Published online Jan 7, 2009. doi: 10.3748/wjg.15.86
Revised: October 10, 2008
Accepted: October 17, 2008
Published online: January 7, 2009
AIM: To investigate prevalence of Clonorchis sinensis in patients with gastrointestinal symptoms, and the relation of the infection to hepatobiliary diseases in 26 hospitals in Korea.
METHODS: Consecutive patients who had been admitted to the Division of Gastroenterology with gastrointestinal symptoms were enrolled from March to April 2005. Of those who had been diagnosed with clonorchiasis, epidemiology and correlation between infection and hepatobiliary diseases were surveyed by questionnaire.
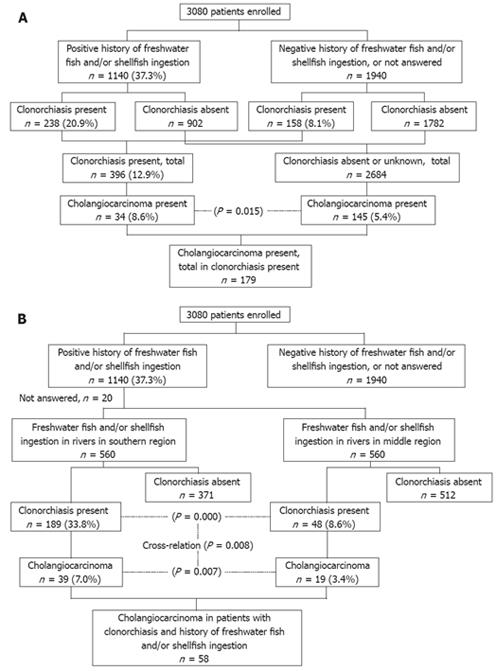
RESULTS: Of 3080 patients with gastrointestinal diseases, 396 (12.9%) had clonorchiasis and 1140 patients (37.2%) had a history of eating raw freshwater fish. Of those with a history of raw freshwater fish ingestion, 238 (20.9%) patients had clonorchiasis. Cholangiocarcinoma was more prevalent in C. sinensis-infected patients than non-infected patients [34/396 (8.6%) vs 145/2684 (5.4%), P = 0.015]. Cholangiocarcinoma and clonorchiasis showed statistically significant positive cross-relation (P = 0.008). Choledocholithiasis, cholecystolithiasis, cholangitis, hepatocellular carcinoma, and biliary pancreatitis did not correlate with clonorchiasis.
CONCLUSION: Infection rate of clonorchiasis was still high in patients with gastrointestinal diseases in Korea, and has not decreased very much during the last two decades. Cholangiocarcinoma was related to clonorchiasis, which suggested an etiological role for the parasite.
- Citation: Kim HG, Han J, Kim MH, Cho KH, Shin IH, Kim GH, Kim JS, Kim JB, Kim TN, Kim TH, Kim TH, Kim JW, Ryu JK, Moon YS, Moon JH, Park SJ, Park CG, Bang SJ, Yang CH, Yoo KS, Yoo BM, Lee KT, Lee DK, Lee BS, Lee SS, Lee SO, Lee WJ, Cho CM, Joo YE, Cheon GJ, Choi YW, Chung JB, Yoon YB. Prevalence of clonorchiasis in patients with gastrointestinal disease: A Korean nationwide multicenter survey. World J Gastroenterol 2009; 15(1): 86-94
- URL: https://www.wjgnet.com/1007-9327/full/v15/i1/86.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.86
Clonorchiasis is a parasitic infection caused by C. sinensis, and is one of the most prevalent endemic diseases in eastern Asia[1–3]. According to a report by World Health Organization (WHO) and International Agency for Research on Cancer in 1994, about 7 million people in the world were infected with C. sinensis[4]. In Korea, the stool egg-positive rate for C. sinensis has decreased dramatically from 4.6% in 1971 to 2.7% in 1986, after the introductioin of praziquantel, but the rate remained at 1.4% in 1997[56–8]. The high prevalence rate of clonorchiasis in Korea results from a long tradition of consuming raw freshwater fish and/or shellfish[9].
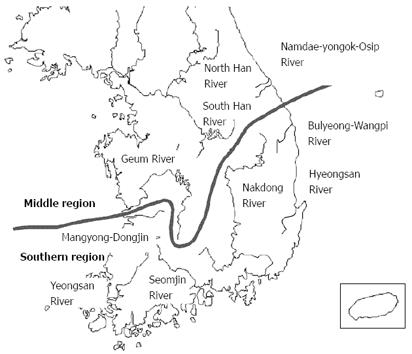
Infection rate in Korea differs from one major river basin to another. According to a national survey conducted in 1981, the stool egg-positive rate for C. sinensis in people of southern river basins (Nakdong, Yeongsan, and Seomjin Rivers) was 17%-40%, while that in people of middle river basins (Han, Geum, and Dangjim-Mankyong Rivers) was lower at 8%-12%[10]. However, there have been no data on infection rate among people in other river basins in middle and eastern areas (North Han, Bulyeong-Wangpi, and Namdae-Yeonggok-Osip Rivers).
