Abstract
Background: Paracetamol (acetaminophen) is the most common cause of acute liver failure (ALF). ALF attributed to paracetamol is most often associated with the following features: an unintentional overdose, a single product, an opioid-paracetamol combination, duration of <7 days, and a median dose of 7.5 g/day. Currently, the recommended maximum daily dose of paracetamol is 4 g.
Objectives: The aims of the study were to determine opioid-paracetamol prescription patterns, including prescriptions exceeding the recommended dose of paracetamol (4 g/day) [prescriptions and beneficiaries]; examine factors associated with receiving opioid-paracetamol prescriptions in excess of paracetamol 4 g/day; and evaluate opioid-paracetamol prescription patterns for beneficiaries with liver dysfunction.
Methods: A retrospective cohort study examining prescription data of 4.8 million beneficiaries from a US health benefits organization from 1 January 2009 through 31 December 2009. The main outcomes examined were daily paracetamol dose and liver dysfunction.
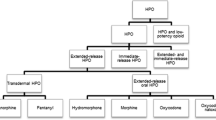
Results: A large proportion (8.1%) of the 5.3 million prescriptions for opioid-paracetamol exceeded the recommended maximum daily dose of paracetamol (4 g/day), putting over one-quarter of a million (255 123 [18.9%]) of the 1.35 million beneficiaries receiving an opioid-paracetamol prescription at risk of toxicity. The most frequently prescribed products that exceeded paracetamol dose guidelines contained dextropropoxyphene and hydrocodone. Multiple factors, including type of product (i.e. dextropropoxyphene or oxycodone-containing), geographical location (Midwest), strength of the paracetamol in the opioid-paracetamol product (>325 mg) and prescriber specialty (dentist, physician assistant), were associated with high-dose paracetamol prescriptions. Liver dysfunction was diagnosed in 3818 cases, and 23.4% of these beneficiaries received an opioid-paracetamol prescription in the 90 days prior to the liver dysfunction diagnosis.
Conclusions: Although most opioid-paracetamol prescriptions are written and dispensed for <4 g/day of paracetamol, a significant portion of beneficiaries are being prescribed and dispensed excessive doses of paracetamol. Efforts to curtail this practice may involve provision of prescriber and pharmacist education, utilization of benefit manager systems to flag excessive dosing or that require confirmation of dosing, and implementation of US FDA recommendations supported by these data.




Similar content being viewed by others
References
Kaufman DW, Kelly JP, Rosenberg L, et al. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA 2002; 287: 337–44
Amar PJ, Schiff ER. Acetaminophen safety and hepatotoxicity: where do we go from here? Expert Opin Drug Saf 2007; 6: 341–55
Lee WM. Acetaminophen toxicity: changing perceptions on a social/medical issue. Hepatology 2007; 46: 966–70
Watkins PB, Kaplowitz N, Slattery JT, et al. Aminotrans-ferase elevations in healthy adults receiving 4 grams of a-cetaminophen daily: a randomized controlled trial. JAMA 2006; 296: 87–93
Larson AM, Polson J, Fontana RJ, et al., for the Acute Liver Failure Study Group. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology 2005; 42: 1364–72
Escorsell A, Mas A, de la Mata M. Acute liver failure in Spain: analysis of 267 cases. Spanish Group for the Study of Acute Liver Failure. Liver Transplant 2007; 13: 1389–95
Ostapowicz G, Fontana RJ, Schiodt FV, et al., for the US Acute Liver Failure Study Group. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002; 137: 947–54
Krenzelok EP. The FDA acetaminophen advisory committee meeting: what is the future of acetaminophen in the United States? The perspective of a committee member. Clin Toxicol 2009; 47: 784–9
US Food and Drug Administration. FDA limits acetaminophen in prescription combination products: requires liver toxicity warnings. 2011 Jan 13 [online]. Available from URL: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm239894.htm [Accessed 2011 Feb 24]
Mort JR. High dose acetaminophen in narcotic combinations: should there be a concern? S D Med 2008; 61: 294–5
Centers for Medicare & Medicaid Services. Diagnosis and procedure codes: abbreviated and full code titles [online]. Available from URL: https://www.cms.gov/icd9providerdiagnosticcodes/06_codes.asp [Accessed 2011 Sep 1]
Myers RP, Lung Y, Shaheen AA, et al. Validation of ICD-9-CM/ICD-10 coding algorithms for the identification of patients with acetaminophen overdose and hepatotoxicity using administrative data. BMS Health Services Research 2007; 7: 159
Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986; 73(1): 13–22
Barthlow M. Top 200 prescription drugs of 2009. Pharmacy Times [online]. Available from URL: http://www.pharmacytimes.com/publications/issue/2010/May2010/RxFocusTopDrugs-0510 [Accessed 2011 Sep 1]
Pletcher MJ, Kertesz SG, Kohn MA, et al. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA 2008; 299: 70–8
Bower WA, Johns M, Margolis HS, et al. Population-based surveillance for acute liver failure. Am J Gastroenterol 2007; 102: 2459–63
Micromedex® Healthcare Series. Internet database (updated periodically). Greenwood Village, CO: Thomson Healthcare [online]. Available from URL: http://www.thomsonhc.com/hcs/librarian [Accessed 2011 Sep 12]
Albertson TE, Walker VM, Stebbins MR, et al. A population study of the frequency of high-dose acetaminophen prescribing and dispensing. Ann Pharmacother 2010; 44: 1191–5
Mort JR, Aparasu RR. Prescribing of potentially inappropriate psychotropic medications to ambulatory elderly. Arch Intern Med 2000; 160: 2825–31
Goulding MR. Inappropriate medication prescribing for elderly ambulatory care patients. Arch Intern Med 2004; 164: 305–12
US Food and Drug Administration. Propoxyphene: withdrawal — risk of cardiac toxicity. 2010 Nov 19 [online]. Available from URL: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm234389.htm [Accessed 2010 Nov 23]
Rancourt C, Moisan J, Baillargeon L, et al. Potentially inappropriate prescriptions for older patients in long-term care. BMC Geriatr 2004; 4: 9
Aparasu RR, Mort JR. Prevalence, correlates, and associated outcomes of potentially inappropriate psychotropic use in the community-dwelling elderly. Am J Geriatr Pharmacother 2004; 2: 102–11
Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther 2007; 32: 113–21
Hornsby LB, Whitely HP, Hester EK, et al. Survey of patient knowledge related to acetaminophen recognition, dosing, and toxicity. J Am Pharm Assoc 2010; 50: 485–9
Acknowledgements
All authors have no financial disclosures, and no funding/ support was received for this study. Drs Lilian Ndehi, Yihua Xu and Jane Stacy are employees of Humana, Inc., and Jane Stacy owns stock in Humana, Inc. Jane Mort and Olayinka Shiyanbola have no conflicts of interest to declare that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mort, J.R., Shiyanbola, O.O., Ndehi, L.N. et al. Opioid-Paracetamol Prescription Patterns and Liver Dysfunction. Drug-Safety 34, 1079–1088 (2011). https://doi.org/10.2165/11593100-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11593100-000000000-00000