Published online Nov 14, 2008. doi: 10.3748/wjg.14.6578
Revised: July 19, 2008
Accepted: July 26, 2008
Published online: November 14, 2008
A 17-year-old gentleman was admitted to our hospital for headache, the differential diagnosis of which included Behçet’s syndrome (BS). He developed an acute abdomen and was found to have air under the diaphragm on erect chest X-ray. Subsequent laparotomy revealed multiple perforations throughout the colon. This report describes an unusual complication of Behcets syndrome occurring at the time of presentation and a review of the current literature of reported cases.
- Citation: Dowling CM, Hill AD, Malone C, Sheehan JJ, Tormey S, Sheahan K, McDermott E, O’Higgins NJ. Colonic perforation in Behçet’s syndrome. World J Gastroenterol 2008; 14(42): 6578-6580
- URL: https://www.wjgnet.com/1007-9327/full/v14/i42/6578.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6578
Behçet’s syndrome (BS) is a multisystemic vasculitic disorder which can affect a number of different systems. It was first described by the Turkish dermatologist, Halushi Behçet in 1937, who described a triad of oral ulceration, genital ulceration and ocular inflammation[1]. BS is now recognized as a chronic, inflammatory, multisystemic disorder, which relapses in nature. It is a vasculitic process which can affect large and small vessels of both the venous and arterial systems[2].
Manifestations of BS are widespread and varied, the most common of which are cutaneous including oral and genital ulceration, erythema nodosum, pyoderma gangrenosum and many more. Up to half of patients will have musculoskeletal complications which include arthralgia and arthritis[3]. The diagnosis of BS is made using major and minor criteria devised by the International Study Group Criteria for Behçets disease in 1990[4]. The disease mainly affects young males and has a higher prevalence along the historic “silk route”, i.e. from the eastern rim of Asia to the Eastern Mediterranean[5].
Gastrointestinal symptoms, such as nausea, vomiting and abdominal pain, can sometimes occur, but the presence of intestinal ulceration is rare (< 1%)[6]. Our report describes a case of extensive colonic perforation due to intestinal involvement.
A 17-year-old man was admitted to the Accident and Emergency Department due to a six-week history of occipital headache associated with vomiting and poor balance. He also reported decreased appetite and weight loss of approximately 28 lbs over a two-month period. He described transient tender skin nodules, which were present on the anterior tibial area, eight weeks prior to presentation. On direct questioning, he did reveal that he had oral ulceration previously, but this resolved spontaneously. Background medical history was unremarkable, as was his family history.
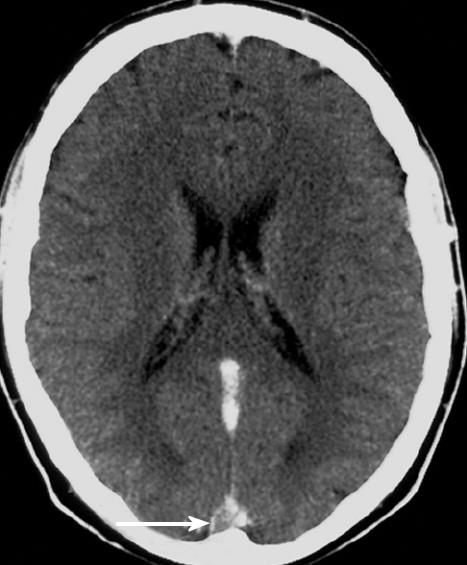
On examination in the Emergency Department, he appeared unwell. However, all his vital signs were within normal limits. Positive findings on examination included bilateral papilloedema and a seventh lower motor neuron lesion. There was bilateral scarring anteriorly on his skins. There was no evidence of oral or genital ulceration and abdominal examination at this time was normal. Hematological investigations were essentially normal except for a raised C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) at 119 mg/L and 84 mm/h, respectively. Further investigations performed included a lumbar puncture, Ziehl-Neelsen stain, autoantibody and infectious mononucleosis screen, all of which were non-contributory. He proceeded to have a CT brain and magnetic resonance studies, which demonstrated evidence of cerebral venous thrombosis. The “Empty Delta” sign on the post contrast MRI image is a characteristic finding in cerebral venous thrombosis (Figure 1).