Fecal examination for eggs has bee used in population-based studies for diagnosis of clonorchiasis[11]. However, this method has low sensitivity, which results in lower prevalence rates. Other methods for diagnosis include intradermal test using diluted antigens of C. sinensis[12], ELISA for circulating antibody against the parasite[13], radiological studies of the liver[14], and bile examination for eggs, metacercariae and cercariae. Of these, intradermal test is the easiest to perform, but has low specificity because of cross-reactivity with other parasites such as Paragonimus westermani[12]. Diffuse dilatation of the intrahepatic bile ducts detected by abdominal ultrasonography (US), computed tomography (CT), or cholangiography can easily establish clonorchiasis. In addition, detection of eggs in bile collected by endoscopic or percutaneous biliary drainage can lead to a definite diagnosis.
Adult worms of C. sinensis migrate from the common bile duct to peripheral intrahepatic bile duct, and remain there for 20-30 years causing chronic persistent infection[15]. In humans, clinical manifestations of light parasite loads are often asymptomatic. On the other hand, chronic infection with heavy parasite loads has been associated with various hepatobiliary diseases, such as biliary obstruction, recurrent pyogenic cholangitis[16], hepatolithiasis[17–21]. According to several experimental and clinical studies, clonorchiasis has been associated with carcinogenesis in the bile duct mucosa[41922]. Adult worms, eggs, or mucoid material after infection can also be the nidus of hepatolithiasis[162324]. Although there have been several studies on association between clonorchiasis and several hepatobiliary diseases, there has been no recent nationwide multicenter study in endemic areas and no investigation on prevalence and infection rates after raw freshwater fish and/or shellfish ingestion.
Therefore, we conducted a prospective nationwide multicenter study to investigate infection rate of C. sinensis in patients with gastrointestinal symptoms, and the relation of C. sinensis infection with hepatobiliary diseases in 26 secondary and tertiary hospitals in Korea.
This prospective study was conducted in 26 secondary and tertiary hospitals in South Korea from March to April 2005. Subjects included consecutive patients with gastrointestinal symptoms who were admitted to the Department of Internal Medicine during the study period. Gastrointestinal symptoms were defined as the presence of any of the following: nausea, vomiting, diarrhea, constipation, abdominal pain, heartburn, dyspepsia, jaundice, indigestion, and fecal incontinence. Patients were excluded if they had been admitted with non-gastrointestinal symptoms, admitted more than twice during the study period, unable to give a thorough history, < 14 years old, and declined to participate in this study.
The institutional review board of each participating hospital approved this study. Informed consent for participation in this study was obtained from each patient included in the study.
Upon admission, attending physicians filled out a structured questionnaire for each subject after a medical interview. The questionnaire included the following information: rivers nearest to the birthplace or place of current residence in order of decreasing duration, history of eating raw freshwater fish and/or shellfish, including the time, place and species of the fish and/or shellfish consumed, past history of clonorchiasis and treatment including type and duration, and past history of hepatobiliary diseases. Rivers nearest to the birthplace or place of current residence included 10 major rivers in South Korea: Nakdong, South Han, North Han, Geum, Yeongsan, Seomjin, Mangyong-Dongjin, Hyeongsan, Bulyeong-Wangpi, and Namdae-Yeongok-Osip.
The questionnaire also included close-ended questions such as: (1) did you (the patient him/herself) know that clonorchiasis can be acquired by ingesting raw freshwater fish? (2) Did you know that clonorchiasis can also be acquired by eating freshwater shellfish? (3) Did you know that clonorchiasis can be transmitted via kitchen knives and/or towels? (4) Did you know clonorchiasis can be transmitted by unwashed hands of raw freshwater fish handlers? (5) Did you know clonorchiasis can be prevented by eating fully cooked freshwater fish?
After admission, all the patients underwent laboratory tests, which included complete blood count with differential count, aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase, gamma-glutamyl transpeptidase (GGT), and total bilirubin. When transabdominal US or abdominal CT was done after admission or within 6 mo of admission, presence of dilatation of the intrahepatic bile ducts and/or extrahepatic bile duct was recorded.
Diagnosis of clonorchiasis was based on the presence of one or more of the following findings: (1) detection of C. sinensis eggs, metacercariae, or adult worms in stools collected during admission; (2) presence of induration with area of 60 mm2 or greater on the forearm after skin test with an intradermal injection of diluted crude antigen of C. sinensis; (3) positive for serum antibodies to C. sinensis using ELISA; (4) detection of C. sinensis eggs, metacercariae, or adult worms in bile collected during percutaneous transhepatic biliary drainage or endoscopic nasobiliary drainage; (5) finding of diffuse dilatation of intrahepatic bile ducts in transabdominal US, abdominal CT, or cholangiography; and (6) detection of C. sinensis infection in stools or bile examination, and/or presence of positive intradermal test described in medical records. To investigate the possible association between clonorchiasis and hepatobiliary diseases, medical records of each patient were reviewed for diagnosis of the following diseases: cholangitis, choledocholithiasis, gallbladder stones, hepatocellular carcinoma, cholangiocarcinoma, gallbladder cancer, biliary pancreatitis, and alcoholic pancreatitis.
