007 Jul; 48(7): 1303–7
Sperling M, Rudd D, Hebert D, et al. Early onset of efficacy in the initial weeks of treatment with lacosamide: a pooled analysis of three phase II/III trials. Neurology 2009; 72(11 Suppl. 1): A352
Benbadis S, Elger C, Hebert D, et al. Efficacy of adjunctive lacosamide in patients with partial-onset seizures and prior surgical interventions for epilepsy. American Epilepsy Society (AES) 63rd Annual Scientific Conference; 2009 Dec 4–8; Boston (MA)
Rosenfeld WRD, Hebert D, Doty P. Lacosamide efficacy is independent of concomitant AED(s) treatment [abstract]. Neurology 2009; 72(11 Suppl. 1): A353
Schiller Y, Najjar Y. Quantifying the response to antiepileptic drugs: effect of past treatment history. Neurology 2008 Jan 1; 70(1): 54–65
Abou-Khalil B. Levetiracetam in the treatment of epilepsy. Neuropsychiatr Dis Treat 2008 Jun; 4(3): 507–23
Chung S. Third-generation antiepileptic drugs for partialonset seizures: lacosamide, retigabine, and eslicarbazepine. Eur Neurol J 2009; 1(1): 1–11
Cretin B, Hirsch E. Adjunctive antiepileptic drugs in adult epilepsy: how the first add-on could be the last. Expert Opin Pharmacother 2010 May; 11(7): 1053–67
Gil-Nagel A, Zaccara G, Baldinetti F, et al. Add-on treatment with pregabalin for partial seizures with or without generalisation: pooled data analysis of four randomised placebo-controlled trials. Seizure 2009 Apr; 18(3): 184–92
Peeters K, Adriaenssen I, Wapenaar R, et al. A pooled analysis of adjunctive topiramate in refractory partial epilepsy. Acta Neurol Scand 2003 Jul; 108(1): 9–15
Acknowledgements
Individual trials as well as pooled analyses were supported by SCHWARZ Biosciences Inc. and SCHWARZ Biosciences GmbH, members of the UCB group. Steve Chung, MD, is a consultant for Medtronics, Inc., GlaxoSmithKline plc. and UCB S.A., is on the speaker’s bureaux of Cyberonics, Inc., GlaxoSmithKline plc. and UCB S.A., and receives grant and research support from Schwarz Pharma A.G., GlaxoSmithKline, UCB S.A., Valeant, Eisai Inc., Ortho-McNeil and Medtronics, Inc. Elinor Ben-Menachem, MD, PhD has taken honorarium for speaking for UCB S.A., Janssen-Cilag EMEA, Bial, Eisai Inc. and Valeant, and has received support from Cyberonics, Inc., Bial, Eisai Inc., Pfizer Inc., Johnson & Johnson Inc. and UCB S.A. She has also served as a paid consultant for UCB S.A., Eisai Inc., Bial, Valeant and Sanofi-Aventis. Michael Sperling, MD, is a consultant for Dainippon Sumitomo Pharma Co., Ltd. and Valeant, is on the speaker’s bureaux of Pfizer, Eisai Inc. and UCB S.A., and receives research support from UCB S.A. and Schwarz Pharma A.G., NeuroPace, Inc., Medtronics, Inc., Eisai Inc., Johnson & Johnson Inc. and Marinus Pharmaceuticals, Inc. William Rosenfeld, MD, receives research support from UCB Pharma, Eisai, SCHWARZ Biosciences, Valeant, Medtronics, Inc., King Pharmaceuticals, Lundbeck, Johnson & Johnson PRD, Sepracor, Vertex and Upsher Smith, is on the speaker’s bureaux for UCB Pharma and Lundbeck and is a consultant for UCB Pharma. Nathan Fountain, MD, receives research support from UCB, SCHWARZ Biosciences, Vertex, Sepracor, Neuropace, Medtronics, Inc. and NIH. Selim Benbadis, MD, is a consultant for and on the speaker’s bureaux of Cyberonics, GlaxoSmithKline, Lundbeck, Pfizer, Spleepmed, UCB and XLTEK. David Hebert, PhD, Jouko Isojärvi, MD, PhD, and Pamela Doty, PhD, are employees of SCHWARZ Biosciences, a member of the UCB group. The authors gratefully acknowledge Willi Cawello, PhD, of SCHWARZ Biosciences GmbH, for his expertise and assistance with the manuscript. Full medical writing assistance was supported by UCB and was provided by Jennifer Hepker, PhD, of Prescott Medical Communications Group (Chicago, IL, USA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, S., Ben-Menachem, E., Sperling, M.R. et al. Examining the Clinical Utility of Lacosamide. CNS Drugs 24, 1041–1054 (2010). https://doi.org/10.2165/11586830-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11586830-000000000-00000