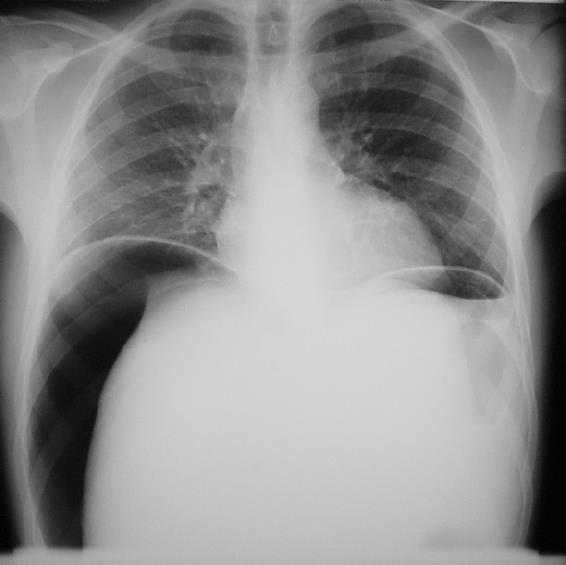
A working diagnosis of vasculitis was formulated at this stage and the patient was placed on anticoagulation and steroids with proton-pump inhibitor cover. His symptoms gradually improved, but on day eight, he developed acute abdominal pain. On examination, his abdomen was distended, diffusely tender with absent bowel sounds. An erect chest X-ray demonstrated air under the right hemidiaphragm (Figure 2).
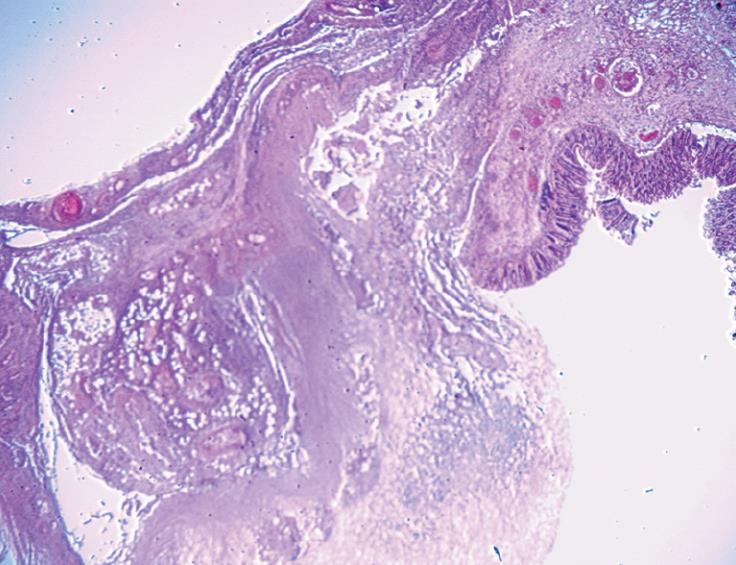
Marked fecal peritonitis was observed at laparotomy. There were five separate colonic perforations in the cecum, ascending, transverse and sigmoid colon. Surrounding these perforations were multiple areas of gangrenous colon with punched-out ulcerations extending throughout the colon to the level of the proximal sigmoid colon (Figure 3). A sub-total colectomy and terminal ileum resection with an end ileostomy were performed.
The histology specimen demonstrated a normal terminal ileum, but extensive ulceration in the proximal colon. The colon had numerous punched-out areas of ulceration, many of which were deeply penetrating with perforation. The intervening mucosa showed areas of normal mucosa. The distal segment of bowel, descending and sigmoid colon showed less ulceration than the proximal segment. However, there were nine distinct areas of necrosis, the largest of which was 2 cm in diameter. There was active inflammation with vasculitis, consistent with changes described in BS (Figure 4).
The patient made a good post-operative recovery, but developed a pelvic collection four weeks after the procedure. This was treated with a transrectal drain and intravenous antibiotic therapy. The patient was discharged home after a 51-d hospital stay on warfarin, azathioprine and a decreasing dose of corticosteroids. He remained well two months post discharge on immunosuppressant therapy.
BS involves the gastrointestinal tract in 10%-50% of patients, manifesting as diarrhoea, nausea, anorexia and abdominal pain. However, ulcerative changes are found in less than 1% of patients with BS[7]. Two types of ulceration can occur: localized and diffuse. Localized lesions tend to occur in the ileocaecal region, and are deep, often penetrating the serosal surface. In contrast, diffuse lesions are seen more commonly in the colon and may occur as multiple discrete, punched-out ulcers.
The main sites of involvement are the terminal ileum and cecum. Sometimes, BS can present with a cecal mass, anemia and weight loss, and thus mimick a cecal carcinoma[8]. In a recent literature review by Turan et al[9], the distribution of diffuse ulcers in twenty patients with BS was reviewed. Of these 20 patients, 9 had ulceration involving the entire colon, and only two cases (including their case) involved the sigmoid colon. Kyle et al[10] described the other case in 1991. Our case is the third reported case of sigmoid perforation in BS. In both previous cases, the diagnosis of BS was established. However, our case illustrates this rare complication at the time of presentation.