Overall infection rate of C. sinensis and that according to the river basins were calculated. Infection rates between raw freshwater fish and/or shellfish eaters and non-eaters were also compared. Level of knowledge on transmission and prevention of clonorchiasis was assessed. By using the χ2 test and independent t test, the differences between infected and non-infected patients were assessed with regard to the presence of peripheral eosinophilia and abnormal liver function tests. Sensitivities of various diagnostic methods used in this study were evaluated.
Association with hepatobiliary diseases was evaluated for infected and non-infected patients by using the χ2 test. Association between clonorchiasis and cholangiocarcinoma among raw freshwater fish and/or shellfish eaters from high prevalence river basins (Nakdong, Yeongsan, Seomjin, and Hyeongsan Rivers) and lower prevalence river basins (the remainder) was assessed using the t test and odds ratio. After correction for regions, Cochran’s Mantel-Haenszel χ2 test was used to evaluate the association between clonorchiasis and cholangiocarcinoma. SPSS (version 12.0 for Windows; Chicago, IL, USA) was used for statistical analysis and P < 0.05 was considered statistically significant.
Subjects included 3080 patients from 26 hospitals. Number of patients according to rivers nearest to the birthplace or place of current residence was 947 (31.5%) in Nakdong, 774 (25.7%) in South Han, 270 (9.0%) in North Han, 303 (10.1%) in Geum, 137 (4.6%) in Yeongsan, 97 (3.2%) in Seomjin, 266 (8.8%) in Mangyong-Dongjin, 154 (4.8%) in Hyeongsan, six (0.2%) in Bulyeong-Wangpi, 64 (2.1%) in Namdae-Yeongok-Osip Rivers and 71 unanswered (Table 1). There were 1953 male and 1127 female patients. Male to female ratio was 1.7:1. Mean age of the patients was 58.2 years old (range, 14-98).
| Rivers | Number of patients |
| Nakdong | 947 (31.5) |
| South Han | 774 (25.7) |
| North Han | 270 (9.0) |
| Geum | 303 (10.1) |
| Yeongsan | 137 (4.6) |
| Seomjin | 97 (3.2) |
| Mangyong-Dongjin | 266 (8.8) |
| Hyeongsan | 145 (4.8) |
| Bulyeong-Wangpi | 6 (0.2) |
| Namdae-Yongok-Osip | 64 (2.1) |
| Not answered | 71 |
| Total | 3080 |
The number of patients with past history of raw freshwater fish and/or shellfish ingestion was 1140 (37.3%) out of 3055 of those who answered the questionnaire, while there were 191 (62.7%) patients with no past history of ingestion, and there were 25 unanswered questionnaires. Of those with a past history of ingestion, 156 out of 1140 patients (13.9%) ingested only once, 318 patients (28.3%) two to four times, and 648 patients (57.8%) more than five times. Initial time of raw freshwater fish and/or shellfish ingestion was within 10 years in 278 patients (25.5%), 11-20 years ago in 207 (19.0%), 21–30 years ago in 179 (16.4%), > 30 years ago in 427 (39.1%), and 49 questionnaires were unanswered (Table 2).
| Characteristics | Number of patients |
| History of ingestion | |
| Present | 1140 (37.3) |
| Frequency | |
| Once | 156 (13.9) |
| 2-4 times | 318 (28.3) |
| ≥ 5 times | 648 (57.8) |
| Unknown or not answered | 18 |
| Time of first ingestion | |
| 0-10 yr ago | 278 (25.5) |
| 11-20 yr ago | 107 (19.0) |
| 21-30 yr ago | 179 (16.4) |
| ≥ 30 yr ago | 427 (39.1) |
| Unknown or not answered | 49 |
| None | 1915 (62.7) |
| Not answered | 25 |
| Total | 3080 |
In 1140 patients with a past history of ingestion, river basins nearest to the place of ingestion were Nakdong for 394 patients (35.2%), South Han for 156 (13.9%), North Han for 207 (18.5%), Geum for 84 (7.5%), Yeongsan for 47 (4.2%), Seomjin for 65 (5.8%), Mangyong-Dongjin for 78 (7.0%), Hyeongsan for 54 (4.8%), Bulyeong-Wangpi for three (0.3%), Namdae-Yeongok-Osip Rivers for 32 (2.9%), and 20 questionnaires were unanswered (Table 3).
| River basins | Patients, n (%) | Infected patients (n) | Infection rate (%) |
| Nakdong | 394 (35.2) | 132 | 33.5 |
| South Han | 156 (13.9) | 12 | 7.7 |
| North Han | 207 (18.5) | 15 | 7.2 |
| Geum | 84 (7.5) | 7 | 8.3 |
| Yeongsan | 47 (4.2) | 19 | 40.4 |
| Seomjin | 65 (5.8) | 14 | 21.5 |
| Mangyong-Dongjin | 78 (7.0) | 10 | 1.8 |
| Hyeongsan | 54 (4.8) | 24 | 44.4 |
| Bulyeong-Wangpi | 3 (0.3) | 0 | 0 |
| Namdae-Yongok-Osip | 32 (2.9) | 4 | 12.5 |
| Not answered | 20 | 3 | |
| Total | 1140 | 238 | 20.9 |
Only 150 (5.0%) patients had been diagnosed with clonorchiasis in the past. The number of patients without a past history of diagnosis or treatment was 2880 (95.0%) and 50 questionnaires were unanswered. Of those 150 patients with a past history of clonorchiasis, 120 (81.6%) had received eradication therapy, 14 (9.5%) did not receive any therapy, 13 (8.8%) had undergone treatment without definite diagnosis, and three did not answer. There were 657 patients (21.3%) with a past history of hepato-biliary diseases. Of these patients, 395 (60.4%) had bile duct stones, 118 (18.1%) cholangitis, 64 (9.6%) cholangiocarcinoma, 116 (17.6%) jaundice of uncertain cause, and 112 (16.5%) pancreatitis.
Of 3049 patients who answered the questionnaire, 2464 (80.8%) knew that clonorchiasis can be acquired by ingesting raw freshwater fish and 1629 (53.3%) knew that clonorchiasis can also be acquired by eating raw freshwater shellfish. Also, 1141 (47.2%) knew that clonorchiasis can be transmitted via kitchen knives and/or towels and 1192 (39.1%) acknowledged that clonorchiasis can be transmitted by unwashed hands of raw freshwater fish handlers. In addition, 2371 patients (77.8%) knew that clonorchiasis can be prevented by eating fully cooked freshwater fish (Table 4).
| Questions | patients with “Yes”n (%) | Patients with “No”n (%) | Number of notanswered (n) |
| Did you (the patient him/herself) know that clonorchiasis can be acquired by ingesting raw freshwater fish? | 2464 (80.8) | 585 (19.2) | 31 |
| Did you know that clonorchiasis can also be acquired by eating freshwater shellfish? | 1626 (53.3) | 1423 (46.7) | 31 |
| Did you know that clonorchiasis can be transmitted via kitchen knifes and/or towels? | 1441 (47.3) | 1608 (52.7) | 31 |
| Did you know clonorchiasis can be transmitted by unwashed hands of raw freshwater fish handlers? | 1192 (39.1) | 1855 (60.9) | 33 |
| Did you know that clonorchiasis can be prevented by eating fully cooked freshwater fish? | 2371 (77.8) | 676 (22.2) | 33 |
Diagnosis of infection: Of 3080 patients admitted to the Department of Internal Medicine during the study period, 396 (12.9%) had been diagnosed with clonorchiasis. Stool examination was positive for C. sinensis eggs, metacercariae, or adult worms in 55 patients. Intradermal test was positive in 225 patients and serum antibodies to C. sinensis using an ELISA were positive in 157 patients. In 14 patients, C. sinensis eggs, metacercariae, or adult worms were detected in bile collected during percutaneous transhepatic biliary drainage or endoscopic nasobiliary drainage. Diffuse dilatation of intrahepatic bile ducts in transabdominal US, abdominal CT, or cholangiography was found in 34 patients. C. sinensis infection in stools or bile examination and/or presence of positive intradermal test was described in the medical records of 150 patients.
Sensitivities of the diagnostic tests were highest for intradermal test (74.5%) and second highest for serum antibodies to C. sinensis using an ELISA (43.4%) (Table 5).
| Diagnostic modalities | Infected persons, who were tested (n) | Positive results (n) | Sensitivity (%) |
| Fecal exam for eggs | 321 | 55 | 17.1 |
| ELISA for circulating antibody | 362 | 157 | 43.40 |
| Intradermal test | 302 | 225 | 74.50 |
| Examination of collected bile | 134 | 14 | 10.40 |
| Radiologic findings | 295 | 34 | 11.50 |
Among patients with clonorchiasis, there was no patient younger than 19 year old. There were seven patients (6.5%) out of 107 in their twenties, 25 (11.3%) out of 222 in their thirties, 79 (17.1%) out 463 in their forties, 99 (14.2%) out of 695 in their fifties, 113 (13.6%) out of 831 in their sixties, and 61 (10.6%) out of 575 in their seventies. There were 12 (7.5%) out of 161 patients older than 80 years (Table 6).
| Age group (yr) | Number of patients (n) | Number of patients with clonorchiasis |
| 0-19 | 26 | 0 (0) |
| 20-29 | 107 | 7 (6.5) |
| 30-39 | 222 | 25 (11.3) |
| 40-49 | 463 | 79 (17.1) |
| 50-59 | 695 | 99 (14.2) |
| 60-69 | 831 | 113 (13.6) |
| 70-79 | 575 | 61 (10.6) |
| ≥ 80 | 161 | 12 (7.5) |
| Total | 3080 | 396 |
Distribution of infected patients according to river basins from where ingested raw freshwater fishes originated: Of 1140 patients with a history of raw freshwater fish and/or shellfish ingestion, 238 (20.9%) had been diagnosed with clonorchiasis. Also, there was evidence of clonorchiasis in 157 out of 1940 patients (6.5%) who had no history of ingestion or had not answered the questionnaire (Table 7).
| Number of patients with clonorchiasis | |
| Total number of patients (n = 3080) | 396 (12.9) |
| Patients with positive history of raw freshwater fish ingestion (n = 1140) | 238 (20.9) |
| Patients without raw freshwater fish ingestion (n = 1940) | 158 (8.1) |
Of 1120 patients who answered, the river basin nearest to the place of raw freshwater fish or shellfish ingestion was Nakdong for 132 patients, South Han for 12 patients, North Han for 15 patients, Geum for seven patients, Yeongsan for 19 patients, Seomjin for 14 patients, Mangyong-Dongjin for 10 patients, Hyeongsan for 24 patients, Bulyeong-Wangpi for none, and Namdae-Yeongok-Osip Rivers for four patients (Table 4). The river basin with highest infection rate was Hyeongsan (44.4%). Other river basins in decreasing order of infection rate were Yeongsan (40.4%) and Nakdong (33.5%).