In a review by Kasahara et al[6], the most common site of involvement of the small intestine was the terminal ileum. Our case is also unusual in that the terminal ileum was unaffected.
BS often represents a diagnostic challenge, as an incomplete disease can be confused with other conditions which have similar clinical manifestations, for example inflammatory bowel disease (IBD). Not only do they share gastrointestinal manifestations, but the extra-intestinal features of both BS and IBD are very similar. Gastrointestinal disease in BS is associated with an overall poor prognosis, as approx 5%-10% will require surgery[3]. This poses a number of problems for patients with BS. Recurrent ulceration of the stoma is a relatively common complication, as is recurrence of disease adjacent to or at the surgical anastomosis. Most of these recurrent ulcers appear within two years of the resection. There are very few reports on the long term prognosis of intestinal BS. Naganuma et al[11] looked at 2-year follow-up in 20 patients with BS in Japan, and found that the postoperative recurrence rate is as high as 87.5%.
The pathergy phenomenon seen in BS, that is a cutaneous hyperreactivity following minor trauma[12], means that patients with BS are prone to problems at the incision site[13]. Fortunately, our patient has not experienced any such complications.
As BS is a relapsing condition, careful follow-up is necessary to detect any late complications or reactivation of disease. This report describes a rare complication of BS at the time of presentation, and highlights the importance of considering BS in the differential diagnosis of a complex patient presenting with such gastrointestinal manifestations.
Peer reviewer: Alessandro Fichera, MD, FACS, FASCRS, Assistant Professor, Department of Surgery-University of Chicago, 5841 S. Maryland Ave, MC 5031, Chicago, IL 60637, United States
S- Editor Zhong XY L- Editor Wang XL E- Editor Zheng XM
| 1. | Behçet H. Uber rezivirde, aphtose, durch virus verursachte. Geshwure am Mund, am Auge, und den Genitalien. Dermatol Wochenschr. 1937;1153-1157. [Cited in This Article: ] |
| 2. | Koç Y, Güllü I, Akpek G, Akpolat T, Kansu E, Kiraz S, Batman F, Kansu T, Balkanci F, Akkaya S. Vascular involvement in Behçet's disease. J Rheumatol. 1992;19:402-410. [Cited in This Article: ] |
| 3. | Bradbury AW, Milne AA, Murie JA. Surgical aspects of Behçet's disease. Br J Surg. 1994;81:1712-1721. [Cited in This Article: ] |
| 4. | International study group for Behcet’s disease. Criteria for diagnosis of Behcet’s disease. Lancet. 1990;335:1078-1080. [Cited in This Article: ] |
| 5. | O'Duffy JD. Behçet's syndrome. N Engl J Med. 1990;322:326-328. [Cited in This Article: ] |
| 6. | Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, Kuyama T. Intestinal involvement in Behçet's disease: review of 136 surgical cases in the Japanese literature. Dis Colon Rectum. 1981;24:103-106. [Cited in This Article: ] |
| 7. | Baba S, Maruta M, Ando K, Teramoto T, Endo I. Intestinal Behçet's disease: report of five cases. Dis Colon Rectum. 1976;19:428-440. [Cited in This Article: ] |
| 8. | Ha HK, Lee HJ, Yang SK, Ki WW, Yoon KH, Shin YM, Jung HY, Yu E, Lee SI, Kim KW. Intestinal Behçet syndrome: CT features of patients with and patients without complications. Radiology. 1998;209:449-454. [Cited in This Article: ] |
| 9. | Turan M, Sen M, Koyuncu A, Aydin C, Arici S. Sigmoid colon perforation as an unusual complication of Behçet's syndrome: report of a case. Surg Today. 2003;33:383-386. [Cited in This Article: ] |
| 10. | Kyle SM, Yeong ML, Isbister WH, Clark SP. Bechet's colitis: a differential diagnosis in inflammations of the large intestine. Aust N Z J Surg. 1991;61:547-550. [Cited in This Article: ] |
| 11. | Naganuma M, Iwao Y, Inoue N, Hisamatsu T, Imaeda H, Ishii H, Kanai T, Watanabe M, Hibi T. Analysis of clinical course and long-term prognosis of surgical and nonsurgical patients with intestinal Behçet's disease. Am J Gastroenterol. 2000;95:2848-2851. [Cited in This Article: ] |
| 12. | Gilhar A, Winterstein G, Turani H, Landau J, Etzioni A. Skin hyperreactivity response (pathergy) in Behçet's disease. J Am Acad Dermatol. 1989;21:547-552. [Cited in This Article: ] |
| 13. | Bozkurt M, Torin G, Aksakal B, Ataoglu O. Behçet's disease and surgical intervention. Int J Dermatol. 1992;31:571-573. [Cited in This Article: ] |