Laboratory findings: Eosinophilia in the peripheral blood (> 400/mm3) was found in 65 of 389 patients with clonorchiasis (16.7%), while it was found in 250 of 2617 patients (9.6%) without clonorchiasis (P = 0.000) (Table 8). Serum alkaline phosphatase was 304.8 ± 418.35 U/L in 382 patients with clonorchiasis, but 234.4 ± 350.81 U/L in 2611 patients without clonorchiasis
| Laboratory findings | With clonorchiasis (n = 396) | Without clonorchiasis (n = 2684) | P | ||
| Number of patients | mean ± SD | Number of patients | mean ± SD | ||
| Eosinophilia1 | 65 | NA | 250 | NA | 0 |
| AST (U/L) | 393 | 104.5 ± 269.56 | 2671 | 110.7 ± 263.59 | 0.665 |
| ALT (U/L) | 393 | 113.5 ± 254.01 | 2669 | 107.7 ± 258.17 | 0.68 |
| Alkaline phosphatase (U/L) | 382 | 304.8 ± 418.35 | 2611 | 234.4 ± 350.81 | 0.002 |
| γ-glutamyl transpeptidase (U/L) | 362 | 200.0 ± 261.19 | 2233 | 187.0 ± 440.01 | 0.585 |
| Total bilirubin (mg/dL) | 392 | 3.07 ± 17.246 | 2668 | 3.28 ± 5.401 | 0.81 |
(P = 0.002). However, levels of AST, ALT, GGT, and total bilirubin were not significantly different between the two groups (Table 8).
Association between clonorchiasis and hepato-biliary diseases: When prevalence of various hepatobiliary diseases was evaluated between patients with and without clonorchiasis, a statistically significant difference was found only for cholangiocarcinoma [34 (8.6%) vs 145 (5.4%), P = 0.015] (Figure 1A). There was no significant difference regarding cholangitis, bile duct stones, hepatitis, hepatocellular carcinoma, gallstone pancreatitis, and gallbladder cancer between patients with and without clonorchiasis (Table 9).
| Hepatobiliary diseases | Patients with clonorchiasis (n = 396) | Patients without clonorchiasis (n = 2684) | P |
| Cholangitis | 32 (8.0) | 242 (9.0) | NS |
| Bile duct stones | 92 (23.2) | 716 (26.7) | NS |
| Gallstone | 45 (11.4) | 340 (12.7) | NS |
| Intrahepatic bile duct stones | 13 (3.3) | 107 (4.0) | NS |
| Extrahepatic bile duct stones | 34 (8.6) | 269 (10.0) | NS |
| Hepatitis | 100 (25.3) | 650 (24.2) | NS |
| Hepatitis B virus | 58 (14.6) | 336 (12.5) | NS |
| Hepatitis C virus | 5 (1.3) | 66 (2.5) | NS |
| Alcoholic | 25 (6.3) | 159 (5.9) | NS |
| Toxic | 5 (1.3) | 40 (1.5) | NS |
| Autoimmune | 1 (0.3) | 5 (0.2) | NS |
| Other causes | 6 (1.5) | 44 (1.6) | NS |
| Hepatocellular carcinoma | 51 (12.9) | 391 (14.6) | NS |
| Cholangiocarcinoma | 34 (8.6) | 145 (5.4) | 0.015 |
| Gallbladder cancer | 9 (2.3) | 75 (2.8) | NS |
| Biliary pancreatitis | 6 (1.5) | 71 (2.6) | NS |
Patients were divided into two groups according to regions of the river basins nearest to the place of residence, and analyzed for association between presence of clonorchiasis and cholangiocarcinoma. Rivers of the southern region of the Korean Peninsula included Nakdong, Yeongsan, Seomjin and Hyeongsan Rivers and those of the middle region included South Han, North Han, Geum, Bulyeong-Wangpi, Namdae-Yeongok-Osip, and Mangyong-Dongjin Rivers (Figure 2). Clonorchiasis was present in 189 of 560 patients (33.8%) from the southern region, but in only 48 of 560 patients (8.6%) from the middle region (P = 0.000). While cholangiocarcinoma was found in 39 of 560 patients (7.0%) from the southern region, it was found in 19 of 560 patients (3.4%) from the middle region (P = 0.007) (Figure 1B).
In both southern and middle region groups, there was a significant association between presence of clonorchiasis and cholangiocarcinoma [P = 0.005, odds ratio: 4.136 (95% CI, 1.422-12.030] and P = 0.040, odds ratio: 1.961 (95% CI, 1.020-3.773), respectively]. Even after correction for regional influence, there was a significant association between presence of clonorchiasis and cholangiocarcinoma [P = 0.003, common odds ratio: 2.289 (95% CI, 1.297-4.038)] (Table 10, Figure 1B).
| Rivers in southern region1 | Rivers in middle region2 | |||||
| With cholangiocarcinoma | Without cholangiocarcinoma | χ2(P) | With cholangiocarcinoma | Without cholangiocarcinoma | χ2(P) | |
| With clonorchiasis,n(%) | 5 (10.4) | 43 (89.6) | 7.902 (0.005) | 19 (10.1) | 170 (89.9) | 4.2 (0.04) |
| Without clonorchiasis,n(%) | 14 (2.7) | 498 (97.3) | 20 (5.4) | 351 (94.6) | ||
| Odd ratio | 4.136 (95% CI 1.422-12.030) | 1.961 (95% CI 1.020-3.773) | ||||
| Common odds ratio3 | 2.289 (95% CI 1.297-4.038) | |||||
Twenty-four of 34 patients with clonorchiasis and cholangiocarcinoma had a history of raw freshwater fish and/or shellfish ingestion. Fifteen of these patients (62.5%) had ingested raw freshwater fish and/or shellfish 30 years ago, seven patients did so within last 10 years, and the other two patients ingested raw freshwater fish and/or shellfish between 21 and 30 years ago.
In this prospective study of Korean patients who had been admitted with gastrointestinal symptoms, 37.2% had a history of ingesting raw freshwater fish and/or shellfish more than once. Many Koreans still enjoy raw freshwater fish and/or shellfish and most do so more than once in his/her lifetime.
More than 80% of the patients knew that ingesting raw freshwater fish can result in clonorchiasis and 78% answered that eating fully cooked freshwater fish can prevent clonorchiasis. However, only 50% knew that eating raw freshwater shellfish could result in clonorchiasis. About 40%-50% of the patients also knew that clonorchiasis can be transmitted through kitchen knives, towels, kitchen boards, and/or unwashed hands of the cook or handler. Many people knew the transmission route of clonorchiasis, but still enjoyed eating raw freshwater fish and/or shellfish. Perhaps, these people believed that clonorchiasis can be easily treated with oral medication and clonorchiasis will not result in serious hepatobiliary diseases.
Since the objective of this study was to evaluate the association between clonorchiasis and various hepatobiliary diseases, rather than to evaluate epidemiology of clonorchiasis in the Korean population, diagnosis of clonorchiasis was based not only on positive laboratory findings, but also on presence of peripheral intrahepatic bile duct dilatation and clonorchiasis documented in medical records. Of 3080 patients admitted with gastrointestinal symptoms, 12.9% had been diagnosed with clonorchiasis. It is apparent that clonorchiasis is still prevalent in the Korean population. In the past, epidemiological studies of clonorchiasis in Korea have been based on stool examination and/or intradermal tests[1112]. One epidemiological study in 1969 utilizing cellophane thick smear revealed that 11.6% of 3880 subjects were infected with C. sinensis[25]. Another study in 1973 using an intradermal test showed an infection rate of 21.1%[5]. In 1981, stool examination of 13 000 Koreans from seven river basins demonstrated a clonorchiasis infection rate of 21.5%. From national surveys of clonorchiasis done every 5 years since 1971, the Ministry of Health and Welfare have reported an infection rate of 1.8%-4.6% in the Korean population[2]. Although the present study enrolled patients admitted with gastrointestinal symptoms, clonorchiasis seemed still prevalent with an infection rate of 12.9%. About one out of five patients who had ingested raw freshwater fish had clonorchiasis. Also, 6.5% of those without a history of raw freshwater fish ingestion had clonorchiasis, which implied that there might be routes of infection other than ingestion of raw freshwater fish or shellfish.
In a previous study, people from river basins in southern region of the Korean Peninsula showed higher infection rates when compared to those from river basins in the middle region (17.3%-40.2% vs 8.0%-17.3%, respectively)[10]. The results of the present study were similar to those of the previous study. While 33.8% of patients from river basins in southern region were infected with clonorchiasis, only 8.3% of those from the middle region were infected.
Among various methods used to diagnose clonorchiasis in the present study, intradermal tests showed the highest sensitivity of 74.5%, followed by detection of serum antibodies using ELISA, with a sensitivity of 46.4%. These two methods are limited by cross-reactivity and low specificity. Stool examination and bile cytology for adult worms and/or eggs have high specificity, but low sensitivity of 10%-12%. Radiological findings of intrahepatic bile duct dilatation also showed low sensitivity of 11.5%. In order to increase sensitivity, more than two diagnostic studies are needed.
Eosinophilia was found in 16.7% of patients with infection, while it was found in 9.6% of patients without clonorchiasis. Mean level of serum alkaline phosphatase was 304 U/L in patients with infection and 234.4 U/L in those without clonorchiasis. When laboratory tests during admission show eosinophilia with elevated alkaline phosphatase, clonorchiasis should be considered. There was no significant difference regarding other laboratory tests such as AST, ALT, GGT, and total bilirubin. Therefore, clonorchiasis cannot be excluded by liver function test only.
Adult worms of C. sinensis attach themselves with suckers to the walls of peripheral intrahepatic bile ducts. Long-term infection with C. sinensis is associated with various hepatobiliary diseases. It has been reported that cholangiocarcinoma has originated from papillary or adenomatous hyperplasia of the bile ducts infected with C. sinensis[26]. In a recent case-control study of Korean patients, peripheral intrahepatic bile dilatation or positive serum antibodies has been a risk factor for cholangiocarcinoma[27]. In the present study, there was no association of cholangitis and bile duct stones with clonorchiasis. Even after dividing bile duct stones into intrahepatic, extrahepatic, and gallbladder stones, there was no association between bile duct stones and clonorchiasis. In the present study, in patients admitted with gastrointestinal symptoms, cholangitis and bile ducts stones were present in 9% and 26.7% of patients without clonorchiasis. This may explain the absence of association of these diseases with clonorchiasis. Neither gallstone pancreatitis nor hepatitis of various causes was associated with clonorchiasis. Also, hepatocellular carcinoma and gallbladder cancer showed no association with clonorchiasis. Similar to results of other studies[2627], cholangiocarcinoma was associated with the presence of clonorchiasis.
River basins of the southern region showed a higher infection rate of C. sinensis than those of the middle region (33.8% vs 8.6%, P = 0.000). Also, river basins of the southern region showed a higher prevalence rate of cholangiocarcinoma compared to those of the middle region (7.0% vs 3.4%, P = 0.007). The odds ratio of patients with clonorchiasis for cholangiocarcinoma was 4.136 (95% CI, 1.422-12.030) in the southern region and 1.961 (95% CI, 1.020-3.773) in the middle region. Even after correction for regional influence, the odds ratio was 2.289. According to these data, there was a strong correlation between clonorchiasis and cholangiocarcinoma. These findings were similar to the results of a previous study on the Korean population[28].
Initial ingestion of raw freshwater fish or shellfish dated back to 20 years ago in 70.8% of 24 patients with clonorchiasis and cholangiocarcinoma. Long-term infestation with C. sinensis is associated with development of cholangiocarcinoma, therefore, clonorchiasis should be treated as soon as possible when suspected. In this prospective multicenter nationwide study, prevalence of clonorchiasis and the association between clonorchiasis and hepatobiliary diseases in the Korean population were evaluated. Unlike other intestinal nematode infections, clonorchiasis is still prevalent. This seems to result from the habit of raw freshwater fish and/or shellfish ingestion. Since prevalence of clonorchiasis in river basins of the southern region was higher than other parts, there is an urgent need for public education to prevent further raw freshwater fish or shellfish ingestion. Also, the presence of clonorchiasis was associated with cholangiocarcinoma and is a risk factor for cholangiocarcinoma.
Clonorchiasis is an infection caused by the parasite C. sinensis, and has been one of the most important endemic diseases in eastern Asia. Clonorchiasis can cause a variety of gastrointestinal diseases such as bile duct obstruction, acute cholangitis, hepatolithiasis, and cholangiocarcinoma.
Important areas in the research field related to this article are development of more rapid and convenient diagnostic modalities and antihelminthic vaccines, and investigation of mechanisms by which C. sinensis causes cellular injury.
Despite public efforts and education, clonorchiasis is still present in the Korean population, and more so in certain regions of the country. Also, clonorchiasis is associated with cholangiocarcinoma and is a risk factor for cholangiocarcinoma.
To prevent clonorchiasis and cholangiocarcinoma associated with this parasite infection, there is a need for public education to prevent further raw freshwater fish or shellfish ingestion.
Acute cholangitis is inflammation of bile duct that can cause fever, abdominal pain and abnormal blood test results. Hepatolithiasis refers to stone formation inside the liver. Cholangiocarcinoma is a certain type of liver cancer that originates from bile duct.
This study showed an impressive epidemiology and way of infection of clornochiasis in riverside populations of Korea. The authors collected data from 26 hospitals in only 1 mo. This is an important contribution to the etiology of cholangiocarcionoma in this part of the world. Also, the results of this study can serve as a basis for public health initiatives for prevention and mass treatment of clonorchiasis.
| 1. | Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, Bonis P, Hassall E, Straumann A, Rothenberg ME. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342-1363. [Cited in This Article: ] |
| 2. | Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004;113:11-28; quiz 29. [Cited in This Article: ] |
| 3. | Ona FV, Dytoc JN. Clonorchis-associated cholangio-carcinoma: a report of two cases with unusual manifestations. Gastroenterology. 1991;101:831-839. [Cited in This Article: ] |
| 4. | Infection with liver flukes (Opisthorchis viverrini, Opisthorchis felineus and Clonorchis sinensis). IARC Monogr Eval Carcinog Risks Hum. 1994;61:121-175. [Cited in This Article: ] |
| 5. | Rim HJ. Clonorchiasis in Korea. Kisaengchunghak Chapchi. 1990;28 Suppl:63-78. [Cited in This Article: ] |
| 6. | Ministry of Health and Welfare and Korean Association of Health. Prevalence of intestinal parasitic infections in Korea. The sixth report. 1997;28 Suppl. [Cited in This Article: ] |
| 7. | Kim SS, Han MH, Park SG, Lim HS, Hong ST. [A survey on the epidemiological factors of clonorchiasis in the Pohang industrial belt along the Hyungsan river, Kyongsangbuk-do]. Kisaengchunghak Chapchi. 1990;28:213-219. [Cited in This Article: ] |
| 8. | Min DY, Ahn MH, Kim KM, Kim CW. [Intestinal parasite survey in Seoul by stool examination at Hanyang University Hospital]. Kisaengchunghak Chapchi. 1986;24:209-212. [Cited in This Article: ] |
| 9. | Choi BI, Park JH, Kim YI, Yu ES, Kim SH, Kim WH, Kim CY, Han MC. Peripheral cholangiocarcinoma and clonorchiasis: CT findings. Radiology. 1988;169:149-153. [Cited in This Article: ] |
| 10. | Seo BS, Lee SH, Cho SY, Chai JY, Hong ST, Han IS, Sohn JS, Cho BH, Ahn SR, Lee SK. An Epidemiologic Study On Clonorchiasis And Metagonimiasis In Riverside Areas In Korea. Kisaengchunghak Chapchi. 1981;19:137-150. [Cited in This Article: ] |
| 11. | Choi MH, Ge T, Yuan S, Hong ST. Correlation of egg counts of Clonorchis sinensis by three methods of fecal examination. Korean J Parasitol. 2005;43:115-117. [Cited in This Article: ] |
| 12. | Shin BM, Choi KI. Diagnostic significance of intradermal test compared with radiologic findings for clonorchiasis. Korean J Clin Pathol. 2000;20:81-86. [Cited in This Article: ] |
| 13. | Kim SI. A Clonorchis sinensis-specific antigen that detects active human clonorchiasis. Korean J Parasitol. 1998;36:37-45. [Cited in This Article: ] |
| 14. | Choi BI, Han JK, Hong ST, Lee KH. Clonorchiasis and cholangiocarcinoma: etiologic relationship and imaging diagnosis. Clin Microbiol Rev. 2004;17:540-552, table of contents. [Cited in This Article: ] |
| 15. | Hou PC. The pathology of Clonorchis sinensis infestation of the liver. J Pathol Bacteriol. 1955;70:53-64. [Cited in This Article: ] |
| 16. | Lim JH. Oriental cholangiohepatitis: pathologic, clinical, and radiologic features. AJR Am J Roentgenol. 1991;157:1-8. [Cited in This Article: ] |
| 17. | Huang MH, Chen CH, Yen CM, Yang JC, Yang CC, Yeh YH, Chou DA, Yueh SK, Yang YY, Nien CK. Relation of hepatolithiasis to helminthic infestation. J Gastroenterol Hepatol. 2005;20:141-146. [Cited in This Article: ] |
| 18. | Kubo S, Kinoshita H, Hirohashi K, Hamba H. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995;19:637-641. [Cited in This Article: ] |
| 19. | Hou PC. The relationship between primary carcinoma of the liver and infestation with Clonorchis sinensis. J Pathol Bacteriol. 1956;72:239-246. [Cited in This Article: ] |
| 20. | Belamaric J. Intrahepatic bile duct carcinoma and C. sinensis infection in Hong Kong. Cancer. 1973;31:468-473. [Cited in This Article: ] |
| 21. | Chung CS, Lee SK. An epidemiological study of primary liver carcinomas in pusan area with special reference to clonorchiasis. Korean J Pathol. 1976;10:33-64. [Cited in This Article: ] |
| 22. | Choi BI, Han JK. Other parasitic diseases. Hepatobiliary disease pathophysiology and imaging. Blackwell Science: London 2001; 579-581. [Cited in This Article: ] |
| 23. | Callea F, Sergi C, Fabbretti G, Brisigotti M, Cozzutto C, Medicina D. Precancerous lesions of the biliary tree. J Surg Oncol Suppl. 1993;3:131-133. [Cited in This Article: ] |
| 24. | Teoh TB. A study of gall-stones and included worms in recurrent pyogenic cholangitis. J Pathol Bacteriol. 1963;86:123-129. [Cited in This Article: ] |
| 25. | Seo BS, Rim HJ, Loh IK, Lee SH, Cho SY, Park SC, Bae JW, Kim JH, Lee JS, Koo BY. [Study On The Status Of Helminthic Infections In Koreans]. Kisaengchunghak Chapchi. 1969;7:53-70. [Cited in This Article: ] |
| 26. | Lee JH, Yang HM, Bak UB, Rim HJ. Promoting role of Clonorchis sinensis infection on induction of cholangiocarcinoma during two-step carcinogenesis. Korean J Parasitol. 1994;32:13-18. [Cited in This Article: ] |
| 27. | Choi D, Lim JH, Lee KT, Lee JK, Choi SH, Heo JS, Jang KT, Lee NY, Kim S, Hong ST. Cholangiocarcinoma and Clonorchis sinensis infection: a case-control study in Korea. J Hepatol. 2006;44:1066-1073. [Cited in This Article: ] |
| 28. | Lim MK, Ju YH, Franceschi S, Oh JK, Kong HJ, Hwang SS, Park SK, Cho SI, Sohn WM, Kim DI. Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg. 2006;75:93-96. [Cited in This Article: ] |